Immunotherapy has revolutionized the treatment of melanoma, particularly for advanced or metastatic cases. By harnessing the body’s immune system, immunotherapy enables more effective targeting and destruction of melanoma cells. This approach is especially significant because melanoma, which can be aggressive and difficult to treat in later stages, has shown improved outcomes with immunotherapy. This article will explore different types of immunotherapy, including checkpoint inhibitors, as well as side effects, success rates, and findings from recent clinical trials that demonstrate its efficacy.
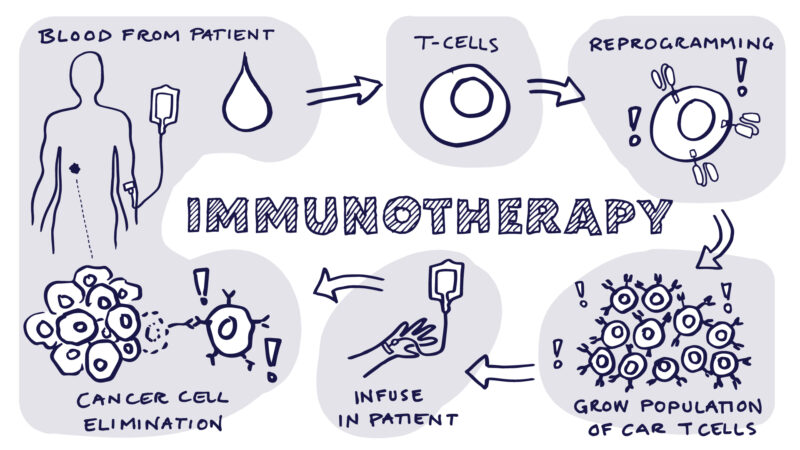
What Is Immunotherapy for Melanoma?
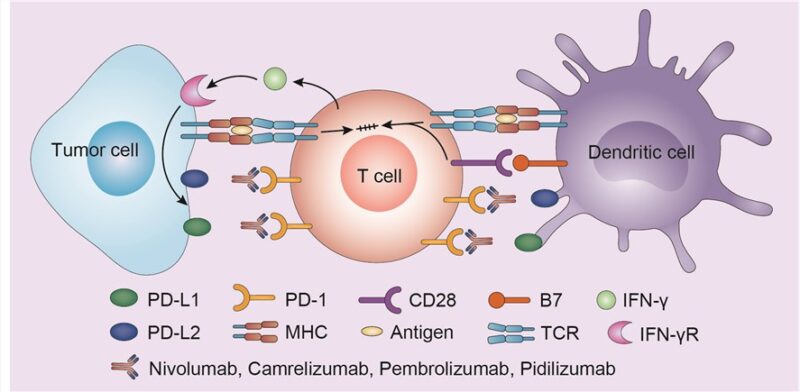
Immunotherapy is a treatment that uses the body’s immune system to identify and destroy cancer cells, including melanoma. Melanoma cells can often evade the immune system, but immunotherapy boosts the body’s natural defenses, helping it to recognize and attack the cancer. One of the primary mechanisms involves checkpoint inhibitors like pembrolizumab or nivolumab, which block proteins (e.g., PD-1) that prevent immune cells (T-cells) from attacking cancer cells. By removing these brakes, immunotherapy strengthens the immune response against melanoma.
What Are the Types of Immunotherapy for Melanoma?
Immunotherapy boosts the immune system to fight cancer through approaches like immune checkpoint inhibitors (e.g., pembrolizumab), cytokines (e.g., IL-2), and cancer vaccines (e.g., sipuleucel-T). Each targets cancer differently, with ongoing research enhancing their effectiveness and safety.
Immune Checkpoint Inhibitors
Nivolumab (Opdivo), pembrolizumab (Keytruda), and ipilimumab (Yervoy) are immune checkpoint inhibitors that work by targeting specific proteins on T-cells to enhance the body’s ability to recognize and fight cancer cells. Nivolumab and pembrolizumab both target PD-1, a receptor on T-cells that, when activated by its ligand PD-L1 found on cancer cells, turns off the immune response. By blocking this interaction, these drugs help keep T-cells active, enabling them to attack tumors. Ipilimumab, on the other hand, targets CTLA-4, another receptor on T-cells, further releasing the brakes on the immune system.
