Targeted therapy vs immunotherapy is a big debate and huge advancement in cancer treatment. Targeted therapy focuses on specific proteins or genes that promote cancer growth, offering a highly precise approach. Immunotherapy, by contrast, boosts the immune system’s ability to recognize and attack cancer cells. Understanding these differences is essential for personalized cancer care, as each approach has distinct mechanisms, success rates, and side effect profiles.
This article will explore both therapies in depth, including mechanisms, success rates, side effects, and costs, supported by the latest clinical research findings.
What Is Targeted Therapy?
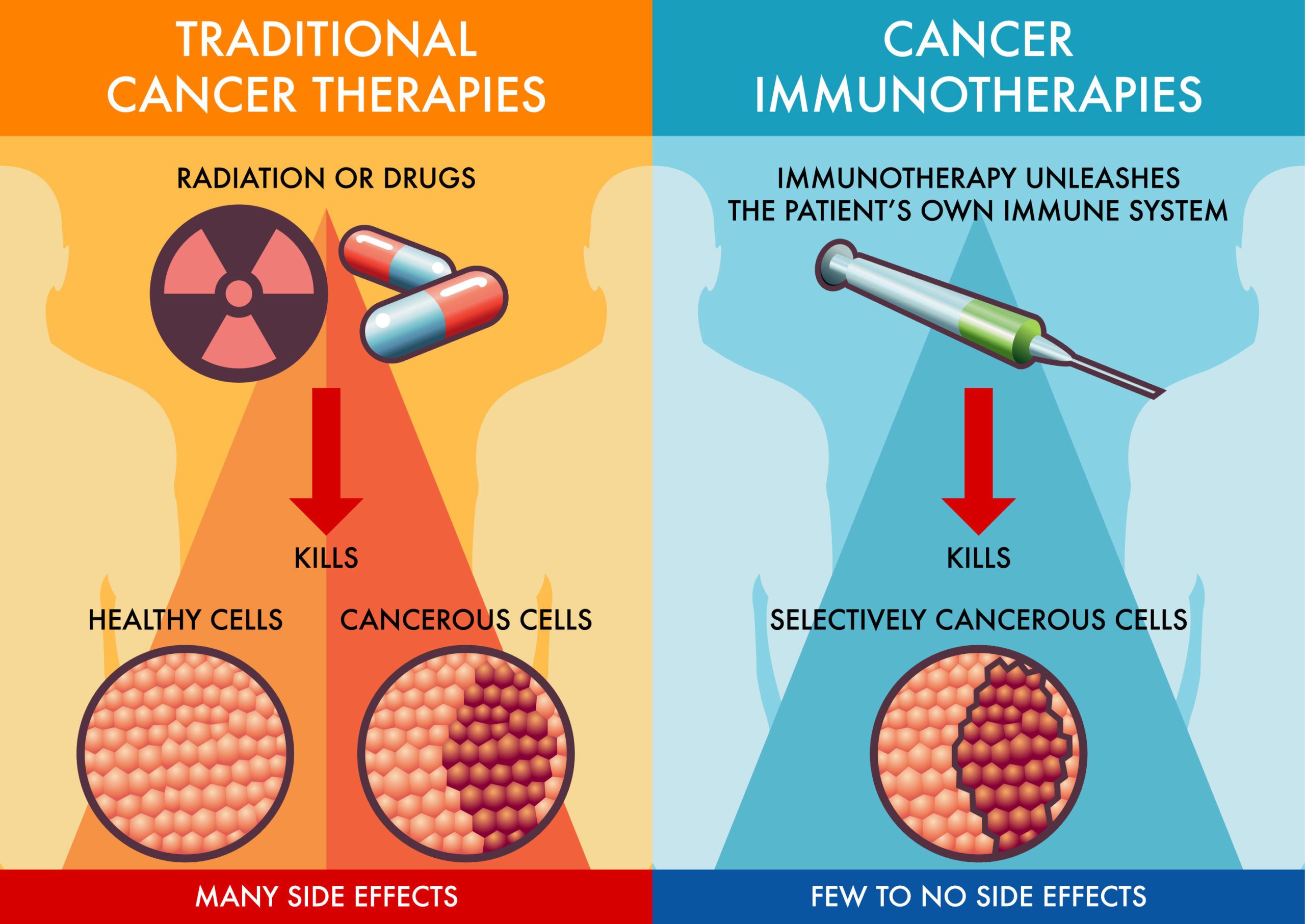
Targeted therapy is a novel cancer treatment that specifically attacks cancer cells by focusing on certain genes, proteins, or the environment surrounding a tumor. Unlike traditional chemotherapy, which indiscriminately affects all rapidly dividing cells, targeted therapy zeroes in on molecular changes unique to cancer. This precise approach often leads to fewer side effects.
