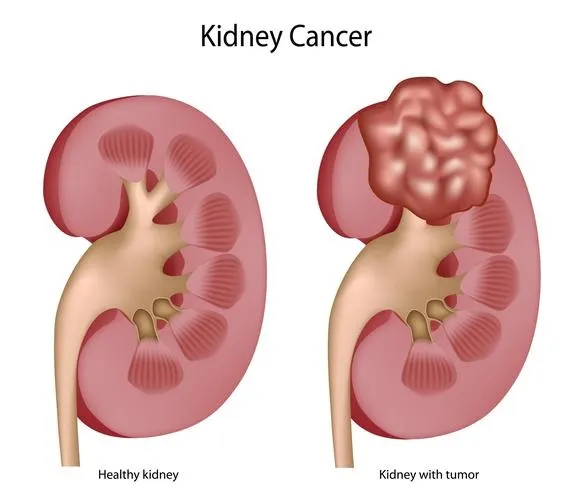
Kidney cancer, also known as renal cancer, originates in the kidneys—two bean-shaped organs located on either side of the spine, responsible for filtering blood and producing urine. In recent years, kidney cancer has become a significant health concern. According to the American Cancer Society, it ranks among the top ten most common cancers in adults, accounting for approximately 4% to 5% of all cancer cases in the United States.
This article aims to provide a comprehensive overview of kidney cancer, including its types, risk factors, symptoms, diagnosis, treatment options, and recent advancements in research. By understanding these aspects, individuals can be better informed about the disease and the importance of early detection and treatment.
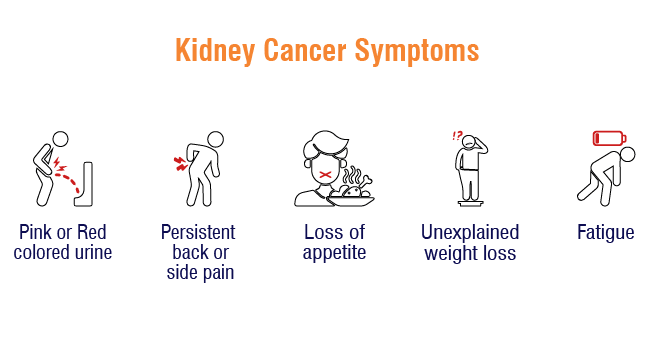
What Are the Symptoms of Kidney Cancer?
One of the primary symptoms of kidney cancer is hematuria, or the presence of blood in the urine. This can manifest as pink, red, or cola-colored urine. However, hematuria is often intermittent and painless, leading individuals to overlook or attribute it to less severe conditions like urinary tract infections or kidney stones. According to the American Cancer Society, blood in the urine is a common symptom but can be caused by benign conditions, making it less alarming to patients.
Another common symptom is persistent pain in the back or flank (the side between the ribs and hip). This pain is typically dull and aching, which can be mistaken for muscle strain or arthritis. The subtle nature of this discomfort often leads to delays in seeking medical attention. As noted by the American Cancer Society, these cancers usually do not cause pain or other symptoms when they are found, leading to incidental findings during imaging tests for other reasons.
Due to the nonspecific nature of these symptoms, many kidney cancers are discovered incidentally during imaging studies for unrelated issues. This incidental detection often occurs because the early stages of kidney cancer may not present noticeable symptoms, underscoring the importance of regular medical check-ups and awareness of subtle bodily changes.
What Causes Kidney Cancer?
According to the American Cancer Society, several well-established risk factors increase the likelihood of developing kidney cancer. These include:
- Older age-The risk of kidney cancer increases with age, with most cases occurring in people over 60.
- Smoking– Is a significant risk factor for kidney cancer. The risk increases with the amount and duration of smoking. However, the risk decreases gradually after quitting smoking.
- Obesity– Excess body weight is linked to an increased risk of kidney cancer. Obesity can cause changes in certain hormones that may lead to the development of renal cell carcinoma
- High blood pressure-People with high blood pressure have a higher risk of developing kidney cancer. This risk remains even if the high blood pressure is being treated with medication.
- Long-term dialysis-People with advanced kidney disease, especially those on long-term dialysis, have a higher risk of developing kidney cancer.
These risk factors are important to understand, as they can guide both prevention efforts and early detection strategies.