Studies have shown these treatments to be effective in melanoma. The CheckMate 067 trial reported that the combination of nivolumab and ipilimumab had a response rate of 58%, significantly higher than with monotherapy, and led to a 4-year survival rate of 53% for advanced melanoma patients. Pembrolizumab also showed success in the KEYNOTE-006 trial, where it improved overall survival compared to ipilimumab alone. While combination therapies may offer better outcomes, they come with a higher risk of immune-related adverse events .
Cytokines
Interleukin-2 (IL-2), especially high-dose IL-2 (HD IL-2) therapy, has been a key treatment for metastatic melanoma, enhancing T-cells and natural killer (NK) cells to attack cancer cells. Atkins et al. reported a 14% overall response rate for HD IL-2, with 3% achieving complete responses and long-term remissions.
However, due to serious side effects like capillary leak syndrome and organ dysfunction, HD IL-2 is now used less frequently, with checkpoint inhibitors (e.g., nivolumab, pembrolizumab) offering better efficacy and fewer side effects. IL-2 remains an option for patients unresponsive to these newer therapies and may be combined with other treatments to improve outcomes.
Cancer Vaccines
Melanoma vaccines are an emerging form of immunotherapy, designed to help the immune system recognize and attack melanoma cells by introducing specific melanoma-associated antigens. Types include peptide-based vaccines, dendritic cell vaccines, and viral vaccines like Talimogene laherparepvec (T-VEC). T-VEC, an oncolytic viral vaccine, uses a modified herpes virus to destroy cancer cells and stimulate an immune response, with studies showing a 26% overall response rate.
Check out more about novel mRNA vaccine for Melanoma, included in OncoDaily 10 Most Promising Cancer Drugs Not Yet Approved: Solid Tumors

While still in development, melanoma vaccines have shown early promise, providing personalized treatment and potentially long-term immune memory. They are also being studied in combination with checkpoint inhibitors to enhance treatment outcomes, though overcoming challenges like the tumor microenvironment remains a focus of ongoing research.
What Is the Success Rate of Immunotherapy for Melanoma?
Immunotherapy has significantly improved the treatment outcomes for melanoma, particularly in advanced stages. Success rates for immunotherapy vary, but many patients experience prolonged survival and remission. For metastatic melanoma, immune checkpoint inhibitors like nivolumab and pembrolizumab have been shown to improve overall survival, with many patients achieving long-term remission. In early-stage melanoma, immunotherapy helps reduce the risk of recurrence, offering a promising option for preventing disease progression. These therapies have transformed melanoma treatment by providing durable responses and improved quality of life for patients.
Success Rates for Early-Stage Melanoma
According to a study by Luke et al. in The Lancet Oncology (2022), pembrolizumab significantly reduced the risk of recurrence in high-risk stage II melanoma, achieving a 12-month recurrence-free survival rate of 90.5%. Similarly, Weber et al. in The New England Journal of Medicine (2017) reported that nivolumab improved 2-year recurrence-free survival to 63% in stage III and IV melanoma patients compared to 50% with ipilimumab, showing the effectiveness of immunotherapy in early-stage melanoma.
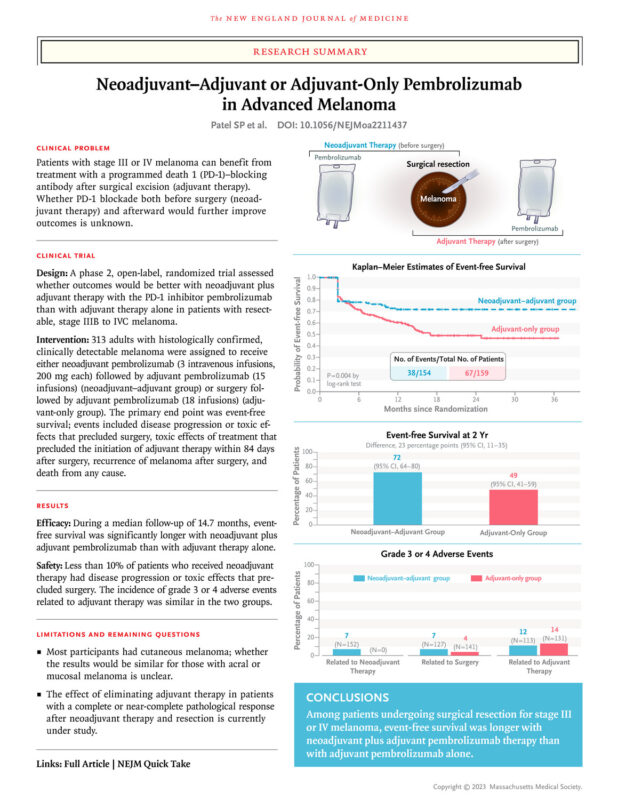
Neoadjuvant therapy, where immunotherapy is administered before surgery, has shown promise in high-risk melanoma cases. The SWOG1801 trial demonstrated improved event-free survival (72% vs. 49%) with neoadjuvant pembrolizumab. Studies like PRADO and OPACIN-neo have also shown that combinations like ipilimumab and nivolumab resulted in major pathologic responses, correlating with better long-term outcomes. This approach reduces tumor burden and improves surgical outcomes, especially in high-risk cases.