Mechanism of Action
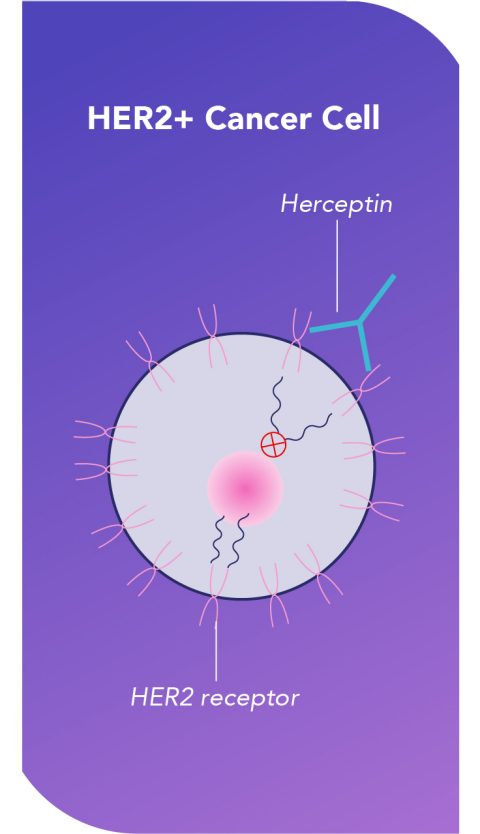
- Monoclonal Antibodies: Lab-made proteins, like trastuzumab (Herceptin), bind to specific cancer cell antigens, such as the HER2 protein in HER2-positive breast cancer, blocking growth signals and marking the cells for immune destruction.
- Small Molecule Inhibitors: These drugs, such as erlotinib (Tarceva), penetrate cancer cells and block key proteins like EGFR in lung cancer, slowing or stopping cell growth.
By targeting specific cancer pathways, this therapy offers a more personalized treatment. However, its success largely depends on the presence of certain biomarkers, making genetic testing an essential part of the treatment plan.
What Is Immunotherapy?
Immunotherapy harnesses the power of the immune system to fight cancer more effectively. It either stimulates the immune system to work harder or teaches it to recognize cancer cells as dangerous, which it might not do naturally.
Mechanism of Action
- Checkpoint Inhibitors: Drugs like pembrolizumab (Keytruda) block proteins such as PD-1 and PD-L1, which cancer cells use to hide from immune attacks. By inhibiting these checkpoints, T-cells can destroy the cancer cells.
- Cancer Vaccines: These vaccines encourage the immune system to target cancer-specific antigens.
- CAR T-cell Therapy: A breakthrough for blood cancers like leukemia, CAR T-cell therapy modifies a patient’s T-cells to recognize and destroy cancer cells.
Immunotherapy vs targeted therapy brings different advantages: while targeted therapy attacks the cancer directly, immunotherapy works by enabling the immune system to identify and fight cancer more efficiently. Immunotherapy is particularly effective in cancers like melanoma and triple-negative breast cancer, providing long-term survival benefits, although immune-related side effects need careful management.
Read More on Latest Approval of T cell Therapy called Afami-Cel
How Do Targeted Therapy vs Immunotherapy Differ in Their Mechanisms?
Targeted therapy and immunotherapy represent two highly advanced yet distinct approaches to cancer treatment.
- Targeted Therapy: This treatment focuses on specific molecular targets that are essential for cancer cell growth and survival. Drugs like trastuzumab for HER2-positive breast cancer and erlotinib for lung cancer directly block growth signals or disrupt cellular processes. The result? A more personalized approach that spares healthy cells but may require combination therapies as cancer cells can develop resistance over time.
- Immunotherapy: On the other hand, immunotherapy activates the immune system to recognize and destroy cancer cells, which often evade detection. Checkpoint inhibitors (like pembrolizumab) unlock immune responses, while CAR T-cell therapy genetically reprograms T-cells to hunt cancer. Immunotherapy offers long-term responses but has a more unpredictable side effect profile, often related to immune overactivity.
In the ongoing discussion of targeted therapy vs immunotherapy, these two therapies may be used alone or in combination, depending on the type of cancer. Researchers continue to explore combining both therapies for diseases like melanoma and lung cancer, aiming to leverage the benefits of both approaches.
