Skin cancer is one of the most common forms of cancer worldwide, with melanoma being the most aggressive and deadly subtype. Melanoma originates from melanocytes, the pigment-producing cells in the skin. While it accounts for only about 1% of skin cancers, it is responsible for the majority of skin cancer-related deaths due to its high metastatic potential. According to the American Cancer Society, the estimated number of new melanoma cases in the United States in 2025 is about 104,960, with approximately 8,430 deaths expected. Early detection and proper medical intervention significantly improve survival rates, making public awareness crucial.
What Are the Symptoms of Melanoma?
Melanoma can present itself in various ways, and its symptoms can sometimes be mistaken for benign skin conditions. The most recognizable warning sign is an unusual mole or skin lesion that changes over time. The ABCDE rule is widely used by dermatologists and oncologists to identify potentially malignant moles:
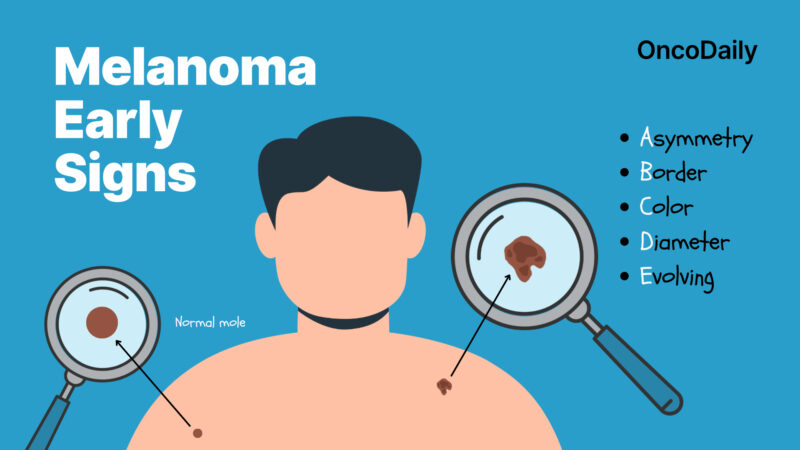
A – Asymmetry: One half of the mole does not match the other half.
B – Border: Irregular, scalloped, or poorly defined edges.
C – Color: Varied shades of brown, black, tan, or even white, red, or blue.
D – Diameter: Larger than 6 mm (about the size of a pencil eraser), though melanomas can be smaller.
E – Evolving: Any noticeable changes in size, shape, color, or texture over time.
Other symptoms of melanoma
Many people recognize melanoma by its irregular shape or unusually dark color, but the disease can also manifest through other, less well-known warning signs. These symptoms can develop gradually or appear suddenly, signaling that something more serious is happening beneath the skin. Being aware of these changes and seeking medical attention early can make a significant difference in treatment outcomes.
- A mole or lesion that itches, bleeds, or becomes tender.
- A fast-growing, raised bump on the skin.
- Pigmentation that spreads beyond the border of an existing mole.
- The appearance of a sore that does not heal.
These symptoms warrant immediate medical evaluation. According to studies published in ASCO and ESMO guidelines, recognizing melanoma early through the ABCDE rule improves prognosis significantly, as early-stage melanoma has a nearly 99% five-year survival rate when treated promptly.
What Are the Early Signs of Melanoma?
Early-stage melanoma can be subtle, often starting as a small, dark spot that gradually enlarges or a changing mole with darkening redness, or irregular borders. It can also appear in uncommon areas like the palms, soles, under nails, or mucous membranes, making early detection crucial. Regular skin checks help identify these warning signs when treatment is most effective.
Since melanoma can sometimes resemble benign conditions like age spots, freckles, or rashes, it is important to differentiate between harmless and potentially dangerous skin changes. Melanoma lesions often exhibit multiple colors and irregular borders, unlike common moles or sunspots. Studies show that in about 70% of early-detected melanoma cases, patients noticed a mole evolving before seeking medical attention, underscoring the importance of self-examination and regular dermatological check-ups.
What Causes Melanoma?