Success Rates for Metastatic Melanoma
According to Larkin et al., in a study published in The New England Journal of Medicine in 2019, the CheckMate 067 trial combining nivolumab and ipilimumab showed a 5-year overall survival rate of 52% for patients with advanced melanoma. This marked a significant improvement over older therapies, with some patients experiencing durable long-term remission.
Similarly, according to Robert et al., published in The Lancet Oncology in 2020, the KEYNOTE-006 trial reported a 5-year survival rate of 43% in patients treated with pembrolizumab. Many patients experienced durable remission, remaining progression-free for years, highlighting the transformative potential of immunotherapy.
These treatments have also improved quality of life, as noted in both trials. Although side effects are significant, they are often manageable, with fewer long-term complications compared to traditional chemotherapy.
What Are the Side Effects of Immunotherapy for Melanoma?
Immunotherapy for melanoma can cause a range of side effects, both common and serious. Common side effects include fatigue, skin rash, and diarrhea, which can vary in intensity but are generally manageable with supportive care. More serious side effects, such as autoimmune reactions, can occur when the immune system attacks healthy tissues, leading to complications like colitis or hepatitis. Close monitoring is crucial throughout treatment to manage these side effects early and adjust the therapy as needed, ensuring the patient’s safety and overall well-being.
Common Side Effects
Common side effects of immunotherapy for melanoma include fatigue, nausea, and skin issues, all of which can significantly impact patients’ daily lives.
- Fatigue is one of the most prevalent side effects, affecting up to 30-50% of patients. Many patients report persistent tiredness that interferes with regular activities, often requiring adjustments to their lifestyle and routines.
- Nausea is another frequent issue, with about 20-30% of patients experiencing mild to moderate nausea. It is usually less severe than the nausea associated with chemotherapy, and anti-nausea medications can help manage it.
- Skin issues, including rashes and itching, affect up to 40% of patients. These side effects are usually mild and can be treated with topical creams or corticosteroids, but in some cases, they can become more severe, requiring systemic treatment.
Understanding the prevalence and managing these common side effects early helps improve the patient’s overall experience during treatment. You can Read OncoDaily Special Article on Immunotherapy Side Effects
Serious Side Effects
More serious side effects of immunotherapy include autoimmune reactions and infusion reactions, which require close monitoring due to their potential severity.
- Autoimmune reactions occur when the immune system, stimulated by the treatment, mistakenly attacks healthy organs. This can lead to conditions such as colitis (inflammation of the colon), hepatitis (liver inflammation), pneumonitis (lung inflammation), or thyroiditis (thyroid inflammation).
- Infusion reactions are another serious side effect that can occur during or immediately after receiving immunotherapy. Symptoms may range from mild issues, like fever and chills, to more severe complications, such as anaphylaxis, hypotension, and difficulty breathing. In one reported case, a patient experienced a severe infusion reaction during pembrolizumab treatment, which included shortness of breath and a significant drop in blood pressure, requiring immediate medical intervention.
Both of these side effects highlight the importance of monitoring patients closely throughout treatment and intervening quickly to mitigate risks.
Immunotherapy for Stage 4 Melanoma
For stage 4 melanoma, treatment options have evolved significantly with the introduction of immunotherapies and targeted therapies. Immunotherapy drugs, such as nivolumab (Opdivo), pembrolizumab (Keytruda), and ipilimumab (Yervoy), are used to boost the immune system’s ability to fight cancer. These treatments have shown promising results, with some patients achieving long-term remission and extended survival. For patients with specific genetic mutations like BRAF, targeted therapies like vemurafenib and dabrafenib offer another option. While treatment effectiveness varies based on individual factors, these therapies have significantly improved outcomes compared to traditional chemotherapy.