Success Rates: Targeted Therapy vs Immunotherapy
The success rates of targeted therapy vs immunotherapy in cancer treatment are heavily influenced by tumor type and the presence of specific biomarkers. For example, in HER2-positive breast cancer, a landmark study by Piccart-Gebhart et al., published in The New England Journal of Medicine (2005), demonstrated that combining trastuzumab (Herceptin) with chemotherapy boosted 5-year survival rates to over 90% and reduced cancer recurrence by 50%.
In EGFR-mutated non-small cell lung cancer (NSCLC), the FLAURA trial (Soria et al., The New England Journal of Medicine, 2018) revealed that osimertinib extended progression-free survival (PFS) to 18.9 months, offering significant improvements over previous treatments.
On the immunotherapy side, treatments like pembrolizumab have delivered notable results, especially in triple-negative breast cancer (TNBC). In the KEYNOTE-355 trial, Schmid et al. (2020, The Lancet) found that pembrolizumab improved overall survival to 23 months in PD-L1-positive TNBC patients, showcasing the power of biomarker-driven approaches in optimizing outcomes.
Targeted Therapy Success Rates
Targeted therapy has revolutionized treatment for cancers like NSCLC and BRAF-mutated melanoma, offering better survival outcomes with fewer side effects compared to chemotherapy.
- Non-Small Cell Lung Cancer (NSCLC): In the FLAURA trial (Soria et al., The New England Journal of Medicine, 2018), osimertinib, an EGFR inhibitor, extended progression-free survival to 18.9 months and overall survival to 38.6 months in patients with EGFR mutations. Many experienced long-term remission and improved quality of life.
- BRAF-Mutated Melanoma: According to Long et al., published in The Lancet (2016), the combination of dabrafenib and trametinib resulted in a 3-year overall survival rate of 45%. Some patients saw long-term remission with minimal disease progression, underscoring the potential for durable outcomes.
These success rates highlight the effectiveness of targeted therapy in treating specific cancer types, with patients often experiencing fewer side effects and better long-term outcomes.
Immunotherapy Success Rates
Immunotherapy has demonstrated varying success across different cancer types, often leading to long-term survival benefits for patients with advanced cancers.
- Melanoma: Checkpoint inhibitors like pembrolizumab (Keytruda) and nivolumab (Opdivo) have dramatically improved outcomes for metastatic melanoma. Wolchok et al. reported 5-year survival rates of 34-44%, and combination treatments like nivolumab + ipilimumab have yielded even better results, with some patients achieving long-term remission.
- Non-Small Cell Lung Cancer (NSCLC): In the KEYNOTE-024 trial, pembrolizumab extended overall survival to 30 months in PD-L1-positive NSCLC patients, compared to standard therapies. Furthermore, the CheckMate 227 trial showed that nivolumab combined with ipilimumab improved 3-year survival rates to 33%, further establishing immunotherapy’s role in lung cancer treatment.
- Triple-Negative Breast Cancer (TNBC): The KEYNOTE-355 trial demonstrated that pembrolizumabcombined with chemotherapy extended overall survival to 23 months in PD-L1-positive TNBC patients. This represented a significant improvement over chemotherapy alone, highlighting immunotherapy’s growing importance in hard-to-treat cancers.
- Renal Cell Carcinoma: Nivolumab with ipilimumab has transformed the treatment of advanced renal cell carcinoma, improving 5-year survival rates to 52%, according to the CheckMate 214 trial.
- Head and Neck Cancer: The KEYNOTE-048 trial showed that pembrolizumab improved overall survival to 14.9 months in PD-L1-positive head and neck cancers, showcasing immunotherapy’s versatility across multiple tumor types.
These results, supported by clinical trials in prestigious journals like The Lancet and The New England Journal of Medicine, demonstrate the growing success of immunotherapy vs targeted therapy across various cancer types. However, the effectiveness of immunotherapy often depends on factors such as tumor biology and the presence of biomarkers, reinforcing the need for personalized treatment strategies.
Side Effects: Targeted Therapy vs Immunotherapy
The side effects of targeted therapy and immunotherapy differ in predictability and severity, largely due to their distinct mechanisms.
Targeted Therapy Side Effects tend to be more predictable and manageable. Common side effects include rash, diarrhea, and liver toxicity. Skin problems, such as dryness or irritation, can often be treated with topical steroids. Gastrointestinal issues like diarrhea and nausea may require medication and dietary changes. Long-term side effects are generally limited but may involve ongoing liver function monitoring.
