Olubukola Ayodele, Consultant Medical Oncologist at the University Hospitals of Leicester NHS Trust and Breast Cancer Clinical Trials Lead at Leicester Cancer Research Centre, shared a post on LinkedIn:
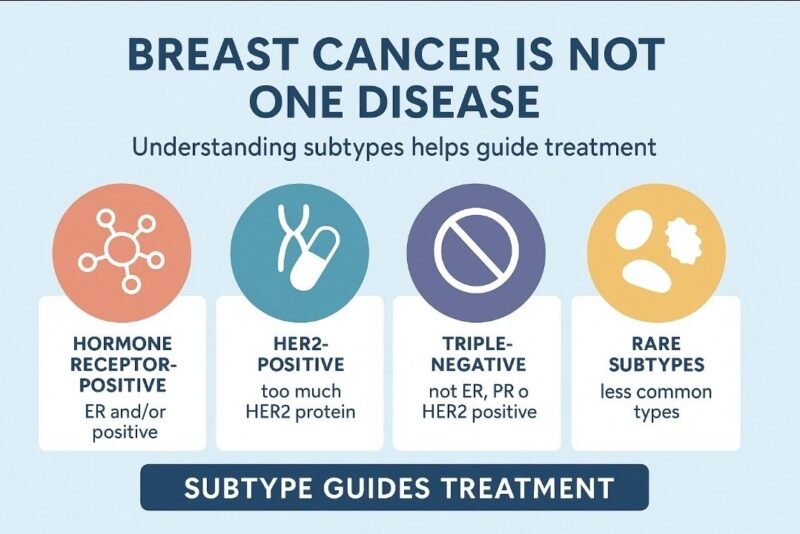
“When people hear the words “breast cancer”, they often think of it as a single illness with a single treatment path. But as a breast oncologist, I can tell you that breast cancer is not one disease. In fact, it’s a group of biologically diverse subtypes, each with its own behaviour, risks, and response to treatment.
Understanding this complexity is crucial, not just for clinicians, but for the public, patients, and policymakers too.
So, what are the main subtypes of breast cancer?
1. Hormone Receptor Positive (ER+/PR+):
This is the most common subtype. These cancers grow in response to hormones like oestrogen or progesterone. They can be slower-growing and can be treated with hormone-blocking therapies.
2. HER2-Positive:
These cancers produce too much of the HER2 protein, which promotes cancer cell growth. They used to have a poor prognosis, but targeted therapies like trastuzumab have significantly improved outcomes.
3. Triple-Negative Breast Cancer (TNBC):
These do not express oestrogen, progesterone, or HER2. TNBC is more aggressive, more common in younger women and women of African/ Caribbean descent, and doesn’t respond to hormone or HER2-targeted therapies. Chemotherapy remains the mainstay sometimes with the addition of immunotherapy but research into newer agents is evolving rapidly.
Why does this matter?
Because subtype guides treatment. It influences:
– The type of surgery and need for chemotherapy
– Whether hormone or targeted therapies will be effective
– The length of treatment and follow-up
– Prognosis and risk of recurrence
This is why a “one-size-fits-all” approach to breast cancer is outdated. Personalised medicine, guided by biology, not just stage offers the best chance for optimal outcomes.
As patients, families, and advocates, it’s important to know:
– The name of the subtype
– Why a certain treatment is recommended (or not)
– That more treatment doesn’t always mean better outcome; it must be appropriate for the biology
In breast cancer care, knowledge truly is power. And for clinicians, the responsibility lies in making this complexity understandable and empowering for every patient.
Let’s continue to increase the awareness that breast cancer is not just one disease, and every woman and man deserves care that is as unique as their diagnosis.”
More posts featuring Olubukola Ayodele.


