Brain tumors are complex and often intimidating diagnoses, both for patients and their healthcare providers. Among the various treatment options available, chemotherapy plays a crucial role, especially in combination with surgery and radiation therapy. Chemotherapy aims to kill cancer cells, slow tumor growth, and provide relief from symptoms. However, many patients wonder: How effective is chemotherapy for brain tumors? What is the brain tumor chemotherapy success rate?
The answer depends on several factors, including tumor type, location, size, and whether the tumor has spread. This article aims to explore the brain cancer chemotherapy success rate, discuss the factors influencing outcomes, and offer guidance on what patients can expect throughout their treatment journey.
Read About Brain Cancer on OncoDaily
Understanding Chemotherapy and Its Role in Brain Tumor Treatment
Chemotherapy for brain tumors typically involves the use of drugs that kill fast-growing cells, a hallmark of cancer. These drugs can be administered orally, intravenously, or directly into the cerebrospinal fluid (CSF) that surrounds the brain. Chemotherapy can be used alone, though it is more commonly part of a multimodal approach—combining surgery, radiation, and chemotherapy to treat tumors from multiple angles.
Brain tumors are categorized into primary and metastatic types. Primary brain tumors originate in the brain, while metastatic tumors spread from other body parts. The most common primary brain tumors in adults are gliomas, including glioblastomas, which are aggressive and difficult to treat. Chemotherapy’s success varies significantly based on the tumor’s grade, type, and location (Stupp et al., 2005; Jakola et al., 2012).
Chemotherapy Success Rate by Tumor Type
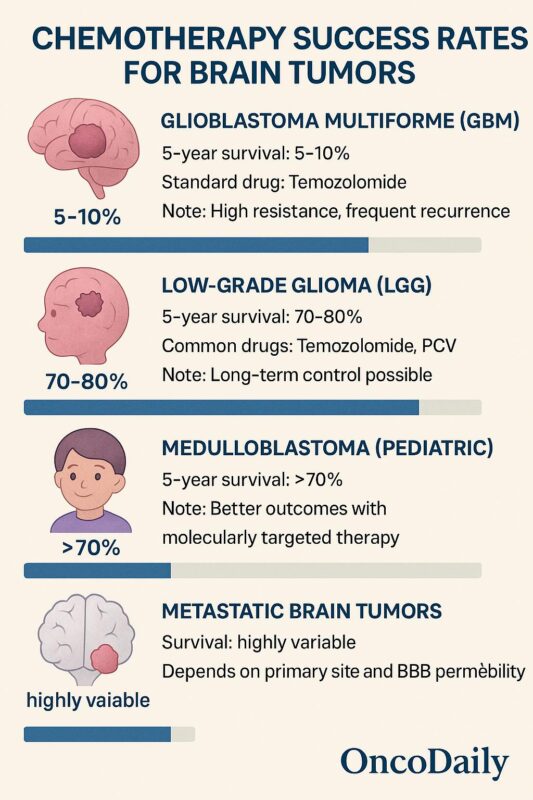
Glioblastoma Multiforme (GBM): Glioblastoma multiforme is the most common and aggressive type of malignant brain tumor. Unfortunately, GBM has a low chemotherapy success rate, and patients often face recurrence despite treatment. The standard chemotherapy regimen for GBM is temozolomide (TMZ), often used alongside radiation in the adjuvant setting after surgery.
The median survival rate for patients with GBM, even with chemotherapy, is typically 12–15 months, with 5-year survival rates of around 5–10% (Stupp et al., 2005). While chemotherapy extends survival, the tumor’s ability to become resistant to TMZ is a significant challenge.
Read About Glioblastoma on OncoDaily
Low-Grade Gliomas (LGG): In contrast, low-grade gliomas (which are less aggressive) can have better chemotherapy outcomes. These tumors may respond well to chemotherapy regimens like temozolomide and procarbazine. When treated early with a combination of surgery and chemotherapy, patients can achieve longer progression-free survival.
For patients with low-grade gliomas, 5-year survival rates can exceed 70–80% depending on tumor grade, location, and molecular markers (Jakola et al., 2012). The introduction of chemotherapy as part of an aggressive treatment plan has led to improved survival rates.