Combination Therapies
Combination therapies, particularly the use of nivolumab (Opdivo) with ipilimumab (Yervoy), have significantly improved outcomes for patients with advanced melanoma. These therapies target different immune checkpoints—nivolumab blocks the PD-1 receptor, while ipilimumab inhibits CTLA-4—helping to amplify the immune system’s ability to detect and destroy cancer cells.
The effectiveness of this combination has been demonstrated in multiple studies, showing higher response rates and longer survival compared to single-agent treatments. Patients treated with the combination therapy experience durable responses and long-term remission in many cases. However, combination therapy also comes with a higher risk of immune-related side effects, which require careful management but often remain manageable for patients. This dual approach has become a standard treatment for patients with advanced melanoma, offering hope where other treatments may have failed.
Monotherapy Options
Single-agent immunotherapies, such as nivolumab (Opdivo) and pembrolizumab (Keytruda), have shown substantial success in treating stage 4 melanoma, particularly in patients whose tumors express certain biomarkers, like PD-L1. These drugs work by inhibiting the PD-1 receptor on T-cells, which prevents cancer cells from evading immune detection.
Nivolumab has demonstrated long-term survival benefits, with significant numbers of patients achieving durable responses. Studies show that pembrolizumab offers similar effectiveness, with many patients experiencing prolonged periods of disease stabilization or remission. Though single-agent therapies may not be as effective as combination therapies for some patients, they often come with fewer side effects, making them a suitable option for those unable to tolerate the more intense combination regimens. Overall, single-agent immunotherapies have become a key component in managing advanced melanoma, offering improved quality of life and extended survival for many.
How Is Immunotherapy Administered?
Immunotherapy drugs for melanoma, such as nivolumab (Opdivo), pembrolizumab (Keytruda), and ipilimumab (Yervoy), are administered via intravenous (IV) infusions. Infusion times range from 30 minutes to 2 hours, depending on the drug. Pembrolizumab is typically given every 3 or 6 weeks, while nivolumab is administered every 2 to 4 weeks. Treatment duration varies, with some patients continuing therapy for up to 2 years or longer, depending on their response.
Patients are carefully monitored during and after infusions to manage side effects and ensure safety.
What Should Patients Expect During Treatment?
During cancer treatment, patients can expect a series of steps that may include:
- Initial Consultation: The oncologist will discuss treatment options based on cancer type, stage, and the patient’s health. Diagnostic tests may be performed to assess the tumor’s characteristics.
- Treatment Sessions: Immunotherapy and targeted therapies are typically administered as intravenous (IV) infusions, often in a hospital or outpatient clinic. Sessions can last between 30 minutes to a few hours, depending on the treatment regimen.
- Frequency and Duration: Treatments are usually scheduled every few weeks, depending on the type of drug, and can last from several months to years, depending on the patient’s response.
- Monitoring and Follow-Up: Regular follow-up visits are essential for monitoring side effects and evaluating treatment effectiveness through imaging tests or bloodwork.
- Side Effects: Patients may experience fatigue, skin reactions, or more severe immune-related side effects, which will be managed by their healthcare team.
It’s important for patients to maintain open communication with their doctors to manage any side effects and adjust treatment as necessary.
How Long Does It Take to See Results from Immunotherapy?
The timeline for observing improvements after starting immunotherapy can vary, with changes in tumor size or disease progression typically seen 6 to 12 weeks after treatment begins. Some patients may experience pseudoprogression, where tumors initially appear larger due to immune cell infiltration before shrinking.
In some cases, patients achieve durable responses, with benefits lasting long after treatment ends. The timeline and response depend on factors such as the type of cancer, the patient’s overall health, and the specific immunotherapy used. Regular imaging tests are crucial for monitoring progress and adjusting the treatment plan if needed.
What Are the Costs of Immunotherapy for Melanoma?
Immunotherapy treatments can be costly, ranging from $100,000 to $200,000 per year, depending on the drug and duration. Medications like pembrolizumab (Keytruda) and nivolumab (Opdivo) typically fall within this range. While insurance often covers FDA-approved treatments, patients may still face significant co-pays, deductibles, and out-of-pocket costs, depending on their plan.
