Immunotherapy is moving beyond advanced disease into the curative setting. In colorectal cancer, trials are testing PD-1 inhibitors with chemotherapy, radiotherapy, and even TIL therapy before and after surgery—aiming to shrink tumors, eliminate micrometastases, and boost surgical outcomes. From neoadjuvant chemo-IO regimens to SBRT plus checkpoint blockade after liver resection, the goal is clear: turn high-risk patients into long-term survivors, and bring cure within reach.
Camrelizumab + Neoadjuvant Chemotherapy After Stent Placement in Left-Sided Obstructive Colorectal Cancer
A Phase I/II single-arm trial is testing whether adding immunotherapy to standard neoadjuvant chemotherapy can improve outcomes for patients with left-sided obstructive colorectal cancer who undergo stent placement before surgery.
In this study, patients first receive a self-expanding metallic stent (SEMS) to relieve obstruction. Once stable, they are treated with:
- Camrelizumab (anti–PD-1 antibody, 200 mg IV) × 2 cycles
- Neoadjuvant chemotherapy with either mFOLFOX6 (3 cycles) or CapeOx (2 cycles)
- Surgery follows 2–3 weeks after chemotherapy.
The trial aims to test whether this approach:
- Improves overall survival (OS) and progression-free survival (PFS) by eradicating micrometastases
- Increases primary anastomosis rates and reduces permanent stoma formation by allowing longer bowel decompression before surgery
- Maintains safety and tolerability compared with standard emergency surgery.
A total of 20 patients will be enrolled in China, with study completion expected in December 2026.
Neoadjuvant Tislelizumab + CapeOX for Locally Advanced Colon Cancer
A Phase II, single-arm, investigator-initiated study is testing neoadjuvant tislelizumab (anti–PD-1) plus CapeOXbefore curative resection in locally advanced colon adenocarcinoma (cT3-4 and/or N+, M0).
Treatment plan
- Tislelizumab 200 mg IV Day 1 (q3w)
- Oxaliplatin 130 mg/m² IV Day 1
- Capecitabine 1000 mg/m² orally, twice daily, Days 1–14
After approximately three weeks of treatment, patients will undergo re-evaluation to assess tumor response. Surgery is then planned three to five weeks after completion of the second treatment cycle. Following resection, patients will be monitored according to standard protocols, with CT scans performed at one and three years to track long-term outcomes. Surgical specimens and associated clinical data will also be collected for integrative multi-omics analysis, aiming to develop a predictive model of treatment efficacy.
The study’s primary endpoints, assessed at six months, include the rate of pathological complete response (pCR) and the objective response rate (ORR). Key secondary outcomes include the rate of major pathological response, defined as tumors with ≤10% residual viable cells, the proportion of patients achieving R0 resection, as well as disease-free survival and overall survival at two years.
- Design notes: single center, open-label; planned N=100; adults ECOG 0–1; biomarker consent required. The trial asks whether short-course PD-1 blockade plus chemotherapy can deepen tumor regression, increase R0/pCR, and inform biomarker-driven perioperative strategies.
Effect of Gut Microbiota on Immunotherapy in Metastatic Colorectal Cancer
This prospective, single-center observational study is investigating how the gut microbiota influences the effectiveness of immunotherapy in patients with metastatic colorectal cancer (mCRC). A total of 50 patients treated at the First Hospital of Jilin University will be enrolled between 2024 and 2026.
Stool and blood samples are collected at baseline (before immunotherapy) and again after one cycle, then stored at –80°C. Six months after treatment with PD-1 inhibitor sintilimab plus fruquintinib, patients will be evaluated using iRECIST criteria and categorized as responders or non-responders.
The study applies multi-omics profiling, including metagenomic sequencing, proteomics, and metabolomics, to identify key microbial species and pathways linked to treatment response. Correlation analyses will explore how gut microbiota interact with immune and metabolic changes. Findings will be validated in animal models to uncover mechanisms by which intestinal microbes modulate PD-1 efficacy.
The primary outcome is treatment response at six months, classified as objective response or durable stable disease versus progression. The ultimate goal is to clarify microbiota–immunotherapy interactions, paving the way for personalized strategies to enhance immunotherapy efficacy in colorectal cancer.
