Penpulimab, also known by its generic name penpulimab-kcqx, is a newly FDA-approved immunotherapy for certain types of nasopharyngeal carcinoma (NPC). It belongs to a class of drugs known as immune checkpoint inhibitors and is designed to help the body’s immune system better recognize and fight cancer. As of April 2025, the U.S. Food and Drug Administration (FDA) approved penpulimab for both first-line and subsequent-line treatment of non-keratinizing NPC, offering new hope to patients facing this challenging disease.
What Is Penpulimab and How Does It Work?
Penpulimab is developed together by two companies: Akeso, Inc., and Chia Tai Tianqing, which is part of the larger Sino Biopharmaceutical group.It is a humanized monoclonal antibody that targets PD-1 (programmed death-1), a protein on immune cells that acts as a brake to prevent them from attacking other cells—including cancer cells. Many tumors use this PD-1 pathway to escape immune detection.
By blocking PD-1, penpulimab helps reactivate T cells, allowing them to identify and destroy cancer cells. Unlike other PD-1 inhibitors that are IgG4-based, penpulimab is engineered as an Fc-null IgG1 antibody, which reduces unwanted immune-related side effects while maintaining strong antitumor activity.

Photo from akesobio.com
What Cancers Does Penpulimab Treat?
Penpulimab is approved for:
- Recurrent or metastatic non-keratinizing NPC (nasopharyngeal carcinoma) in combination with chemotherapy (first-line).
- Metastatic non-keratinizing NPC as a monotherapy after platinum-based chemotherapy and at least one additional treatment.
It is also approved in China for:
- Classic Hodgkin’s lymphoma (cHL) – after two or more systemic treatments.
- Squamous non-small cell lung cancer (sq-NSCLC) – as a first-line therapy with chemotherapy.
- Advanced nasopharyngeal cancer – as a first option with chemotherapy.
These approvals make penpulimab an important tool in treating cancers that are often difficult to manage.
You can read about Immunotherapy for Cancer: An Overview on OncoDaily.
Efficacy and Results from Clinical Trials
Penpulimab, an Fc-engineered anti-PD-1 antibody, is being studied as both a first-line and later-line treatment for recurrent or metastatic nasopharyngeal carcinoma (NPC). Early trials show it may improve progression-free survival and offer lasting responses.
First-Line NPC (AK105-304 Trial)
In the Phase III AK105-304 trial involving 291 patients with recurrent or metastatic NPC, penpulimab combined with chemotherapy significantly improved progression-free survival (PFS):
- Median PFS: 9.6 months (penpulimab) vs. 7.0 months (placebo)
- 12-month PFS rates: 31% (penpulimab) vs. 11% (placebo)
- Hazard Ratio: 0.45 (p < 0.0001)
Subsequent-Line NPC (AK105-202 Trial)
The Phase II AK105-202 study focused on patients with advanced NPC who had failed prior therapies:
- Objective Response Rate (ORR): 28%
- Duration of Response (DOR): Not yet reached, with some patients showing lasting benefit beyond 9 months
These results confirmed penpulimab’s meaningful antitumor activity even in heavily pretreated patients.
Learn more about Nasopharyngeal Cancer: What patients should know on OncoDaily.
What Is a Clinical Trial and Why Does It Matter?
A clinical trial is a research study designed to test new drugs and treatments in patients to determine their safety and effectiveness. Before Penpulimab was approved, it went through multiple phases of clinical trials to assess how well it worked, what side effects it caused, and whether it was better than existing treatments. Clinical trials are essential because they provide scientific evidence that a drug can help patients while ensuring it is safe for widespread use.