Melanoma is a complex disease that develops when pigment-producing cells, known as melanocytes, begin to grow uncontrollably. Genetic predisposition also plays a significant role, with some individuals inheriting mutations that increase their susceptibility to the disease. In many cases, melanoma arises due to a combination of genetic and environmental influences, making it crucial to understand both aspects when assessing risk and taking preventive measures.
Genetic and Family History Risk Factors
Melanoma has a well-established genetic component, with certain hereditary mutations increasing an individual’s risk of developing the disease. One of the most significant genetic mutations associated with melanoma is in the CDKN2A gene, which encodes proteins responsible for regulating cell growth. Mutations in this gene have been linked to familial melanoma, with studies suggesting that 10-20% of melanoma cases occur in individuals with a family history of the disease. In addition to CDKN2A, mutations in genes like CDK4, BAP1, MITF, and POT1 have been identified in familial melanoma cases.
Research shows that individuals with these mutations often develop melanoma at a younger age and may experience multiple primary melanomas over their lifetime. A 2022 study published in The Journal of Investigative Dermatology found that individuals with CDKN2A mutations have a lifetime melanoma risk of up to 76%.
Those with a family history of melanoma, particularly if multiple first-degree relatives have been affected, should consider genetic testing. A well-documented case study involves a family in Australia with multiple members diagnosed with melanoma due to an inherited CDKN2A mutation. With increased screening and sun protection measures, the younger generations of this family have seen a marked reduction in advanced-stage melanoma diagnoses.
Environmental and Lifestyle Risk Factors
One of the primary environmental triggers of melanoma is ultraviolet (UV) radiation from the sun and artificial sources like tanning beds. Studies have shown that intense, intermittent sun exposure, particularly during childhood, increases the risk of melanoma later in life. According to the World Health Organization (WHO), individuals who use tanning beds before the age of 35 have a 75% increased risk of developing melanoma.
Geographical location also influences melanoma risk, such as Australia, New Zealand, and southern parts of the United States, have significantly higher melanoma incidence rates. A study published by the National Cancer Institute in 2023 reported that Australia has the highest melanoma rate globally, with 1 in 17 Australians diagnosed by age 85. Spending long hours outdoors without proper sun protection, such as sunscreen, protective clothing, or shade, increases exposure to harmful UV rays. Additionally, individuals with weakened immune systems, whether due to organ transplants, HIV, or immunosuppressive medications, are more vulnerable to melanoma.

Sunscreen and Cancer: Separating Myth from Reality with OncoDaily
What Are the Types of Melanoma?
Melanoma comes in different types, each varying in appearance, growth rate, and likelihood of spreading. Understanding these types helps with early detection and appropriate treatment. Melanoma manifests in several forms, each with distinct characteristics.
- Superficial Spreading Melanoma: This is the most prevalent type, accounting for approximately 70% of cases. It typically appears as a flat or slightly raised discolored patch with irregular borders and can occur anywhere on the body.
- Nodular Melanoma: Representing about 15-20% of melanomas, this aggressive form is characterized by a raised, often dark-colored bump. It tends to grow more rapidly than other types.
- Lentigo Maligna Melanoma: Commonly developing in older adults, this type arises in sun-damaged areas like the face and neck. It begins as a flat or slightly elevated mottled tan, brown, or dark brown discoloration.
- Acral Lentiginous Melanoma: Although rare, this type is the most common melanoma in individuals with darker skin tones. It appears on the palms, soles, or under the nails and may be mistaken for other conditions, leading to delayed diagnosis.
What Are the Stages of Melanoma?
Melanoma staging helps determine the severity of the disease and guides treatment decisions. Each stage is classified based on tumor size, ulceration, lymph node involvement, and metastasis.
Stage 0 (In Situ): The melanoma is confined to the epidermis (outermost skin layer) and has not spread. Lymph nodes are not involved. Treatment typically involves surgical excision, and the prognosis is excellent.