Neoadjuvant Immunotherapy for T4 dMMR Colon Cancer
This phase II, prospective, single-arm clinical trial is evaluating whether neoadjuvant immunotherapy can improve surgical outcomes in patients with T4 colon cancer and deficient mismatch repair (dMMR). Standard chemotherapy is often ineffective in this group, but immune checkpoint blockade has shown high pathologic response rates, making it a promising strategy before surgery.
Patients receive camrelizumab (200 mg IV) every 3 weeks for three cycles, followed by surgery 2–3 weeks after the last dose. The type and extent of resection are determined by the operating surgeon, with the goal of achieving R0 resection while preserving adjacent organs.
The primary endpoint is the R0 resection rate, defined as no tumor infiltration within 1 mm of surgical margins. Secondary endpoints include:
- Pathologic complete response (pCR) (per Mandard regression grading)
- Disease-free survival (DFS) at 3 years
- Overall survival (OS) at 5 years
- Safety and tolerability of camrelizumab, assessed by CTCAE v5.0
The study aims to enroll 18 patients at Peking Union Medical College Hospital, with completion expected in 2030. If successful, this trial could establish neoadjuvant PD-1 blockade as a new treatment paradigm for dMMR T4 colon cancer, offering better surgical outcomes and long-term survival.
Neoadjuvant Immune Checkpoint Inhibition and Novel IO Combinations in Early-Stage Colon Cancer
This multi-center, open-label, phase II exploratory trial is testing short-term neoadjuvant immunotherapy and novel immuno-oncology (IO) combinations in patients with stage I–III colon adenocarcinoma without distant metastases. Treatment is given during the ~6-week window before surgery.
Originally, the trial enrolled 60 patients (30 MSI/dMMR, 30 MSS/pMMR). Patients with MSS tumors were randomized, while all MSI tumors received ipilimumab + nivolumab. Over time, the study expanded to include novel IO combinations, with multiple amendments adding new cohorts.
Treatment cohorts include:
- Group 1 (closed): Ipilimumab (1 mg/kg, day 1) + Nivolumab (3 mg/kg, days 1 and 15)
- Group 2 (closed): Same as Group 1 + daily celecoxib until surgery
- Cohort 4 (closed, MSS): Nivolumab + anti-IL8 (BMS-986253)
- Cohort 5 (active, MSS): Nivolumab + relatlimab (anti-LAG3)
- Cohort 6 (closed, MSI): Nivolumab + relatlimab
The trial’s primary endpoints focus on safety, assessed by adverse events according to CTCAE v4.0, and three-year disease-free survival in the expanded MSI cohort. Secondary endpoints include immune activation measured by paired biopsies before and after treatment, relapse-free survival, and long-term disease-free survival extending up to five years.
In total, 268 patients are planned for enrollment—an expansion from the original 60 participants to include both MSI and MSS cohorts. Recruitment began in 2017 and is expected to conclude in late 2024.
This trial has been pivotal in showing that short-course neoadjuvant immunotherapy can induce major and complete pathologic responses even in early-stage colon cancer, potentially reshaping standard treatment for dMMR tumors and guiding IO combinations for MSS disease.
Autologous TILs + Pembrolizumab + IL-2 in Refractory Colorectal Cancer
A personalized cell therapy approach for advanced/metastatic, treatment-refractory colorectal cancer using autologous tumor-infiltrating lymphocytes (TILs), combined with pembrolizumab (PD-1 blockade) and aldesleukin (IL-2) to boost anti-tumor immunity.
How it works (treatment flow):
- Tumor harvest → TIL expansion ex vivo.
- Lymphodepletion: cyclophosphamide (2 days) + fludarabine (5 days).
- Priming PD-1 blockade: pembrolizumab given before TIL infusion; TIL infusion (Day 0).
- Activation support: high-dose IL-2 (up to 8 bolus doses) after TILs.
- Pembrolizumab maintenance: additional doses (e.g., ~Day 28 & 70), then q6-week maintenance up to 1 year if tolerated.
Design: Open-label, single-arm Phase I/II study (recruiting; planned n≈85). Safety monitored closely during admission and follow-up; responses assessed by RECIST v1.1.
The study’s primary endpoint is the objective response rate (ORR). Secondary endpoints include disease control rate (DCR), duration of response (DOR), progression-free survival (PFS), overall survival (OS), and quality of life (QoL).