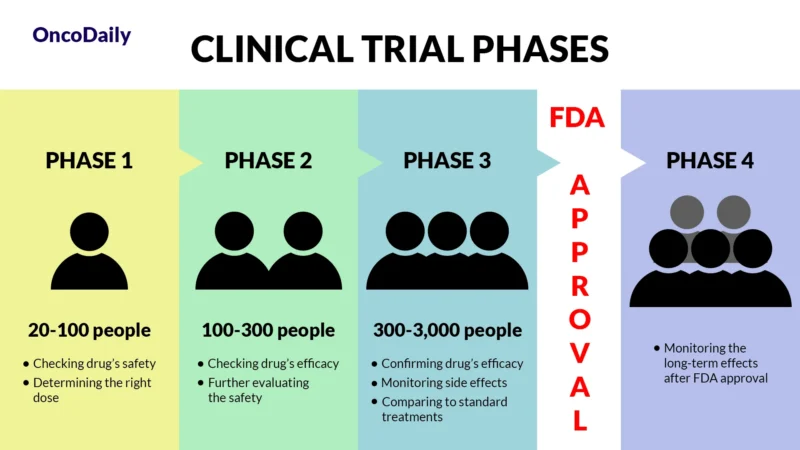
What Does FDA Approval Mean?
When a drug receives FDA approval, it means that after rigorous testing in clinical trials, it has been shown to be both safe and effective for treating a specific condition. This approval makes the drug widely available for doctors to prescribe and helps patients access new, cutting-edge treatments sooner.
What Other Trials Are Ongoing?
Penpulimab is currently being evaluated in several clinical trials for its potential to treat various advanced cancers. These studies aim to assess its safety and effectiveness, both alone and in combination with other treatments.
One such trial, identified as NCT06821503, is exploring the combination of penpulimab with LM-108, albumin-bound paclitaxel, and gemcitabine in patients with advanced pancreatic cancer. The initial phase determined the appropriate dosing, and the ongoing phase is focusing on the treatment’s safety and effectiveness.
Another study, NCT06586242, is investigating the use of penpulimab alongside anlotinib and chemotherapy in patients with locally advanced, operable esophageal cancer. This trial compares two groups receiving different chemotherapy agents—oxaliplatin or lobaplatin—combined with penpulimab, anlotinib, and albumin-bound paclitaxel, to determine the most effective treatment regimen.
These ongoing trials are part of the broader effort to find more effective treatments for challenging cancers, offering hope for improved patient outcomes in the future.
What Can Patients Expect During Treatment?
Penpulimab is administered as an intravenous (IV) infusion. Depending on the treatment plan:
- Monotherapy dose: 200 mg IV every 2 weeks
- Combination therapy dose: 200 mg IV every 3 weeks alongside gemcitabine and cisplatin or carboplatin
Infusions typically take about 60 minutes and may include premedication to reduce side effects. Treatment may continue for up to 24 months, or until cancer progresses or side effects become unmanageable.
Penpulimab Side Effects and Their Management
While Penpulimab offers real hope for people with certain cancers, like nasopharyngeal carcinoma, it can also cause side effects—just like many powerful cancer treatments. These may be mild and manageable, or more serious in some cases. Knowing what to expect and how doctors manage these side effects can help patients feel more prepared and supported throughout treatment.
Common Side Effects
Many people taking Penpulimab may experience mild to moderate side effects that are quite common. These can include changes in blood test results, such as higher levels of creatinine that might affect how well the kidneys work. Levels of important minerals and proteins in the blood—like phosphate, sodium, albumin, and hemoglobin—may go down slightly. Liver enzymes such as AST and ALT can also rise, so doctors monitor liver function closely with regular tests.
Some people may notice hormone changes, especially in the thyroid gland. A common issue is low thyroid hormone (called hypothyroidism), which can lead to symptoms like tiredness, feeling cold, or gaining weight. In many cases, this happens because the immune system affects the thyroid.
Penpulimab may also affect metabolism, sometimes leading to higher blood sugar or triglyceride levels. Other common symptoms include muscle or joint pain, low-grade fever, tiredness, mild cough or rash, and minor infections like a sore throat or cold. These effects are typically short-lived and can often be treated with medications, changes to the treatment schedule, or supportive care. Regular monitoring through blood tests helps catch and manage these changes early.
Less Common and Serious Side Effects
In rare cases, Penpulimab can cause more serious side effects that need quick medical attention. Sometimes the immune system becomes too active and starts attacking healthy parts of the body. This can affect the lungs, causing coughing or trouble breathing; the colon, leading to diarrhea or stomach pain; the liver, which may result in tiredness or yellowing of the skin; and the thyroid, which in some cases becomes overactive, causing symptoms like anxiety, weight loss, or a fast heartbeat.