Stage I: The tumor is up to 2 mm thick and may or may not be ulcerated. Lymph nodes are not involved at this stage. The primary treatment is wide local excision (surgical removal of the tumor with a margin of healthy tissue). In some cases, a sentinel lymph node biopsy (SLNB) may be performed to check for microscopic spread, especially if ulceration is present.
Stage II: The tumor is greater than 2 mm in thickness, with or without ulceration, but has not spread to lymph nodes. Treatment involves wide local excision, and SLNB is recommended to check for hidden spread. Depending on risk factors, adjuvant therapy with immunotherapy (e.g., nivolumab, pembrolizumab) may be considered to reduce the risk of recurrence.
Stage III: Melanoma has spread to nearby lymph nodes or developed satellite tumors near the original site. Treatment includes surgical removal of the primary tumor and affected lymph nodes, followed by adjuvant immunotherapy or targeted therapy if the tumor has BRAF mutations. In some cases, radiation therapy is also considered.
Stage IV: The melanoma has metastasized to distant organs, such as the lungs, liver, brain, or distant lymph nodes. Surgery is not usually an option, and treatment focuses on systemic therapies like immunotherapy (checkpoint inhibitors: nivolumab, pembrolizumab, or ipilimumab) and targeted therapy (BRAF/MEK inhibitors like dabrafenib and trametinib, if applicable). Chemotherapy is rarely used but may be considered in some cases.
How Is Melanoma Diagnosed?
Diagnosing melanoma requires a combination of clinical examination and advanced testing. A skin examination is the first step, where a healthcare professional carefully inspects the skin for suspicious lesions. If an abnormality is found, dermoscopy—a technique that uses a specialized magnifying tool—provides a clearer view of the lesion’s structure, improving diagnostic accuracy compared to visual inspection alone.
When a lesion appears concerning, a biopsy is performed, where the suspicious tissue is surgically removed and examined under a microscope to confirm malignancy. In more advanced cases, imaging tests such as PET or CT scans help detect possible metastasis. Additionally, genetic testing can identify mutations like BRAF, which can guide treatment decisions, particularly for targeted therapies.
What Are the Treatment Options for Melanoma?
Melanoma treatment depends on the cancer’s stage, location, and genetic profile. Early-stage melanomas are often curable with surgery, while advanced cases require immunotherapy, targeted therapy, chemotherapy, or radiation. The emergence of checkpoint inhibitors and combination immunotherapies has revolutionized melanoma treatment, significantly improving survival rates. For Stage II melanoma (1–4 mm thick), wide excision with 1–2 cm margins is necessary, along with SLNB for staging. High-risk patients may benefit from adjuvant immunotherapy. Stage III melanoma, which involves lymph node spread, requires wide excision, lymph node dissection, and systemic therapy, including PD-1 inhibitors or targeted therapy for BRAF-mutant cases.
In Stage IV melanoma, where cancer has spread to distant organs, treatment focuses on systemic therapies. Immunotherapy, particularly PD-1 and CTLA-4 inhibitors, has revolutionized survival rates, while BRAF/MEK inhibitors provide targeted options for genetic mutations. Radiation and chemotherapy are used in select cases for symptom control. However, each therapy has unique benefits and side effects, making personalized treatment plans essential for optimal outcomes.

Read more about Relatlimab: Novel LAG-3 Immunotherapy uses in Cancer, Side Effects, Dosages, Expectations, and More on OncoDaily.
Surgery for Melanoma
Surgery is the cornerstone of melanoma treatment, aiming to remove the tumor completely while minimizing the risk of recurrence. The standard approach is wide local excision, where the tumor is removed along with a margin of healthy tissue. The size of this margin depends on the tumor’s thickness and location. For melanoma in situ, a 0.5–1 cm margin is recommended, with Mohs surgery as an option for facial lesions.
Thin melanomas (≤1 mm) require a 1 cm margin, as wider resections do not improve survival. Intermediate thickness melanomas (1–2 mm) typically need a 1–2 cm margin, though a 1 cm margin may be acceptable in challenging areas. For thicker tumors (>2 mm), a 2 cm margin is advised, though survival largely depends on whether the cancer has spread. If melanoma has reached the lymph nodes, a sentinel lymph node biopsy (SLNB) helps determine the extent of the disease. If the sentinel node is positive, lymph node dissection may be required.
