Radiotherapy for Head and Neck Cancer is a key treatment approach for this common group of cancers. Often used alone, or in combination with surgery and/or chemotherapy, it plays a vital role in managing the disease. The primary goal is to achieve control over the tumor within the head and neck region while carefully limiting the radiation dose to nearby healthy tissues. While complex, especially with modern techniques, radiotherapy is a significant factor in the success rates for many head and neck cancers, though patients may experience various acute and late side effects as a result of the treatment.
What is Radiotherapy for Head And Neck Cancer?
Radiotherapy is defined as a treatment method in cancer care that utilizes ionized radiation. This treatment works by directing high-voltage x-ray beams to damage the genetic material, or DNA, within Head and Neck Cancer cells. This damage prevents the cells from dividing and proliferating. The process of ionization also leads to the creation of free oxygen radicals, which further contribute to the death of cancer cells.
Radiotherapy for head and neck cancer is employed with different objectives. It can be used with a curative intent, aiming to eliminate the cancer entirely, sometimes even as an alternative to surgery for early-stage disease, or alongside chemotherapy to preserve organs. It may also be used in an adjuvant setting, administered after an initial treatment like surgery to target and eliminate any remaining microscopic cancer cells that could cause recurrence. Additionally, radiotherapy can be palliative, delivered to help reduce symptoms and improve comfort in cases where the cancer is not curable, often using a shorter treatment course, although for symptom relief in head and neck cancers, the dose might resemble a curative plan in some situations.
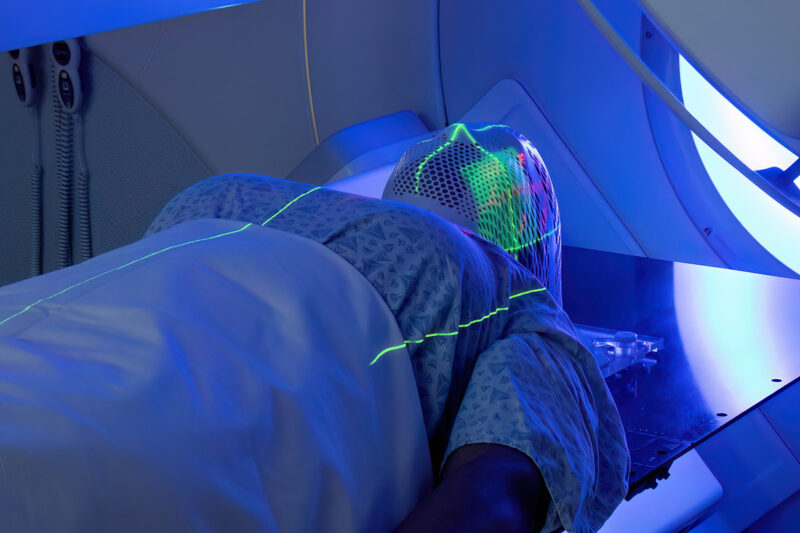
Patient receiving head and neck radiotherapy
source: www.winshipcancer.emory.edu
Types of Radiotherapy for Head And Neck Cancer
There are several types of radiotherapy for head and neck cancer, employing different techniques to target cancer cells while aiming to protect healthy tissues. Some of the main approaches include external beam methods, highly focused techniques, and those using a different type of particle beam.
External Beam Radiation Therapy (EBRT)
External beam therapy involves delivering a beam of high-energy x-rays or protons from a machine outside the body, directed at the tumor site. This type of treatment aims to destroy cancer cells using radiation beams that are generated and targeted at the tumor.
Stereotactic Body Radiotherapy (SBRT)
SBRT is a technique that combines image guidance with advanced technology to deliver extremely high doses of radiation directly to a tumor. It is designed to minimize the radiation dose received by nearby healthy tissues. This approach often requires fewer treatment sessions compared to other forms of radiation therapy and can potentially lead to better outcomes and fewer side effects, although it is not suitable for all patients.
Proton Therapy
Proton therapy is a type of radiation that uses proton beams instead of the more common photon (x-ray) beams. A key characteristic is that protons do not penetrate beyond the tumor, allowing the beam energy to be precisely aimed at a specific depth where the tumor is located. This reduces the dose to normal tissues located behind the tumor compared to photon therapy, where the dose may continue beyond the target.