Financial assistance programs are available through pharmaceutical companies, non-profits, and government programs. For instance, Merck and Bristol-Myers Squibb offer patient assistance programs for Keytruda and Opdivo, respectively. Non-profits like the Patient Access Network Foundation and CancerCare also provide financial aid for treatment and related expenses. It’s important for patients to discuss cost coverage with their healthcare provider and explore these resources early in the treatment process.
How Does Immunotherapy Compare to Other Treatments for Melanoma?
For melanoma, several treatment options are available, each with distinct advantages and limitations:
- Immunotherapy: Drugs like nivolumab and pembrolizumab boost the immune system to target melanoma cells. It’s particularly effective in advanced stages and can offer long-term survival benefits. However, it can cause immune-related side effects, including colitis and pneumonitis.
- Surgery: Highly effective for early-stage melanoma, surgery involves the physical removal of tumors and can often be curative. However, it is not useful for advanced or metastatic melanoma, where cancer has spread to other organs.
- Chemotherapy: Once a mainstay of treatment for melanoma, chemotherapy is now less commonly used due to the rise of immunotherapy and targeted therapies. It works by killing fast-dividing cells but often comes with significant side effects, such as hair loss, fatigue, and nausea, and has lower long-term survival benefits in advanced melanoma.
- Targeted Therapy: For patients with BRAF mutations, targeted drugs like dabrafenib and trametinib inhibit specific proteins driving cancer growth. This approach is highly effective for BRAF-mutant melanoma but may lead to resistance over time and can cause side effects like fever and skin rashes.
Read more about Immunotherapy Vs Targeted Therapy Article by OncoDaily
What Are the Long-Term Effects of Immunotherapy?
Immunotherapy for melanoma has shown long-term benefits for many patients, particularly in achieving sustained remissions and prolonged survival. One of the key advantages is the potential for durable responses, where patients remain cancer-free or experience significantly delayed progression of the disease for several years after treatment. This is a marked improvement over older treatments, which often provided only short-term relief.
However, the long-term effects of immunotherapy are not always purely positive. Some patients develop chronic immune-related adverse effects, such as fatigue, skin issues, or more severe autoimmune reactions that require ongoing management. Although immunotherapy offers a higher quality of life compared to traditional chemotherapy, these long-lasting side effects must be carefully monitored, with regular follow-ups to mitigate any long-term health challenges. Despite these risks, immunotherapy remains a cornerstone in the treatment of advanced melanoma due to its ability to offer life-extending benefits in a subset of patients.
Can All Melanoma Patients Receive Immunotherapy?
Key factors for determining eligibility for immunotherapy in melanoma include:
- Melanoma Stage: Immunotherapy is used not only for advanced melanoma (Stage IV) but also for high-risk early stages like Stage IIb and III. For stage III, it is often given after surgery (adjuvant therapy) to prevent recurrence, while in Stage IV, it is a first-line treatment.
- Type of Immunotherapy: Drugs like pembrolizumab and nivolumab are commonly prescribed after surgery, even if PD-L1 levels are low, demonstrating their wide use regardless of biomarker expression.
- Patient Health: The overall health and ability to tolerate side effects are crucial. Performance status, organ function, and existing conditions such as autoimmune diseases can affect eligibility, as these treatments may worsen underlying issues.
These criteria ensure that immunotherapy is applied effectively, balancing benefits with potential risks.
What Research Is Being Done on Immunotherapy for Melanoma?
Current research in melanoma treatment is rapidly advancing, focusing on improving immunotherapy outcomes through new drugs, combination therapies, and personalized approaches. New checkpoint inhibitors are being explored, targeting pathways beyond PD-1 and CTLA-4, such as LAG-3 and TIGIT. For example, relatlimab, a LAG-3 inhibitor, combined with nivolumab has shown promising results in boosting the immune response, as demonstrated in the RELATIVITY-047 trial for advanced melanoma.
Trials are testing combination therapies, such as nivolumab with relatlimab, and combining immunotherapy with targeted therapies like BRAF and MEK inhibitors to improve outcomes for patients with BRAF mutations. Researchers are also investigating personalized cancer vaccines and CAR T-cell therapy, which show promise in patients resistant to standard treatments. Additionally, novel cytokine-based therapies (like engineered IL-15 and IL-2 variants) are being tested to enhance immune responses while minimizing toxicity. These advancements aim to increase survival rates, improve response durability, and overcome resistance, particularly through combination approaches.