Genetics and Kidney Cancer
Some cases of kidney cancer are linked to inherited genetic syndromes, making certain individuals and families more susceptible to the disease. According to the American Cancer Society, several hereditary conditions significantly increase kidney cancer risk:
One of the most well-known syndromes is von Hippel-Lindau (VHL) disease, a rare genetic disorder caused by mutations in the VHL gene. People with VHL are at high risk of developing multiple tumors, including clear cell renal cell carcinoma, which is the most common type of kidney cancer.
Other hereditary syndromes associated with increased kidney cancer risk include:
- Hereditary Leiomyomatosis and Renal Cell Cancer (HLRCC)
- Birt-Hogg-Dubé Syndrome
- Hereditary Papillary Renal Cell Carcinoma (HPRC)
- Tuberous Sclerosis Complex (TSC)
These syndromes are usually passed down in families and can be identified through genetic testing. Individuals with a strong family history of kidney cancer or known genetic mutations are considered high-risk populations and may benefit from regular screening and early monitoring. Identifying and managing these high-risk groups is crucial for early detection and prevention.
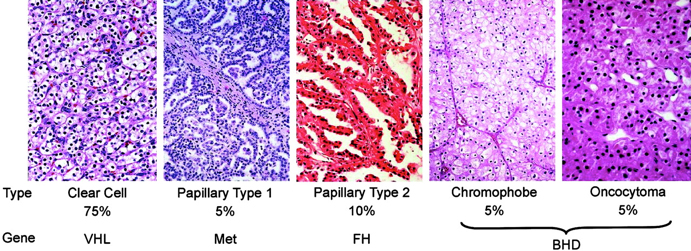
What Are the Types of Kidney Cancer?
Renal cell carcinoma (RCC) comprises various subtypes, each with distinct characteristics, progression patterns, and prognoses:
- Clear Cell Renal Cell Carcinoma (ccRCC): This is the most prevalent RCC subtype, accounting for approximately 70% to 80% of cases. According to a study published in the Korean Journal of Urology, the five-year survival rate for ccRCC confined to the kidney is around 81%. However, this rate decreases significantly if the cancer has metastasized.
- Papillary Renal Cell Carcinoma (pRCC): Representing about 10% to 15% of RCC cases, pRCC is further categorized into two types: Papillary Renal Cell Carcinoma (pRCC) is divided into two main types, each with different outcomes. According to a study published in Scientific Reports, Type I pRCC generally has a more favorable prognosis. The study found that patients with Type I pRCC had a five-year cancer-specific survival (CSS) rate of 95.2%, meaning most patients lived at least five years after diagnosis without cancer progression. On the other hand, Type II pRCC is typically associated with a poorer outcome. The same study reported that the five-year CSS rate for Type II pRCC was 75.7%, showing a significantly lower survival rate compared to Type I. These differences highlight the importance of identifying the subtype to better predict patient outcomes and guide treatment decisions.
- Chromophobe Renal Cell Carcinoma: This subtype accounts for approximately 3% to 5% of RCC cases. Patients with chromophobe RCC generally have a favorable prognosis, with five-year survival rates exceeding 90%.
- Collecting Duct Carcinoma: A rare and aggressive form of RCC, collecting duct carcinoma often presents at an advanced stage. Due to its rarity, specific survival statistics are limited, but the prognosis is generally considered poor.
- Medullary Renal Cell Carcinoma: This rare subtype predominantly affects individuals with sickle cell trait. It is characterized by aggressive behavior and a poor prognosis, with many patients experiencing rapid disease progression.
Understanding these subtypes is crucial for determining appropriate treatment strategies and providing patients with accurate prognostic information.
Renal Cell Carcinoma (RCC)
This is the most common type of kidney cancer, accounting for about 90% of cases. RCC begins in the lining of the small tubes (renal tubules) in the kidney. There are several subtypes of RCC:
- Clear Cell RCC: The most common subtype, representing about 70% of RCC cases.
- Papillary RCC: Makes up about 10-15% of RCC cases and has two subtypes: Type 1 and Type 2.
- Chromophobe RCC: A rare subtype, accounting for about 5% of RCC cases.
- Collecting Duct Carcinoma: A very rare and aggressive form of RCC.
- Translocation RCC: A rare type seen mostly in children and young adults.
