This week in OncoDaily Immuno-Oncology, new studies redefine how we match patients to treatment – from trials comparing immunotherapy to targeted therapy in lung cancer and validating PD1 mRNA as a pan-cancer biomarker, to insights linking immune cell infiltration with response in breast cancer and record survival in liver cancer. Emerging work highlights macrophage-driven immunity in pediatric tumors, CRISPR-enhanced immunotherapy for blood cancers, and refined strategies for dual checkpoint blockade—together marking another leap forward for precision immunotherapy.
Fawzi Abu Rous (Medical Oncologist at Henry Ford Health):
“Glad to have participated in the FRONT-BRAF study comparing immunotherapy with or without chemotherapy to BRAF/MEK inhibitors in 1st line treatment of BRAF-mut NSCLC. This is a highly relevant paper that can have immediate implications in the clinic!
Huge thanks to Biagio Ricciuti and Alessandro Di Federico for leading this effort and congrats to all co-authors!”
Elia Seguí (Advanced Research Fellow of Breast Oncology at Dana-Farber Cancer Institute):
“Extremely happy to see this out today in ESMO Open!
Building on prior work identifying PD1 mRNA as a promising biomarker for anti-PD1 response, ACROPOLI was a prospective, phase 2 study designed to evaluate the efficacy of anti-PD1 monotherapy in patients with advanced solid tumors and high PD1 mRNA expression.
- >1,000 patients prescreened across 33 cancer types through a huge effort by SOLTI #cancerresearch and the Translational Solid Tumors Lab at Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS)
- 56 patients with high PD1 mRNA received anti-PD1 → ORR 18%. Responses observed in cancers typically resistant to ICIs, including pancreatic and microsatellite-stable colorectal cancers.
- Sample recency mattered: ORR increased to 33% when recent tissue (<12mo) was used for testing, highlighting how dynamic the tumor immune microenvironment is.
I was lucky to lead the translational analyses under the mentorship of Aleix Prat, Josep Tabernero, and Fara Brasó Maristany , studying protein, RNA, and DNA determinants of response.
Findings suggest that a composite biomarker strategy, integrating immune and tumor-intrinsic features, may improve patient selection for ICIs.
An incredible journey to be part of – and just the beginning of exploring how to better match the right patient with the right treatment.”
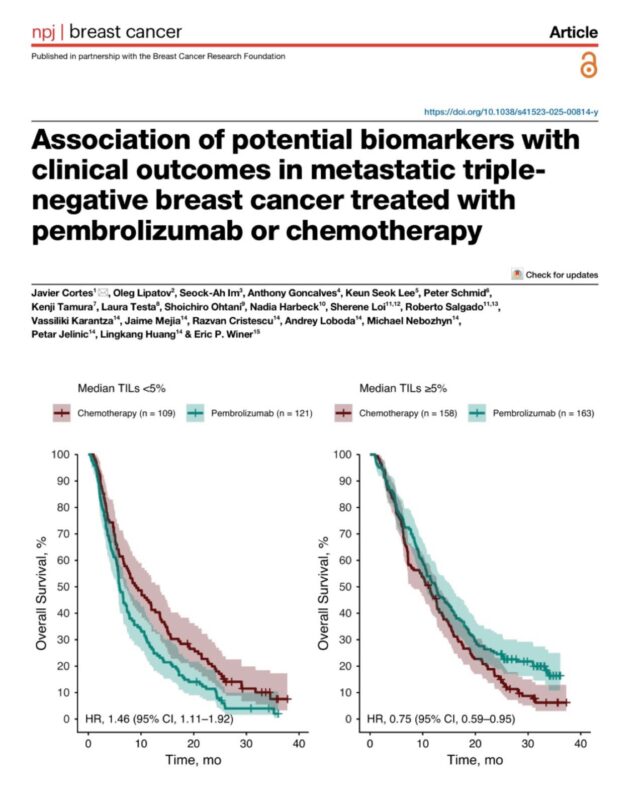
Paolo Tarantino (Research Fellow at Dana-Farber Cancer Institute):
“Biomarker analysis of KN-119 of pembro vs chemo in pretreated mTNBC out in NPJ Breast. Pembro improved OS in pts with TILs ≥5%, no benefit if TILs<5%. Still waiting for the TILs analysis of KN-522, which we hope could refine the use of neoadjuvant pembro.”
Lorenza Rimassa (Associate Professor of Medical Oncology at Humanitas University):
“Unprecedented 5-yr overall survival rate for patients with advanced HCC treated with STRIDE. immunotherapy tremelimumab durvalumab Humanitas University Humanitas Research Hospital Journal of Hepatology.”
Yan Leyfman (Medical Oncologist, Co-Founder and Executive Director of MedNews Week):
“Standing-room-only keynote from global oncology leader Dr. Zihai Li of the Ohio State University Comprehensive Cancer Center-James Cancer Hospital and Solove Research Institute and Pelotonia Institute for Immuno-Oncology (PIIO). Highlighting groundbreaking research on GARP as a promising next-generation target in cancer immunotherapy at the 2025 CAHON New York Oncology Forum. Exciting times ahead for the field!”

Daniëlle Krijgsman (Assistant professor at UMC Utrecht):
“Check out our new publication: “High-plex imaging of hepatoblastoma and adjacent liver in pediatric patients reveals a predominant myeloid infiltrate expressing immune-checkpoints” published in Cancer Immunology, Immunotherapy.
We studied the immune landscape of hepatoblastoma, the most common liver cancer in children.
Key insight: instead of T cells, these tumors are mainly infiltrated with macrophages that carry “brakes” on the immune system (VISTA, SIRPα).
This means that current T cell–focused immunotherapies are unlikely to help hepatoblastoma patients — but targeting macrophages could open new treatment opportunities.
Read more here.”
Shannon McKie-Medd (Director Business Development-International Patient Services at Mass General Brigham):
“Scientists at Harvard Medical School, Massachusetts General Hospital, and the Broad Institute of MIT and Harvard have leveraged CRISPR technology to identify genetic modifications that may enhance the effectiveness of immunotherapy for multiple myeloma.
This innovative approach could pave the way for more personalized and powerful treatments against this challenging blood cancer – a major step toward improving patient outcomes and expanding the potential of gene-based therapies.”
Marco Tagliamento (Assistant Professor at Università degli Studi di Genova):
“Huge meta-analytic work led by Giovanni Rossi exploring the efficacy of neoadjuvant and adjuvant IO in resectable NSCLC in different disease subgroups. Happy to have contributed Link.”
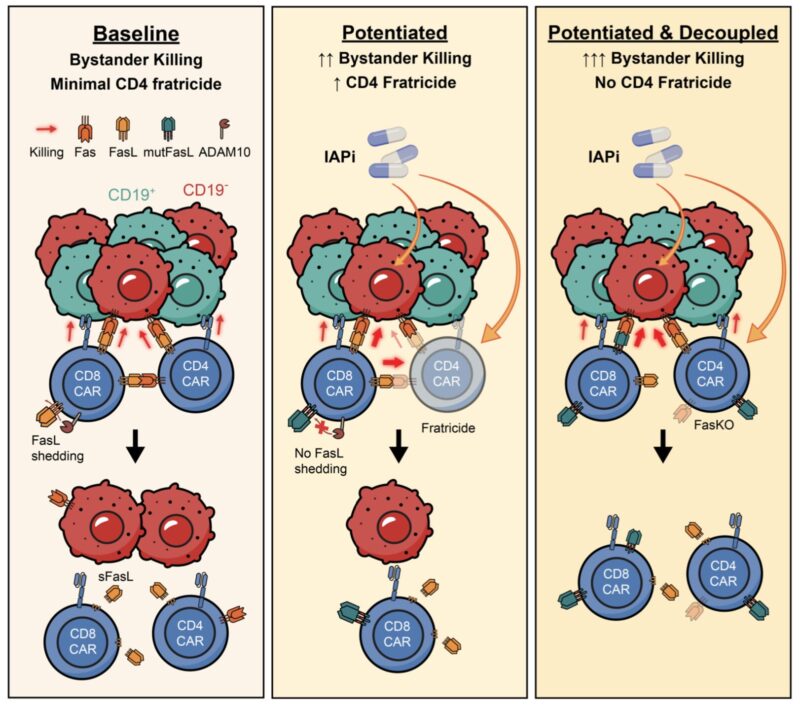
John Gordon (co-Founder, Director, VP Scientific Affairs at Celentyx Ltd):
“CARTcellTherapy | Potentiating CART bystander killing by enhanced hashtag#Fas ↔ FasL signalling ↑ mitigates AntigenEscape in Heterogeneous Tumours ↓ | Major Advance from Joshua Brody, & Friends in Breaking Preprint at BioRxiv |
Antigen (Ag) escape is a frequent mechanism of relapse after CAR-T therapy, even though only ~1% of leukemic and ~0.1% of lymphoma cells are Ag⁻ at baseline.
Here*, Joshua Brody, together with colleagues Matthew Lin, Joanna Chorazeczewski, Gvantsa Pantsulaia, Alan Cooper, et al modelled extreme Ag heterogeneity (>20%) to define how Fas/FasL-dependent bystander killing contributes to tumour clearance.
Across patient cohorts, Fas expression predicted survival after CD19 CAR-T therapy, particularly in CD19-low disease. In both murine and human systems, Fas-dependent bystander killing required Ag stimulation and cell contact, operated within a defined therapeutic window, and could eradicate large fractions of Ag⁻ tumors in vivo.
Pharmacologic potentiation with inhibitor of apoptosis protein antagonists or genetic stabilization of CAR-T membrane-bound FasL enhanced bystander killing but simultaneously induced CD4⁺ T cell fratricide, which was rescued by CAR-T Fas knockout. Importantly, Fas sensitization also enabled bispecific antibody-redirected T cells to mediate bystander killing in resistant tumors. Finally, targeting tumor-associated macrophages triggered Fas-dependent clearance of neighboring tumor cells.
These findings establish Fas-mediated bystander killing as a generalizable and therapeutically actionable axis to prevent Ag escape and broaden the scope of targeted T cell therapies.”
Alessandro Di Federico (MD. Oncologist & PhD student at IRCCS S.Orsola-Malpighi, University of Bologna. Researcher at Dana-Farber Cancer Institute, Harvard University):
“Chemo-immunotherapy options for pts with stage IV non-small cell lung cancer (NSCLC) may include single PD-(L)1 inhibition or dual PD-(L)1 & CTLA-4 inhibition. However, adding CTLA-4 blockade increases toxicity. Identifying biomarkers to select cases where benefits may outweigh risks is therefore an unmet need.
For this reason, we performed a reconstructed individual patient data meta-analysis aiming to identify populations that may benefit from dual immune checkpoint blockade (ICI) with CTLA-4 and PD-(L)1 inhibition. The full paper has just been published in the Lancet Oncology (The Lancet Group).
We focused on trials that provided 5-year survival updates or subgroup analyses based on KRAS and/or STK11 mutational statuses. Trials included were: CheckMate 227; Checkmate 9LA; POSEIDON; Keynote 189; Keynote 407; IMpower 150.
Despite no survival differences in the overall population, combining CTLA-4 and PD-(L)1 blockade significantly prolonged OS in the PD-L1 <1% population (median OS 15.5 vs 14.5 months with single ICI, HR 0.85, P=0.02). Despite apparently being a modest benefit due to the non-proportionality of HRs, this benefit appeared more evident over time, with 5-year OS rates of 16.6% with dual ICI vs 9.3% with single ICI.
Similarly, in the STK11-mutated population, adding CTLA-4 inhibition to PD-(L)1 blockade prolonged OS (median, 13.9 vs 7.8 months with single ICI, HR 0.67, P=0.01) and roughly doubled the survival rates at 3 years compared to single ICI (28.4% with dual ICI vs 13.4% with single ICI).
Our study confirms recent findings published in Nature Magazine by Ferdinandos Skoulidis et al. of improved outcomes with dual ICI among patients with STK11/KEAP1 mutations, and shows the benefit extends to the population with PD-L1 <1% (~1/3 of all NSCLC cases).”
Written by Rima Grigoryan, MDc, Assistant Editor of OncoDaily IO.