There is also a small risk of serious skin reactions such as Stevens-Johnson Syndrome or Toxic Epidermal Necrolysis, which cause painful rashes and require emergency treatment. The nervous system can be affected too, with rare cases of Guillain-Barré syndrome, myasthenia gravis, or brain inflammation, which may lead to muscle weakness, numbness, or confusion.
Other serious conditions that may occur include inflammation of the heart (myocarditis), kidneys (nephritis), or reactions during the infusion—such as chills, a drop in blood pressure, or a rash that appears during or shortly after treatment.
How to Manage Side Effects?
Doctors take a proactive approach to managing side effects from Penpulimab. Patients will have regular check-ups and blood tests to monitor thyroid, liver, kidney, and immune function.
If a more serious side effect appears, the first step is usually to pause Penpulimab and start medications like steroids (such as prednisone). These help calm the immune system and reduce inflammation. Once the patient improves, the drug may be resumed—or permanently stopped if needed.
In some cases, supportive care is also important:
- Hormone replacement therapy may be needed if the thyroid is affected
- IV fluids, fever reducers, or antihistamines may be used for infusion-related side effects
The key is early recognition. Patients are encouraged to tell their care team right away if they feel unwell, notice new symptoms, or something just doesn’t feel right. Catching side effects early often means they can be managed effectively, and many patients are able to continue treatment safely.
Recommended Dose of Penpulimab
Penpulimab is usually given at a dose of 200 mg through an IV. If used alone—for example, in patients with advanced nasopharyngeal carcinoma who have already received other treatments—it is given every two weeks. When used with chemotherapy as a first treatment for recurrent or metastatic disease, it’s given every three weeks alongside gemcitabine and a platinum-based drug. After the chemotherapy part is done, Penpulimab may be continued by itself for up to 24 months, or until the cancer worsens or side effects become unmanageable.
If serious side effects occur, your doctor may temporarily pause or permanently stop the treatment. Immune-related side effects are usually treated with corticosteroids, and close monitoring helps guide these decisions.
How Penpulimab Is Administered?
Penpulimab is given as an intravenous (IV) infusion, meaning it goes directly into a vein over about 60 minutes. The medication is carefully prepared by mixing it with a sterile saline solution. It must look clear or slightly yellow—if it’s cloudy or has particles, it won’t be used.
Once diluted, the solution must be used within 4 hours. During treatment with other drugs, Penpulimab is always given first, followed by chemotherapy medications. It is never mixed with other drugs in the same IV line.
The unopened medication is stored in a refrigerator and protected from light. After preparation, it’s either kept at room temperature or in the fridge, but must be used within a few hours.
What to Expect Long-Term?
Penpulimab is not a cure, but it can provide long-term disease control for many patients. In trials, some patients continued responding to treatment for many months or longer, especially in combination with chemotherapy. If cancer progresses, doctors may suggest switching therapies.
You can read about Radiotherapy for Head And Neck Cancer: Types, Success Rate, Side Effects on OncoDaily.
Real-Life Effectiveness
Beyond trials, penpulimab has shown promise in real-world use, with many patients tolerating it well and benefiting from disease control. As more data becomes available, expectations for long-term use and effectiveness will become clearer.
Looking Ahead – The Future of Treatment
Penpulimab is a key part of Akeso’s growing cancer pipeline. With its unique design and promising results, ongoing studies may expand its use to more cancers and new combinations. Researchers are especially interested in how it can be combined with other immunotherapies to improve survival.
Penpulimab represents a new generation of immunotherapy, offering renewed hope to people with nasopharyngeal carcinoma and other hard-to-treat cancers. Patients starting this therapy should feel supported knowing that it is backed by strong research, manageable side effects, and a clear commitment to better outcomes.
You can read about Kim Woo-bin and Nasopharyngeal Cancer: How He Went Against, How He Survived on OncoDaily.
If you’re a healthcare provider, access the professional version here.