Certain melanoma types require specialized approaches. Head and neck melanomas may need adjuvant radiation therapy if complete excision is difficult or if recurrence risk is high. Acral and subungual melanomas often require more extensive resections, sometimes needing skin grafts or reconstructive surgery. While surgery is highly effective for early-stage melanoma, risks include scarring, infection, and possible lymphedema if lymph nodes are removed.
You Can Also Watch Dr. Fade Mahmoud on Neoadjuvant Immunotherapy and Evolving Melanoma Treatment Standards on OncoDaily
Immunotherapy for Melanoma
For advanced or metastatic melanoma, immunotherapy has revolutionized treatment, significantly improving survival rates and, in some cases, leading to long-term remission. PD-1 inhibitors, such as Pembrolizumab and Nivolumab (Opdivo), help the immune system recognize and attack cancer cells by blocking the PD-1 pathway. Another key approach involves CTLA-4 inhibitors like Ipilimumab, which enhance T-cell activation and are often combined with PD-1 inhibitors for better outcomes. Immunotherapy can cause side effects, including fatigue, inflammation, and autoimmune reactions, as the immune system becomes more active.
Ongoing research continues to refine immunotherapy, exploring new combinations that boost effectiveness while reducing toxicity, offering hope for even better outcomes in the future.
Learn More About Immunotherapy for Melanoma on OncoDaily.
What Is Prognosis for Melanoma?
Melanoma prognosis largely depends on how early the cancer is detected, the type of melanoma, and the patient’s overall health. Early-stage melanoma (Stage 0 or I) has an excellent prognosis, with survival rates exceeding 90%, while advanced melanoma (Stage III or IV) carries a higher risk of recurrence and metastasis. Factors such as tumor thickness (Breslow depth), ulceration, and lymph node involvement play a significant role in determining outcomes. Fortunately, recent breakthroughs in immunotherapy and targeted therapy have dramatically improved survival rates, particularly for those with metastatic disease.
The survival rate for melanoma varies by stage. When diagnosed in its earliest form (Stage 0), the 5-year survival rate is nearly 100%. Patients with Stage I melanoma still have a 90-95% survival rate, while those with Stage II have about 75-85%, depending on tumor thickness and ulceration. Once the disease reaches Stage III, where it has spread to lymph nodes, survival drops to 50-65%. However, the most dramatic improvement in treatment has been seen in Stage IV melanoma, which was once considered nearly untreatable. Before the advent of modern therapies, the 5-year survival rate for metastatic melanoma was less than 10%, but with checkpoint inhibitors and combination immunotherapy, nearly half of patients can now survive beyond 5-10 years.
How Can You Prevent Melanoma?
Preventing melanoma starts with sun protection, as UV exposure is the leading cause. Using broad-spectrum sunscreen (SPF 30+), wearing protective clothing, hats, and sunglasses, and avoiding peak sun hours can significantly reduce risk. Tanning beds pose a major threat due to concentrated UV radiation, making self-tanning products a safer alternative. Regular skin checks and dermatologist visits are crucial, especially for those with a family history, as early detection leads to high cure rates.
A healthy lifestyle also plays a role. A Mediterranean-style diet, rich in antioxidants, healthy fats, and omega-3s, may help protect against melanoma by reducing inflammation and skin damage. Regular exercise supports immune function, further lowering cancer risk. Combining sun safety, nutrition, and physical activity offers the best defense against melanoma.
What are the latest updates in melanoma?
In March 2024, China’s NMPA approved Tunlametinib (HL-085) as the first targeted therapy for NRAS-mutated advanced melanoma after PD-1/PD-L1 therapy. The phase 2 trial (NCT05217303) showed a 35.8% ORR, 72.6% DCR, 4.2-month PFS, and 13.7-month OS. Developed by KeChow Pharma, this MEK inhibitor targets the MAPK/ERK pathway with improved pharmacokinetics. Among 100 patients, 95 had NRAS mutations, with prior immunotherapy recipients achieving a 40.6% ORR. Common AEs included rash (53%) and dermatitis acneiform (24%), while grade 3+ AEs were mostly asymptomatic. KeChow plans further studies in neurofibromatosis type 1, colorectal, and lung cancers.