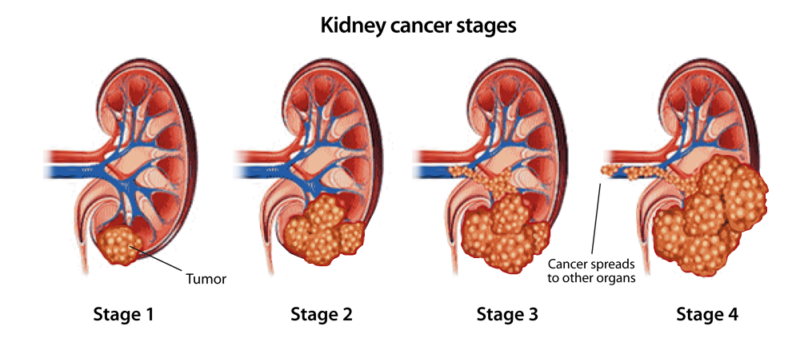
What Are the Stages of Kidney Cancer?
Kidney cancer staging is a critical process that determines the extent of cancer spread and guides treatment decisions. The American Joint Committee on Cancer (AJCC) utilizes the TNM system to classify kidney cancer into four main stages:
-
Stage I: The tumor is confined to the kidney and measures 7 centimeters or smaller.
-
Stage II: The tumor is larger than 7 centimeters but remains confined to the kidney.
-
Stage III: The tumor has extended into major veins or perinephric tissues but has not spread to distant lymph nodes or other organs.
-
Stage IV: The cancer has metastasized to distant lymph nodes or other parts of the body.
Understanding the stage of kidney cancer is crucial for determining the most appropriate treatment and prognosis. If you have any concerns or symptoms, it’s important to consult with a healthcare professional for proper diagnosis and care.
How is Kidney Cancer diagnosed?
Diagnosing kidney cancer requires a careful combination of medical history, physical examinations, imaging studies, laboratory tests, and sometimes tissue biopsies to confirm the presence and type of cancer.
The process typically begins with a detailed medical history. The doctor will ask questions about any symptoms, lifestyle habits, family history of kidney cancer, and known risk factors such as smoking or high blood pressure. A physical examination follows, during which the physician may check for an abnormal mass in the abdomen or any other physical signs that could suggest kidney problems.
Imaging tests are central to diagnosing kidney cancer. An ultrasound is often one of the first imaging studies performed; it uses sound waves to produce images of the kidneys and helps distinguish between harmless fluid-filled cysts and potentially dangerous solid tumors. For more detailed views, a CT scan (Computed Tomography) is used. CT scans provide cross-sectional images of the kidneys, showing the size, shape, and exact location of any tumors and whether the cancer has spread to nearby lymph nodes or tissues. In some cases, an MRI (Magnetic Resonance Imaging) is preferred, especially when more detailed images of soft tissues are needed. Another imaging test, the Intravenous Pyelogram (IVP), involves injecting a contrast dye into a vein, followed by X-rays to visualize how the kidneys and urinary tract are functioning.
Alongside imaging tests, doctors conduct lab tests to evaluate kidney function and detect potential warning signs of cancer. Blood tests measure levels of substances such as creatinine to check how well the kidneys are filtering waste. Abnormal levels may suggest kidney dysfunction. Urine tests (urinalysis) are also essential, as they can detect blood in the urine (hematuria) and other abnormalities often associated with kidney cancer.
In certain cases, when imaging and lab tests do not provide a clear diagnosis, a kidney biopsy may be performed. This procedure involves removing a small tissue sample from the kidney with a needle, which is then examined under a microscope to determine if cancer cells are present and to identify the specific type of kidney cancer. Additionally, doctors may use tests like cystoscopy and ureteroscopy to examine the bladder, urethra, ureter, and renal pelvis. In a cystoscopy, a thin tube with a lens is inserted through the urethra to inspect the bladder, while ureteroscopy uses a lighted tube to look further into the ureter and renal pelvis.
Together, these diagnostic tools provide a comprehensive picture of the patient’s condition, allowing healthcare professionals to develop an accurate diagnosis and tailor the most effective treatment plan. Early and precise diagnosis is essential to achieving better outcomes in kidney cancer care.
What Are the Treatment Options for Kidney Cancer?
Treatment options for kidney cancer vary based on the stage, type, and overall health of the patient. According to the American Cancer Society, the main treatments include:
- Surgery
- Ablation therapies (such as cryoablation and radiofrequency ablation)
- Radiation therapy
- Targeted therapy
- Immunotherapy
These treatment methods can be used alone or in combination, depending on the specific needs of each patient. Choosing the right treatment approach is crucial for achieving the best outcomes.
Surgery for Kidney Cancer
Surgery is the mainstay treatment for kidney cancer, particularly when the tumor is confined to the kidney. The two primary surgical approaches are radical nephrectomy and partial nephrectomy, with the choice depending on the tumor’s size, location, and whether the cancer has spread.