Neoadjuvant Dostarlimab Plus CAPEOX vs CAPEOX Alone in Resectable MMRp/MSS Colon Cancer
This Phase II, open-label, randomized trial is testing whether adding dostarlimab, a PD-1 inhibitor, to standard CAPEOX chemotherapy (capecitabine + oxaliplatin) improves outcomes in patients with previously untreated, resectable T4N0 or stage III mismatch repair proficient/microsatellite stable (MMRp/MSS) colon cancer. Treatment is given before surgery in the neoadjuvant setting, aiming to increase pathological response and surgical success rates.
- Experimental arm: Dostarlimab + CAPEOX
- Control arm: CAPEOX alone
This Phase II trial is evaluating neoadjuvant dostarlimab plus CAPEOX versus CAPEOX alone in resectable MMRp/MSS colon cancer. The primary goals are to measure major pathological response, defined as ≤10% residual viable tumor, and to assess safety, including immune-related toxicities. Key secondary outcomes include complete pathological response, rates of successful tumor resection, and long-term efficacy with disease-free and overall survival.
About 120 patients will be enrolled in Belgium and Spain, with the study launched in February 2025, primary completion expected in mid-2026, and final completion in 2028.
Neoadjuvant Atezolizumab + CAPOX for Resectable pMMR Colon Cancer
Single-arm study (n=28 planned) testing four 3-week cycles of atezolizumab given before CAPOX across a 12-week neoadjuvant window, followed by standard surgical resection. High-risk patients (per guidelines) may receive adjuvant mFOLFOX6 or CAPOX at the investigator’s discretion.
Primary endpoint is pathological tumor regression (TRG-0/1; <10% viable tumor) in the resection specimen; patients not reaching surgery count as failures. Key secondary measures include complete pathologic response, R0 resection rate, safety (CTCAE v5.0, grade ≥3 AEs and surgical timing), and patient-reported quality of life (EORTC QLQ-C30, MDASI).
The trial embeds serial ctDNA monitoring (mandatory) and optional stool/biobank collections at baseline, mid-therapy, end of neoadjuvant therapy, early postoperative, and during follow-up to explore early efficacy signals and biomarker correlations. Post-op assessments occur at week 2, months 3 and 6; long-term surveillance visits at months 12–36 follow standard of care. The study’s endpoint for each participant is the 6-month postoperative visit.
Tiragolumab + Atezolizumab with SBRT for MSS Metastatic Colorectal Cancer
This NCI-led trial tests dual checkpoint blockade (anti-TIGIT tiragolumab + anti-PD-L1 atezolizumab) paired with focal stereotactic body radiotherapy (SBRT) to overcome immunotherapy resistance in microsatellite-stable (MSS) mCRC. Up to 30–36 adults receive IV tiragolumab and atezolizumab every 3 weeks for ≤2 years; SBRT is delivered to one lesion on days 1, 3, and 5 of cycle 1, with a separate non-irradiated lesion tracked for response. Imaging is repeated every 9 weeks; optional biopsies occur at baseline and early on-treatment.
Endpoints
- Primary: (Part A) confirm RP2D via dose-limiting toxicities through cycle 1; (Part B) 9-week progression-free rate.
- Key secondary: safety/tolerability; best overall response (RECIST v1.1); PFS and OS (Kaplan–Meier).
Eligibility (selected): MSS mCRC, ECOG 0–1, ≥2 measurable lesions (≥1 SBRT-eligible and ≥1 outside the radiation field), progression after ≥2 standard metastatic lines (including anti-EGFR if RAS WT), adequate organ function.