A Phase 2 trial (RegoMel, NCT05370807) evaluating regorafenib (REGO) in pretreated advanced melanoma patients was published in JCO on May 29, 2024. Among 16 enrolled patients, the objective response rate (ORR) was 31%, with five partial responses (four confirmed). KIT-mutant melanoma showed the highest response, while BRAF V600-mutant patients benefited from REGO combined with BRAF/MEK inhibitors after progression. Median progression-free survival (PFS) was 11.9 weeks, and overall survival (OS) was not yet reached. No grade ≥4 treatment-related adverse events occurred. The study met its primary endpoint, highlighting REGO’s potential in refractory melanoma.
A Phase I trial is evaluating IL13Rα2 CAR T-cell therapy for patients with stage IIIC or IV melanoma and metastatic solid tumors. Patients receive genetically modified T cells after chemotherapy to target IL13Rα2-expressing cancer cells. The study evaluates safety, tumor response, and cell persistence, with long-term follow-up for up to 15 years.
The Phase I trial (NCT04903119) evaluates the safety and optimal dose of nilotinib combined with dabrafenib/trametinib or encorafenib/binimetinib in patients with BRAF V600-mutant metastatic melanoma who have relapsed on prior BRAF/MEK inhibitor therapy. After a week on the fixed-dose combination, nilotinib is introduced, and all three drugs are administered together. The study assesses toxicity, drug interactions, and pharmacokinetics, with blood samples and biopsies collected to monitor treatment effects.
Written by Mariam Khachatryan, MD
FAQ
Can Melanoma Occur in Areas Not Exposed to the Sun?
Yes, melanoma can develop in areas that receive little or no sun exposure, such as the soles of the feet, palms, under the nails, and even mucous membranes (like the mouth or genitals). This is because genetic factors and other influences, beyond UV exposure, can contribute to melanoma development.
Is Melanoma More Common in Certain Age Groups?
Melanoma can occur at any age, but it is more common in older adults. However, it is also one of the most common cancers in young adults, particularly those aged 25–39. Factors like genetic predisposition and sun exposure history influence risk at different ages.
What Is the Difference Between Melanoma and Other Skin Cancers?
Melanoma is more aggressive than other types of skin cancer, such as basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). While BCC and SCC are typically slow-growing and less likely to spread, melanoma can metastasize rapidly if not detected early, making early diagnosis critical.
How Long Does It Take for Melanoma to Spread?
he rate at which melanoma spreads varies depending on factors like the type, stage, and individual characteristics of the tumor. Some aggressive forms, like nodular melanoma, can spread within weeks to months, while others develop more slowly. Early detection is key to improving outcomes.
What Are the Early Warning Signs of Melanoma?
The ABCDE rule helps identify early melanoma signs: Asymmetry, Border irregularity, Color variation, Diameter larger than 6mm, and Evolving changes in size, shape, or color. Any new or changing moles should be evaluated by a dermatologist.
Does Having Many Moles Increase the Risk of Melanoma?
Yes, having more than 50–100 moles increases melanoma risk. Atypical (dysplastic) moles, which are irregular in shape and color, further raise the risk. Regular skin checks are essential for early detection.
Is Melanoma Treatable If Caught Early?
Yes, early-stage melanoma (Stage 0 or I) is highly treatable, often with surgical removal alone. Survival rates are high if detected early, but advanced-stage melanoma requires more aggressive treatments, including immunotherapy and targeted therapy.
Can Melanoma Be Prevented?
While not all cases can be prevented, reducing UV exposure by wearing sunscreen, protective clothing, and avoiding tanning beds significantly lowers the risk. Regular self-examinations and dermatologist visits help detect melanoma early.