How Can Patients Support Their Immune System During Treatment?
Supporting the immune system during immunotherapy can enhance treatment outcomes and help manage side effects. Here are a few key lifestyle changes and dietary adjustments that can be beneficial:
- Balanced Diet: Focus on nutrient-rich foods like fruits, vegetables, whole grains, and lean proteins. These provide essential vitamins and minerals, such as vitamins C and D, zinc, and antioxidants, which support immune function.
- Stay Hydrated: Drinking plenty of water is essential to keep your body functioning properly, especially during cancer treatment. Adequate hydration helps flush out toxins and supports overall health.
- Moderate Exercise: Regular physical activity, like walking or yoga, can improve circulation and immune function. Consult your healthcare provider before starting any exercise routine.
- Rest and Sleep: Quality sleep is critical for immune health. Aim for 7-9 hours of restful sleep per night to help your body recover and maintain strength.
- Reduce Stress: Chronic stress weakens the immune system. Techniques like meditation, deep breathing exercises, and mindfulness can help manage stress levels and improve overall well-being.
- Supplements: Some patients may benefit from supplements like vitamin D or probiotics, but it is essential to consult your doctor before starting any new supplements, as they can interact with treatments.
Following these strategies can help improve your body’s response to immunotherapy and overall health during treatment. Always coordinate with your healthcare team to ensure that your lifestyle changes are appropriate for your specific situation.
Learn more about Immunotherapy with PodCast series The Immuno-Oncology Curve by Immunotherapy Pioneer, Dr Steven O’Day
FAQ
What Is Neoadjuvant Immunotherapy for Melanoma?
Neoadjuvant immunotherapy involves administering immune-based treatments before surgery to reduce tumor size and improve surgical outcomes. For melanoma, this approach has shown promise, helping patients achieve longer event-free survival rates by targeting the tumor early and improving immune response.
Can Metastatic Melanoma Be Cured with Immunotherapy?
While a complete cure for metastatic melanoma remains challenging, immunotherapy has significantly improved survival rates and remission potential. Many patients experience durable responses, extending survival and enhancing quality of life.
How Much Does Immunotherapy Cost for Melanoma?
Immunotherapy treatments can range from $100,000 to $200,000 annually, depending on the drug and treatment duration. Patients are encouraged to explore financial assistance programs and discuss options with their healthcare team to manage these costs.
Is Immunotherapy Effective in Early-Stage Melanoma?
Yes, immunotherapy has been shown to reduce recurrence risk in early-stage melanoma, especially for high-risk cases. Adjuvant treatments like pembrolizumab and nivolumab are often used after surgery to lower the chance of melanoma returning.
What Side Effects Are Common with Melanoma Immunotherapy?
Common side effects include fatigue, skin rashes, and gastrointestinal issues. Serious side effects, such as autoimmune reactions, can occur, making close monitoring essential to managing these effects during treatment.
How Is Immunotherapy Different from Chemotherapy for Melanoma?
Immunotherapy enhances the body’s natural defenses to fight cancer, while chemotherapy kills fast-growing cells directly. Immunotherapy generally has fewer long-term side effects and offers the potential for durable remission, especially in advanced melanoma cases.
Can Immunotherapy Be Used with Other Treatments for Melanoma?
Yes, immunotherapy is often combined with targeted therapies or other drugs, like immune checkpoint inhibitors, for enhanced effectiveness. Combining treatments can improve outcomes but may increase the risk of side effects.
What Lifestyle Changes Can Support the Immune System During Treatment?
Patients undergoing immunotherapy should prioritize a balanced diet, regular hydration, moderate exercise, quality sleep, and stress reduction. Consulting with healthcare providers ensures these changes complement the treatment effectively.
How Long Does It Take to See Results from Immunotherapy?
Response times vary, but significant changes are often seen within 6 to 12 weeks. Some patients may experience an initial increase in tumor size, known as pseudoprogression, before improvement occurs.
Are There Financial Assistance Programs for Immunotherapy Patients?
Yes, pharmaceutical companies, non-profits, and government programs offer financial assistance to help manage treatment costs. Patients should inquire about these options through their healthcare provider early in the treatment process.
Written by Toma Oganezova, MD