Medulloblastoma: Medulloblastoma, a common pediatric brain tumor, can also be treated with chemotherapy, typically following surgery and radiation therapy. Chemotherapy for medulloblastoma has been shown to significantly improve survival outcomes. For children, the 5-year survival rate with appropriate chemotherapy and radiation can exceed 70%, though survival rates can vary depending on the tumor’s molecular subtype and whether it has spread (Gajjar et al., 2017).

Read About Meduloblastoma on OncoDaily
Chemotherapy Efficacy in Metastatic Brain Tumors
Metastatic brain tumors—cancers that have spread from other parts of the body—are treated differently than primary brain tumors. Chemotherapy’s effectiveness for metastatic brain tumors varies based on the primary cancer site and the ability of the drugs to cross the blood-brain barrier (BBB).
For instance, lung cancer, breast cancer, and melanoma often lead to metastatic brain tumors. In these cases, chemotherapy can be effective in reducing tumor burden and alleviating symptoms. However, the BBB often limits the delivery of chemotherapeutic agents to the brain, making treatment less effective. Targeted therapies, immunotherapy, and systemic chemotherapy may be used, but the success rate can be lower than in other cancers (Kuran et al., 2016).
Factors That Impact Chemotherapy Success
Chemotherapy’s success in treating brain tumors is influenced by multiple factors:
- Tumor Type and Grade: Low-grade gliomas and certain pediatric brain tumors respond better to chemotherapy, while aggressive cancers like GBM are more resistant.
- Location of the Tumor: Tumors located in areas difficult to access or in the brainstem may be less responsive to chemotherapy.
- Age and Overall Health: Younger patients and those in good health may tolerate chemotherapy better, leading to improved outcomes.
- Molecular Characteristics: For gliomas, specific molecular markers like MGMT promoter methylation status influence the likelihood of chemotherapy success. Tumors with this methylation are more likely to respond to temozolomide (Stupp et al., 2005).
- Blood-Brain Barrier (BBB): The ability of chemotherapy drugs to cross the BBB limits the effectiveness of treatment. Newer approaches are exploring ways to bypass this barrier or use targeted delivery mechanisms to enhance drug concentration at the tumor site.
Chemotherapy Side Effects and Management
While chemotherapy is a vital part of treatment, it comes with side effects that can affect a patient’s quality of life. Common side effects of chemotherapy for brain tumors include:
- Fatigue
- Nausea and vomiting
- Hair loss
- Cognitive difficulties
- Increased risk of infections (due to suppressed immune function)
Managing these side effects is crucial for maintaining a patient’s quality of life. Supportive care, including anti-nausea medications, pain management, and cognitive rehabilitation, can help mitigate these challenges and improve the patient’s overall experience.
Advances in Chemotherapy and New Frontiers
Despite the challenges, advancements in chemotherapy regimens, targeted therapy, and personalized treatment are improving the success rates of brain tumor treatment. Clinical trials are continually investigating new chemotherapeutic agents, combination therapies, and targeted drug delivery systems that can more effectively treat brain tumors.
For example, tumor treating fields (TTF) and novel drug delivery methods, like focused ultrasound, are currently being explored to enhance drug penetration into the brain. Additionally, the use of immunotherapy and targeted molecular therapy is becoming increasingly prominent in combination with traditional chemotherapy, improving outcomes for certain brain tumors.
Conclusion
Chemotherapy remains a cornerstone in the treatment of brain tumors, but its success rate depends heavily on tumor type, grade, location, and the patient’s response to treatment. For aggressive tumors like glioblastomas, chemotherapy offers limited survival extension, but newer combination therapies and personalized treatment options are providing hope for better outcomes. For lower-grade gliomas and pediatric tumors, chemotherapy continues to offer high success rates, particularly when coupled with surgery and radiation.
As research continues to unveil new therapies and combination treatments, chemotherapy remains an essential part of the treatment arsenal for brain cancer. Patients and their healthcare teams must consider a range of factors—such as tumor molecular markers, treatment side effects, and overall health status—when determining the most appropriate treatment plan. By staying informed about current treatments and emerging therapies, patients can actively participate in their treatment planning and improve their chances for long-term survival and remission.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD