Evolution of the treatment of metastatic cutaneous melanoma over the past 5 decades
Melanoma is the most aggressive form of skin cancer, and despite being less common than other cutaneous malignancies, it accounts for the majority of skin cancer–related deaths worldwide. For decades, treatment options for advanced melanoma were limited to chemotherapy and high-dose interleukin-2, which offered only modest benefits and were associated with substantial toxicity. Over the past two decades, however, the therapeutic landscape has been transformed by the advent of targeted therapies directed at BRAF and MEK mutations and the development of immune checkpoint inhibitors.
These innovations have not only improved overall survival but have also offered long-term disease control to subsets of patients. Yet, resistance to therapy and disease progression remain significant challenges, highlighting the need for continued clinical research and new treatment strategies. This article provides an overview of conventional approaches, pivotal clinical trials, and recent advances that have reshaped the management of metastatic cutaneous melanoma.
Title: Evolution of the treatment of metastatic cutaneous melanoma over the past 5 decades
Authors: Agop Y. Bedikian
Background
Cutaneous melanoma is the most aggressive form of skin cancer, with historically poor outcomes for patients diagnosed at the metastatic stage. For decades, treatment options were limited to cytotoxic chemotherapy and high-dose interleukin-2, both associated with modest efficacy and significant toxicity. Over the past two decades, the introduction of targeted therapies against oncogenic drivers and immune checkpoint inhibitors has revolutionized the therapeutic landscape, offering patients unprecedented improvements in response rates, survival, and long-term disease control. Despite these advances, the emergence of resistance remains a major clinical challenge, driving ongoing research into novel strategies and combinations.
Methods
This review is based on phase II and III randomized clinical trials, retrospective analyses, and meta-analyses that have investigated chemotherapy, biochemotherapy, targeted therapy, immune checkpoint inhibitors, and novel cellular therapies in patients with metastatic cutaneous melanoma. Special focus was placed on regimens directed at BRAF-mutated melanoma and immune checkpoint blockade, which have defined current standards of care.
Study Design
Historically, dacarbazine (DTIC) served as the comparator in most early clinical trials, with response rates ranging between 5% and 15%. Biochemotherapy regimens, combining DTIC with cisplatin, vinblastine, IL-2, and interferon alfa, demonstrated higher objective response rates (up to 52%) and 10-year survival of 12.5% compared with 5% for chemotherapy alone. However, meta-analyses of over 2,600 patients failed to show an overall survival benefit, limiting adoption.
The discovery of frequent BRAF mutations in melanoma led to a new generation of targeted therapies. Phase III trials compared BRAF and MEK inhibitors, alone and in combination, with dacarbazine or other targeted agents. In parallel, immune checkpoint inhibitors targeting CTLA-4 and PD-1 were tested against standard chemotherapy, demonstrating durable benefits. More recently, studies have focused on treatment sequencing, management of brain metastases, and emerging cellular therapies.
Results
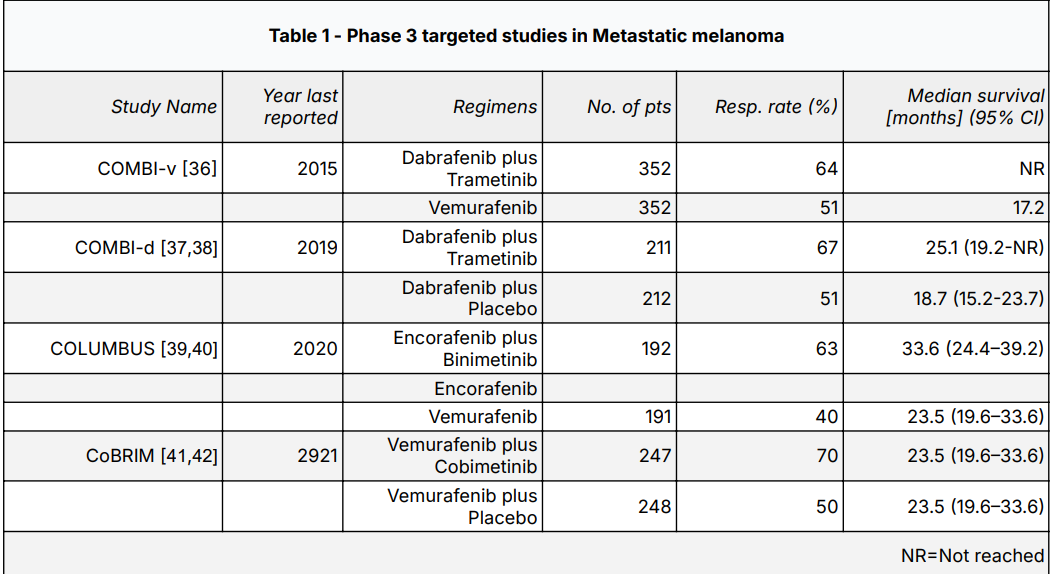
Targeted Therapies
- BRAF inhibitors: Vemurafenib increased response rates to 48% and median overall survival (OS) to 13.3 months compared with 10 months for dacarbazine. Dabrafenib and encorafenib showed similar efficacy.
- MEK inhibitors: Trametinib achieved a median progression-free survival (PFS) of 4.8 months versus 1.4 months with chemotherapy.
- BRAF + MEK inhibitor combinations: Dabrafenib plus trametinib produced an ORR of 67% and median OS of 25.1 months, compared with 51% and 18.7 months for dabrafenib alone. Encorafenib plus binimetinib yielded an ORR of 63% and median OS of 33.6 months. Combination regimens significantly reduced cutaneous squamous cell carcinoma rates compared to BRAF inhibitor monotherapy.