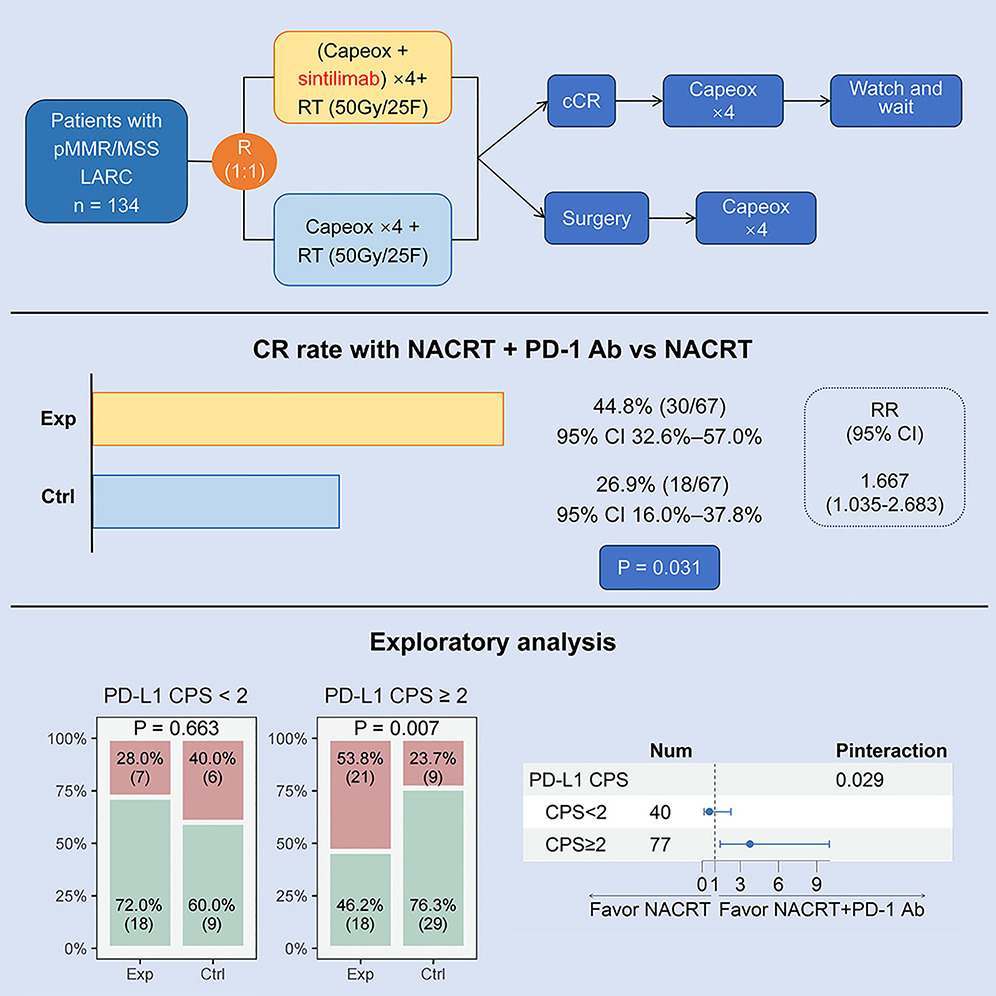
SBRT + PD-1 Immunotherapy Added to Adjuvant Chemotherapy After Liver Metastasectomy in CRC
: In high-risk colorectal cancer liver metastasis (CRLM) after resection (≤5 lesions; R1/R2 or <0.5 cm margins; no extrahepatic disease), this study tests whether adding liver-directed stereotactic body radiotherapy (SBRT) plus PD-1 blockade (sintilimab) to standard postoperative chemotherapy improves outcomes versus chemotherapy alone.
Design and Arms (N=80; open-label, parallel):
- Experimental: Postoperative SBRT to liver bed/lesions + investigator’s-choice chemo (XELOX/FOLFOX/FOLFIRI) + sintilimab 200 mg IV q3w for ~18 weeks.
- Control: Postoperative chemotherapy alone (same regimens, ~18 weeks).
This randomized phase II trial is evaluating whether adding stereotactic body radiotherapy (SBRT) and PD-1 blockade with sintilimab to standard postoperative chemotherapy can improve outcomes in patients with resected colorectal cancer liver metastases at high risk of recurrence.
The primary endpoint is 12-month progression-free survival, with key secondary measures including local hepatic control, overall survival at 36 months, and rates of grade 3–4 treatment-related toxicity. Eligible patients are adults with controlled primary CRC, resected CRLM with close or positive margins, good performance status, and no prior immunotherapy or extrahepatic disease.
You Can Also Read About 10 Ongoing Clinical Trials on Immunotherapy in Lung Cancer

Written by Toma Oganezova, MD, Editor-in-Chief of OncoDaily IO