A radical nephrectomy involves removing the entire kidney, including the surrounding fatty tissue and, in some cases, nearby lymph nodes. This procedure can be done through a traditional open surgery or laparoscopically, using smaller incisions, which generally leads to quicker recovery times. Radical nephrectomy is typically recommended for larger tumors or when cancer has invaded surrounding tissues. While removing a kidney might sound concerning, most patients can live normally with one healthy kidney, though long-term kidney function is closely monitored.
In contrast, a partial nephrectomy, also called nephron-sparing surgery, involves removing only the tumor and a small margin of healthy tissue, leaving the rest of the kidney intact. This method is often preferred for small tumors (typically under 4 cm) or when preserving kidney function is crucial, such as in patients with only one kidney or pre-existing kidney disease. Partial nephrectomy has shown excellent outcomes, offering similar cancer control to radical nephrectomy while reducing the risk of chronic kidney disease. For patients whose cancer has spread (metastasized), a cytoreductive nephrectomy may be considered. In this case, the goal is not to cure the disease but to remove as much of the tumor as possible to enhance the effectiveness of systemic treatments like targeted therapy or immunotherapy.
Recovery from nephrectomy varies based on the type of surgery. Most patients can return to normal activities within a few weeks, especially after laparoscopic procedures. However, as with any major surgery, there are risks, including bleeding, infection, and reduced kidney function.
According to clinical studies referenced by the American Cancer Society, both radical and partial nephrectomies offer high success rates in treating localized kidney cancer, with five-year survival rates exceeding 90% for early-stage disease. The choice of surgery is tailored to each patient’s condition, aiming to achieve the best balance between removing cancer and preserving kidney health.
Targeted Therapy for Kidney Cancer
Targeted therapy has become a cornerstone in the treatment of advanced kidney cancer, offering more precise control over cancer growth compared to traditional chemotherapy. These drugs focus specifically on the molecular pathways that cancer cells use to grow and spread, making them highly effective in many cases.
One of the most widely used targeted therapies is the class of Tyrosine Kinase Inhibitors (TKIs). Drugs like sunitinib (Sutent) and pazopanib (Votrient) work by blocking proteins responsible for promoting cancer cell growth and the formation of new blood vessels (angiogenesis), which tumors need to survive and expand. Clinical studies have shown that sunitinib significantly improves progression-free survival (PFS). According to research published by Motzer et al. in the New England Journal of Medicine, sunitinib demonstrated a median PFS of 11 months compared to 5 months for interferon-alpha, the previous standard treatment (Motzer RJ et al., NEJM, 2007).
Pazopanib, another TKI, has also been shown to provide similar benefits. In a phase III study, pazopanib achieved a median PFS of 9.2 months, which is comparable to sunitinib. Additionally, patient-reported outcomes suggest that some patients find pazopanib better tolerated, with fewer side effects such as fatigue and diarrhea, which are commonly associated with sunitinib. Further options include mTOR inhibitors such as everolimus (Afinitor) and temsirolimus (Torisel), which block a protein involved in cancer cell growth. For patients whose cancer progresses after TKIs, everolimus has shown median PFS improvements and is a common second-line treatment.
Additionally, VEGF inhibitors like bevacizumab (Avastin) target the vascular endothelial growth factor pathway, limiting blood supply to tumors. Bevacizumab is often combined with other therapies for enhanced effectiveness. Another promising approach involves combining targeted therapy with immunotherapy. The combination of pembrolizumab (Keytruda), a checkpoint inhibitor, and axitinib (Inlyta), a TKI, has been approved for first-line treatment of advanced kidney cancer. In clinical trials, this combination demonstrated significantly improved outcomes, with a reported overall survival rate of 89.9% at 12 months, compared to 78.3% with sunitinib alone (Rini BI et al., NEJM, 2019).
While targeted therapies have improved survival and disease control, they can come with side effects like high blood pressure, diarrhea, fatigue, and hand-foot syndrome. However, for many patients, the benefits outweigh the risks, and the availability of multiple targeted therapies allows for tailored treatment based on the individual’s health and response.
Latest treatment approaches for kidney cancer
Recent advancements in kidney cancer treatment have introduced innovative approaches, offering hope for improved patient outcomes.
- Personalized Cancer Vaccines: A small clinical trial led by researchers at Dana-Farber Cancer Institute and Yale Cancer Center explored a personalized cancer vaccine for patients with advanced kidney cancer. The vaccine, tailored to each patient’s tumor profile, successfully elicited an immune response in all nine participants. Notably, these patients remained cancer-free for nearly four years post-treatment. While these findings are promising, larger-scale studies are necessary to confirm the vaccine’s efficacy.
- Combination Therapies: Combining immunotherapy agents has shown significant benefits. For instance, the combination of nivolumab (Opdivo) and ipilimumab (Yervoy) demonstrated a 37% reduction in the risk of death compared to sunitinib (Sutent) in advanced renal cell carcinoma patients. After two years, 67% of patients receiving the combination therapy were alive, versus 56% on sunitinib.
- Targeted Therapies: Advancements in targeted treatments continue to evolve. The phase II PAPMET trial highlighted cabozantinib’s efficacy for metastatic papillary renal cell carcinoma, a rare subtype lacking effective treatments. This regimen is now included in the National Comprehensive Cancer Network’s guidelines for treating papillary RCC.
These developments underscore the importance of ongoing research and clinical trials in enhancing kidney cancer treatment strategies.
What is the Prognosis for Kidney Cancer?
The prognosis for kidney cancer depends largely on three key factors: the stage of cancer at diagnosis, the age of the patient, and how well the cancer responds to treatment. Each of these factors plays a significant role in determining survival outcomes.
Stage at diagnosis is one of the strongest indicators of survival. According to the American Cancer Society, patients diagnosed with localized kidney cancer (Stage I), where the tumor is confined to the kidney, have a 5-year relative survival rate of about 93%. For cancers that have spread to nearby lymph nodes or tissues (Stage II or III, regional stage), the survival rate decreases to approximately 75%. However, when the cancer has metastasized to distant parts of the body, such as the lungs, bones, or brain (Stage IV, distant stage), the survival rate drops sharply to about 18%
Age is another important factor. Data from the SEER program shows that younger patients generally have better survival outcomes. For instance, patients under 15 years old have a 5-year survival rate of about 92.4%, while those aged 15 to 39 years have around 88.9%. The survival rate decreases to 80.9% in patients aged 40 to 64 years, and further drops to 74.8% in those between 65 and 74 years. For individuals 75 years and older, the survival rate is approximately 61.2%
Additionally, a patient’s response to treatment significantly influences their prognosis. Those who respond well to initial therapies like surgery, targeted therapy, or immunotherapy tend to experience better survival outcomes. On the other hand, tumors that are resistant to these treatments pose greater challenges, often leading to poorer results. The rise of personalized medicine is helping improve this, as newer therapies are increasingly tailored to the specific genetic and molecular characteristics of each patient’s tumor, increasing the chance of successful outcomes.
How Can You Reduce Your Risk of Kidney Cancer?
To help lower the risk of kidney cancer, doctors recommend several key prevention strategies. Quitting smoking is one of the most important steps, as smoking significantly increases the risk. Maintaining a healthy weight and managing high blood pressure also play crucial roles in prevention. While there’s no standard screening test for kidney cancer, people with a family history or certain risk factors may benefit from regular check-ups and imaging tests to catch any issues early. Leading a healthy lifestyle overall can greatly reduce kidney cancer risk.
You Can Watch More on OncoDaily Youtube TV
Written by Mariam Chkheidze, MD
FAQ
What is kidney cancer?
Kidney cancer is a type of cancer that starts in the kidneys, most commonly as renal cell carcinoma (RCC).
What are the early symptoms of kidney cancer?
Early symptoms include blood in the urine, back or flank pain, a lump in the abdomen, and unexplained weight loss.
How is kidney cancer diagnosed?
Doctors use imaging tests like ultrasound, CT scans, and MRIs, along with blood and urine tests, to diagnose kidney cancer.
What are the main types of kidney cancer?
The most common type is renal cell carcinoma (RCC), with subtypes like clear cell RCC, papillary RCC, and chromophobe RCC.
What are the stages of kidney cancer?
Stages range from Stage I (localized tumor) to Stage IV (cancer spread to distant organs).
What causes kidney cancer?
Common causes include smoking, obesity, high blood pressure, genetic syndromes, and long-term dialysis.
What are the treatment options for kidney cancer?
Treatment options include surgery, targeted therapy, immunotherapy, radiation therapy, and ablation techniques.
What is the survival rate for kidney cancer?
Early-stage kidney cancer has a 5-year survival rate of around 93%, but survival rates drop if the cancer spreads.
Can kidney cancer be prevented?
While not always preventable, quitting smoking, maintaining a healthy weight, and managing blood pressure reduce the risk.
Is kidney cancer hereditary?
Some cases are linked to genetic conditions like von Hippel-Lindau disease; family history increases risk.