Kidney Cancer Cure Rate and Survival Outcome in 2025
Kidney cancer, often diagnosed unexpectedly during a routine ultrasound or CT scan, is no longer the silent killer it once was. When diagnosed at a localized stage, the kidney cancer cure rate can reach up to 93%, offering real hope for long-term survival and even complete remission in many patients.
According to the American Cancer Society, over 81,000 new cases of kidney cancer will be diagnosed in the U.S. in 2024, with renal cell carcinoma (RCC) making up the vast majority (Siegel et al., 2024). But here’s the good news: when caught early, kidney cancer is one of the most treatable and curable cancers out there.
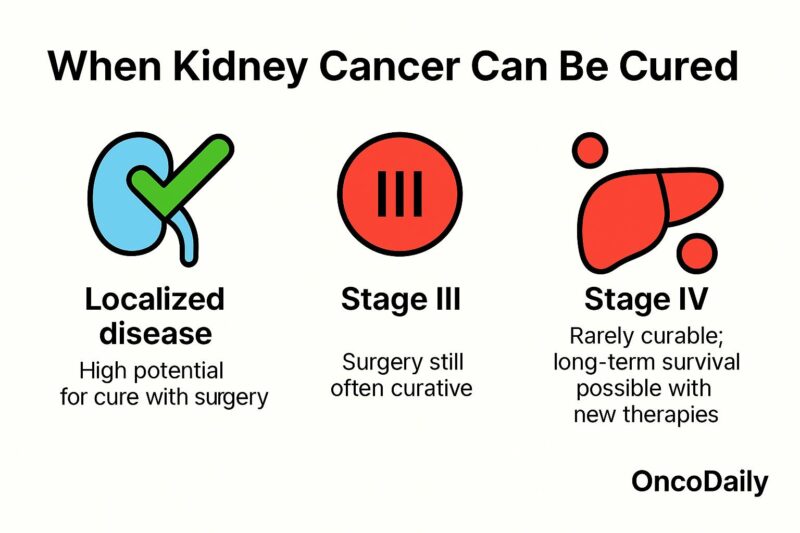
When Is Kidney Cancer Curable?
If kidney cancer is detected while it’s still localized—meaning the tumor hasn’t spread beyond the kidney—the chances of cure are high. Surgery, either removing the whole kidney (radical nephrectomy) or just the tumor (partial nephrectomy), is the gold standard. The five-year survival rate for patients diagnosed at this stage is an impressive 93% (SEER, 2023). For many of these patients, surgery is curative and no further treatment is needed.
Once the disease extends beyond the kidney, however, the picture becomes more complex. Stage III kidney cancer, where the tumor may invade nearby tissues or lymph nodes, still carries a good outlook with a five-year survival of around 70% (NCCN Guidelines, 2024). In these cases, surgery remains the mainstay of treatment, sometimes combined with adjuvant therapy.
The real challenge lies in Stage IV, when cancer has spread to distant organs. While not considered curable in the traditional sense, advanced RCC has seen a revolution in treatment. Thanks to immunotherapy and targeted drugs, long-term remissions—sometimes lasting years—are now possible for a subset of patients (Motzer et al., 2021).
What’s Changing Survival in Advanced Cases?
Just ten years ago, advanced kidney cancer was often treated with cytokines, which had limited benefits and serious side effects. But today, patients have access to cutting-edge immune checkpoint inhibitors like nivolumab and ipilimumab, and VEGF inhibitors like cabozantinib and axitinib. These therapies help the immune system target cancer cells or cut off their blood supply—and in many cases, they work better together.
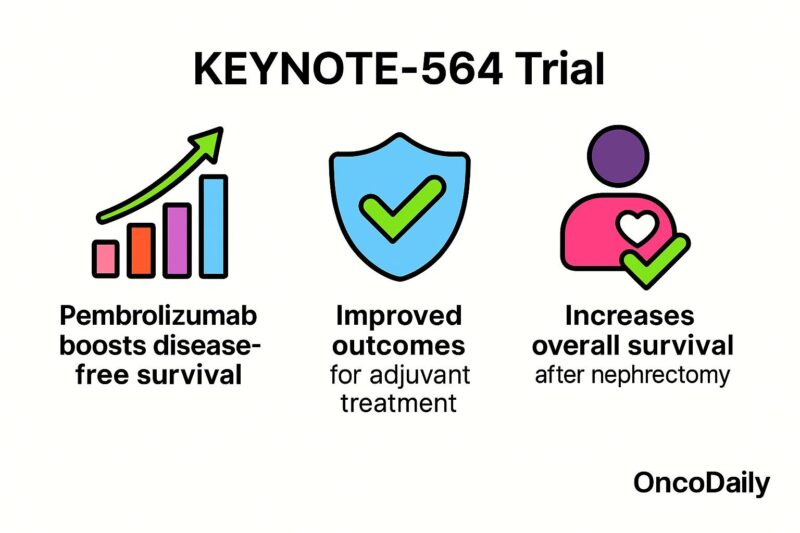
The KEYNOTE-564 trial was a breakthrough. It showed that patients who received pembrolizumab (an immune therapy) after kidney cancer surgery had a 32% lower risk of recurrence than those who didn’t (Choueiri et al., 2021). This finding led to a shift in how early but high-risk cases are managed—and offered new hope for keeping the disease at bay.
Not All Tumors Are the Same
Cure rates also depend on the cancer’s biology. Tumors with aggressive features—like sarcomatoid components or high-grade histology—are more likely to recur. On the other hand, patients with favorable risk profiles, clear cell histology, and strong responses to treatment may live long, cancer-free lives even after Stage IV diagnosis (Heng et al., 2013).
Doctors now use systems like the IMDC risk model to guide treatment choices. Molecular tools, including PD-L1 testing and genomic signatures, are increasingly used to personalize care (Capitanio & Montorsi, 2016).
What Is the IMDC Model?
The IMDC (International Metastatic RCC Database Consortium) risk stratification model, also known as the Heng criteria, is a widely used prognostic tool in metastatic renal cell carcinoma (mRCC). It helps guide treatment decisions and estimate patient outcomes based on six easily measurable clinical and laboratory parameters. These include poor performance status, a short interval between diagnosis and systemic treatment, anemia, elevated corrected calcium, increased neutrophil count, and elevated platelet count. Each factor contributes to the overall risk score.
Based on the total number of risk factors, patients are categorized into three groups. Those with zero risk factors are classified as favorable risk and typically have the best prognosis, with median overall survival often exceeding 40 months. Patients with one to two risk factors fall into the intermediate risk group, where survival averages around 22 to 27 months. Those with three or more risk factors are considered poor risk, with median survival usually ranging between 8 and 12 months.
The IMDC model is essential not only in clinical practice but also in clinical trial design, as it allows oncologists to tailor systemic therapies, including immune checkpoint inhibitors and tyrosine kinase inhibitors, according to risk category. This stratification supports more personalized, evidence-based care for patients with advanced kidney cancer.
What About the Future?
The future of kidney cancer treatment is bright. New combinations of immunotherapy and targeted drugs are in development. Trials are exploring how artificial intelligence and liquid biopsies can detect recurrence earlier. More importantly, global efforts are underway to make these therapies accessible in low- and middle-income countries where survival rates still lag behind.
Conclusion
Kidney cancer is no longer a mystery diagnosis or a death sentence. Early-stage cases are often curable. Even in more advanced disease, breakthroughs in immunotherapy have pushed the boundaries of survival. The path forward involves not just smarter drugs, but smarter strategies—tailoring treatment based on tumor biology, patient needs, and access to care.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