This can potentially lead to fewer side effects, allowing for higher doses to be delivered to the tumor to maximize destruction. Proton therapy can be very helpful for many individuals and is often used for head and neck cancer that has returned after previous treatment, particularly when the cancer is close to sensitive, critical structures.
For patients with early-stage head and neck cancers, radiotherapy alone can be highly effective, sometimes achieving a high likelihood of cure comparable to surgery and potentially replacing the need for surgical removal, such as for certain early laryngeal or nasal vestibule cancers where it helps avoid deformity.
In more advanced cases, radiotherapy is often used in combination with other treatments. Surgery followed by radiotherapy is frequently recommended, as surgery addresses the main tumor mass while radiotherapy targets any microscopic spread that could lead to recurrence. The combination of chemotherapy given concurrently with radiotherapy has been shown to increase tumor control and preserve organs, with meta-analyses indicating an increased 5-year survival rate compared to radiotherapy alone for locally advanced cancers.
How Effective is Radiotherapy for Head and Neck Cancer?
Based on the provided texts, when considering how effective is radiotherapy for head and neck cancer, its success varies depending on factors like the cancer’s primary location and stage. Radiotherapy is a major treatment, beneficial for a significant portion of patients, whether used as the initial primary treatment or as additional therapy after surgery.
For patients with early-stage head and neck cancers, radiotherapy alone can be highly effective, sometimes achieving a high likelihood of cure comparable to surgery and potentially replacing the need for surgical removal, such as for certain early laryngeal or nasal vestibule cancers where it helps avoid deformity.
In more advanced cases, radiotherapy is often used in combination with other treatments. Surgery followed by radiotherapy is frequently recommended, as surgery addresses the main tumor mass while radiotherapy targets any microscopic spread that could lead to recurrence. The combination of chemotherapy given concurrently with radiotherapy has been shown to increase tumor control and preserve organs, with meta-analyses indicating an increased 5-year survival rate compared to radiotherapy alone for locally advanced cancers.
What Are the Side Effects of Radiotherapy for Head and Neck Cancer?
When considering the side effects of radiotherapy for head and neck cancer, patients may experience a range of reactions appearing at different times. Understanding what are the side effects of radiotherapy for head and neck cancer involves distinguishing between effects that emerge during or shortly after treatment and those that might manifest months or years later.
Short-Term Side Effects
These effects typically appear within the first few weeks of starting radiation treatment and generally improve over the weeks to months following the completion of therapy. Common examples include skin changes in the treated area resembling a sunburn (dermatitis), soreness and pain in the mouth and throat, including mucositis (inflammation of the mouth and throat lining), difficulty or pain when swallowing (dysphagia and odynophagia), changes in taste sensation, dryness of the mouth (xerostomia), and hoarseness or alterations in voice.
Fatigue, a feeling of tiredness or weakness, is also a very common short-term side effect. Other effects can involve thicker saliva, changes inside the nose such as dryness, temporary ear pain due to swelling, and temporary hair loss in the treated area. Nausea can also occur in some patients.
Long-Term Side effects
Long-term side effects can develop several months or even years after radiation treatment has finished. Some of these effects may be permanent. Potential late effects include persistent dry mouth (xerostomia), hardening of tissues beneath the skin (subcutaneous fibrosis), limited ability to open the mouth (trismus), ongoing swallowing difficulties, alterations in voice quality, potential thyroid gland dysfunction, and sensorineural hearing loss if the ear was in the treatment field. More serious, though less frequent, late complications can include the breakdown of bone tissue (osteoradionecrosis) or narrowing of the throat (pharyngeal or oropharyngeal stenosis).
A 2008 retrospective case series by Stubblefield et al., published in Archives of Physical Medicine and Rehabilitation, explored botulinum toxin type A (BTX-A) for radiation fibrosis syndrome (RFS). The study of 23 patients found BTX-A injections were indicated for issues like cervical dystonia, neuralgia, trismus, and migraine, with 87% of patients reporting benefit. The authors concluded that initial experience is encouraging but further prospective studies are needed.
How is Radiotherapy for Head And Neck Administered?
Based on the texts provided, administering radiotherapy for head and neck cancer follows a structured process. It typically begins after consultation with your healthcare team, where treatment options are decided.
A crucial step is the simulation, a planning appointment that can take several hours. During this session, a custom mask is created to keep your head and neck perfectly still for treatment, and imaging scans like a CT scan, potentially combined with MRI or PET, are performed while you wear the mask and are in the treatment position. These images precisely map the area to be treated. Small, permanent tattoo dots are also placed on your skin to help align you for each daily session.
Following the simulation, a team of specialists uses the planning images to design your specific treatment plan, a process that takes about one to two weeks. Just before your first treatment, a brief set-up procedure verifies your position using special X-rays to ensure accuracy.
Daily treatment sessions usually occur five days a week for roughly five to seven weeks. For each session, you are positioned on the treatment table using your mask. Radiographers ensure correct alignment before leaving the room to deliver the radiation. While you are alone during the short treatment delivery (which you won’t see or feel, though you may hear the machine), you are continuously monitored via camera and intercom. Daily imaging is often done right before treatment to confirm accurate positioning. You also have regular checks with your care team throughout the treatment course to manage any side effects.
After completing the treatment, side effects may persist for a week or so before gradually improving. Post-treatment care involves follow-up appointments with your healthcare team, typically starting about a week later, for ongoing monitoring and management of any lingering or late side effects.
Radiotherapy Mask for Head And Neck Cancer: Why is it Used?
Radiotherapy mask is used for Head and Neck Cancer treatment primarily to ensure that you are positioned in the exact same way for every single treatment session. This custom-fitted device, often made from a plastic mesh that hardens, covers your face and upper body and attaches to the treatment table.
The main reason for using the mask is to help you remain still and limit the movement of your head, jaw, and shoulders during both the simulation and each daily radiation treatment. Maintaining this precise and consistent position is crucial because it allows the healthcare team to accurately align the radiation beams to the planned target volume, ensuring the cancer receives the intended dose while minimizing exposure to nearby healthy tissues. Essentially, the mask is a vital tool for achieving the high level of accuracy required for effective and safe radiation delivery.

Read OncoDaily’s Special Article About Radiotherapy Mask
What Happens After Radiotherapy for Head And Neck Cancer?
After completing treatment, patients often wonder what happens after radiotherapy for head and neck cancer. The period immediately following the last session involves side effects potentially peaking for about a week before gradually starting to improve. During this time, you maintain access to your healthcare team and receive aftercare advice.
A key part of post-treatment care is scheduled follow-up, beginning with an appointment with your clinical oncologist typically around one week after treatment ends. Following this, you will have regular monitoring visits with the head and neck healthcare team over time. These appointments serve several crucial purposes: to check for any sign that the cancer might be returning (potential recurrence), to manage any side effects that linger or develop later on, and to screen for the possibility of new, unrelated head and neck cancers developing.
Follow-up monitoring often includes continued imaging, such as CT scans, or sometimes MRI or PET scans, to assess how well the treatment worked and to detect any recurrence. If recurrent cancer is found, the team will discuss further treatment possibilities, which could include surgery. Other monitoring might involve dental exams and annual checks of thyroid function.
While specific post-treatment “lifestyle changes” are not detailed as a formal protocol in the texts, it is understood that maintaining good oral hygiene and using fluoride treatments permanently after radiotherapy is important to minimize risks like dental caries. Avoiding smoking, emphasized heavily during treatment due to its negative impacts on healing and treatment effectiveness, remains a beneficial health practice afterward. Your healthcare team will provide guidance tailored to your recovery needs.
What Are the Costs of Radiotherapy for Head and Neck Cancer?
The overall cost for a course of radiotherapy for head and neck cancer can vary significantly based on several factors. These include the geographical location where treatment is received (country, state, or city), the specific hospital or clinic, the type of radiation technology used (such as standard External Beam RT, IMRT, SBRT, or Proton Therapy, with newer or more complex technologies often having higher costs), the total number of treatment sessions required, and the specific dose being delivered.
Costs typically encompass not just the use of the specialized equipment and the delivery of the radiation, but also the extensive pre-treatment planning process, imaging scans (like CT, MRI, PET), professional fees for the entire medical team involved (radiation oncologists, physicists, dosimetrists, therapists), and potentially costs associated with managing side effects or related procedures like the placement of a feeding tube.
How Does Radiotherapy Compare to Other Treatments for Head And Neck Cancer?
Radiotherapy is a primary treatment for head and neck cancer, often used in conjunction with other modalities like surgery and chemotherapy within a multidisciplinary care framework. A 2025 meta-analysis by Zeng, Wang et al., published in Clinical Oncology journal, investigated chemoradiotherapy (ChemoRT) versus radiotherapy (RT) alone for certain stages (T2N0M0, T1-2N1M0, T3N0M0) of nasopharyngeal cancer, questioning current guidelines. Analyzing over 5,000 patients, results showed progression-free survival was higher with ChemoRT (HR = 0.60, P = 0.0007), but overall survival showed no difference between groups (HR = 0.83, P = 0.37). Locoregional control (P=0.22) and distant metastasis risks (P=0.13) also did not differ significantly. Importantly, chemotherapy improved outcomes only in patients treated with 2DCRT, not with IMRT.
Surgery
Surgery serves as a major treatment method, sometimes used alone, particularly for certain early-stage cancers, where it can be an effective alternative to radiotherapy. For early lesions, the decision between surgery and radiotherapy might consider factors such as the tumor site and the expected impact on function and appearance; radiotherapy may be favored for better preservation of these aspects in some areas, while surgery might be chosen for faster tumor removal or potentially fewer initial dental and salivary issues.
However, for most locally advanced head and neck cancers, surgery and postoperative radiotherapy are complementary. Surgery is used to remove the main bulk of the tumor, addressing the primary source of potential treatment failure, while radiotherapy is then administered to sterilize any microscopic cancer cells left behind beyond the surgical margins, which are a major cause of recurrence.
Chemotherapy
Chemotherapy is frequently incorporated into the treatment plan, often used as an additional therapy alongside radiotherapy. For advanced head and neck cancers, chemotherapy is commonly given concurrently with radiation. This combined approach, known as chemoradiotherapy, has been shown to enhance tumor control and aid in preserving organs. Research indicates that concurrent chemoradiotherapy can lead to a significant increase in survival rates compared to radiotherapy alone for locoregionally advanced squamous cell carcinomas. Chemotherapy contributes to this by increasing the sensitivity of cancer cells to the effects of radiation. Combinations of radiotherapy and chemotherapy are also employed for cancers that cannot be surgically removed or as part of specific treatment strategies aimed at preserving organ function, such as the larynx.
A study by Yoshida et al., published in Cancer in 2020, analyzed the use of concurrent chemotherapy with definitive radiotherapy for AJCC 8th edition clinical stage I HPV-positive oropharyngeal cancer. They found concurrent chemotherapy was associated with improved overall survival (HR, 0.782; 95% CI, 0.645-0.948 [P = .012]). However, this benefit was specific to patients with lymph node-positive stage I disease (HR, 0.682; 95% CI, 0.557-0.835 [P < .001]), showing no survival improvement for those with lymph node-negative (N0) disease (HR, 1.646; 95% CI, 1.011-2.681 [P = .05]). This suggests treatment decisions for these patients may need to differ based on lymph node status
What Are The Recent Advances in Radiotherapy for Head And Neck Cancer?
Patients can actively support their health throughout head and neck radiotherapy by focusing on several key areas. Maintaining good nutrition and hydration is crucial; it helps manage weight, which is important for accurate treatment delivery, and ensures the body gets enough calories, protein, and fluids for strength and recovery. Working with a dietitian for advice on eating and potentially using nutritional supplements or a feeding tube if needed are ways to achieve this. Staying well-hydrated is also vital, often by sipping liquids frequently.
Patients should also prioritize managing treatment side effects. This involves listening to the body, especially regarding fatigue, and balancing rest with activity, while planning daily routines around appointments. Promptly reporting any side effects or pain to the healthcare team is essential for getting appropriate management and medication. Following specific guidance for issues like oral hygiene, skin care in the treated area, and dietary adjustments for swallowing difficulties or nausea is a significant part of self-care during therapy.
Avoiding irritants is highly recommended; texts emphasize the importance of not smoking or drinking alcohol, particularly spirits, during treatment, as these can worsen side effects and hinder healing. Attending all scheduled treatment appointments without interruption is also important for the therapy’s effectiveness. Lastly, open communication with the healthcare team about any concerns or issues helps ensure patients receive the necessary support throughout their treatment course.
Written By Aren Karapetyan, MD