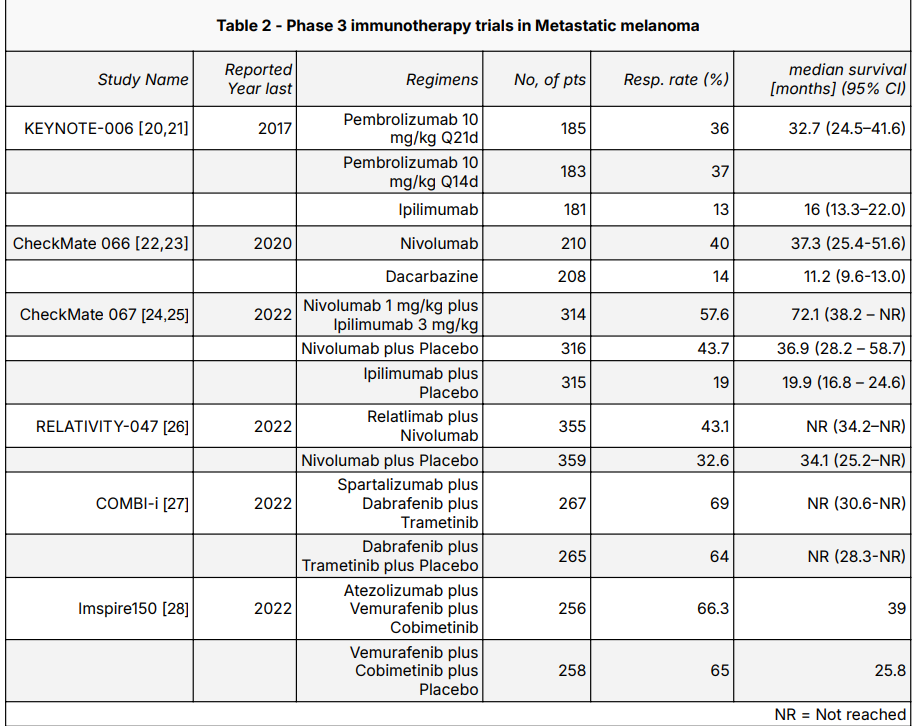
Checkpoint Inhibitors
- CTLA-4 blockade: Ipilimumab improved OS in stage III/IV melanoma, with 2-year survival rates approximately 10% higher than controls. ORR remained modest at 10–15%.
PD-1 inhibitors:
- Nivolumab achieved an ORR of 40% and a median OS of 37.3 months compared with 11.2 months for dacarbazine in CheckMate 066.
- Pembrolizumab (KEYNOTE-006) showed response rates of 36–37% and median OS of 32.7 months, compared to 16 months for ipilimumab.
- Combination regimens: Nivolumab plus ipilimumab in CheckMate 067 achieved an ORR of 57.6% and median OS of 72.1 months, significantly higher than nivolumab alone (36.9 months) or ipilimumab (19.9 months). Relatlimab plus nivolumab further improved progression-free survival compared with nivolumab alone.
Special Situations
- Sequencing therapy: The DREAMseq trial demonstrated superior 2-year survival with upfront immunotherapy (72%) compared to targeted therapy (52%) in BRAF-mutated melanoma, establishing immunotherapy as the preferred initial strategy for most patients.
- Brain metastases: Dabrafenib plus trametinib achieved intracranial response rates of 58% in asymptomatic patients, while nivolumab plus ipilimumab produced intracranial ORRs of 46% versus 20% with nivolumab monotherapy.
- Cellular therapies: Lifileucel (tumor-infiltrating lymphocyte therapy) produced an ORR of 36% in heavily pretreated patients, with durable responses leading to FDA approval in 2024. CAR-T cell therapy remains investigational.
Key Findings
- Chemotherapy and biochemotherapy offered limited long-term benefit, with median OS under 12 months.
- BRAF and MEK inhibitors achieved rapid tumor control, with combination therapy extending OS beyond 30 months in some trials.
- Immune checkpoint inhibitors transformed outcomes, with median OS exceeding 3 years in PD-1 inhibitor studies and over 6 years with dual checkpoint blockade.
- Upfront immunotherapy provides the best survival outcomes in BRAF-mutated melanoma, though targeted therapy remains valuable for patients requiring rapid disease control.
- Lifileucel has introduced a new cellular therapy option, though access and cost remain barriers.
Key Takeaway Messages
- Modern therapies have redefined metastatic melanoma from a uniformly fatal disease to one with meaningful long-term survival in many patients.
- Targeted therapy provides rapid responses but is limited by eventual resistance.
- Immunotherapy offers durable control, with combination regimens achieving survival milestones unthinkable a decade ago.
- Treatment sequencing is critical: most patients with BRAF mutations benefit from upfront immunotherapy unless rapid tumor reduction is clinically necessary.
- Novel approaches—including cellular therapies and next-generation checkpoint inhibitors—are expanding future options.
Conclusion
The treatment of metastatic cutaneous melanoma has evolved dramatically, with targeted therapies and checkpoint inhibitors delivering unprecedented improvements in response and survival. Long-term outcomes are best achieved with immunotherapy, especially in combination regimens, while targeted therapy remains essential in rapidly progressing disease. Cellular therapies such as lifileucel represent the next frontier, though challenges with resistance and accessibility persist. Continued clinical research is essential to further improve survival and address resistance mechanisms, ensuring that advances translate into durable benefit for patients worldwide.
You can read the full article here.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