Immunotherapy Side Effects, on the other hand, are less predictable and often involve immune-related adverse events (irAEs). These can include colitis, pneumonitis, and thyroid dysfunction. Severe irAEs may require treatment with corticosteroids or other immunosuppressants. Some long-term side effects, like thyroid problems, may require lifelong management, underscoring the need for ongoing medical supervision.
Common Side Effects of Targeted Therapy
- Skin Problems: Rashes and dryness are frequent side effects of targeted therapies.
- Management: Using topical steroids and moisturizers helps relieve discomfort.
- Fatigue: Many patients experience persistent fatigue, which can limit daily activities.
- Management: Rest, light exercise, and pacing daily tasks can help manage energy levels.
- Gastrointestinal Issues: Diarrhea and nausea are common, sometimes severely impacting quality of life.
- Management: Anti-nausea medications, hydration, and diet adjustments can mitigate these symptoms.
Common Side Effects of Immunotherapy
- Fatigue: Persistent fatigue is common and may not improve with rest alone.
- Management: Light physical activity and adjusting daily routines can help cope with fatigue.
- Skin Reactions: Rashes and itching are often associated with checkpoint inhibitors like pembrolizumab.
- Management: Topical steroids and antihistamines are typically prescribed to manage these reactions.
- Autoimmune Responses: Immunotherapy can trigger irAEs, such as pneumonitis or colitis.
- Management: These conditions are managed with corticosteroids or immunosuppressive treatments, depending on the severity.
Monitoring these side effects regularly helps ensure timely management, improving patient quality of life during treatment.
Watch MASCC highlights about Immunotoxicity on Oncodaily Youtube Channel.
Costs: Targeted Therapy vs Immunotherapy
The cost of cancer treatment can be a major factor when deciding between targeted therapy vs immunotherapy. While both options are highly effective, they come with different price tags and financial implications.
- Targeted Therapy: Typically ranges from $10,000 to $15,000 per month, depending on the specific drug used. For example, trastuzumab (Herceptin) for HER2-positive breast cancer is in this range, and the costs can accumulate over long-term use.
- Immunotherapy: Generally more expensive, with treatments like pembrolizumab (Keytruda) costing around $150,000 per year. Other immunotherapy options, such as nivolumab (Opdivo), can also exceed $10,000 per dose, with patients requiring multiple doses throughout the treatment.
Insurance Coverage: Most insurance plans cover FDA-approved therapies, but patients often face out-of-pocket expenses, including copays, deductibles, and coinsurance. These costs can vary significantly based on the patient’s insurance plan and the duration of treatment.
Financial Assistance: Many pharmaceutical companies and non-profits offer co-pay assistance and patient financial support programs to help alleviate the financial burden. Cancer treatment centers also provide financial counseling to help patients explore these options and apply for assistance.
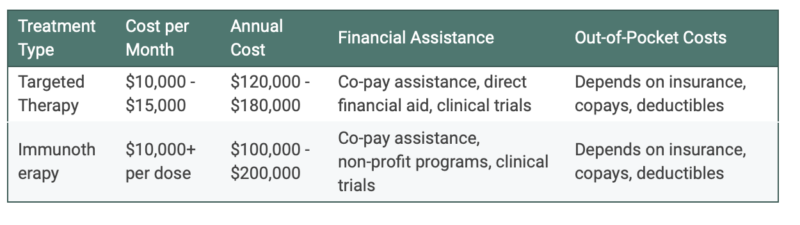
Cost of Targeted Therapy
The cost of targeted therapies can vary based on several factors, including the specific drug, treatment duration, and whether it’s part of a combination therapy. On average, patients can expect costs between $10,000 and $15,000 per month.
- Drugs like trastuzumab (Herceptin) for HER2-positive breast cancer and osimertinib for EGFR-mutated lung cancer fall within this price range.
- Newer targeted therapies tend to be more expensive, but they often provide more personalized and effective treatment options. While many insurance plans cover targeted therapies, patients still face out-of-pocket expenses, which can include significant copays and deductibles.
Financial assistance programs, such as those offered by pharmaceutical companies, can help reduce these costs. Patients may also have access to clinical trials, which often provide these treatments at a reduced cost or for free if eligibility requirements are met.
Cost of Immunotherapy
Immunotherapy is known for its high cost, with treatment expenses typically ranging from $100,000 to $200,000 per year. For example:
- Pembrolizumab (Keytruda) and nivolumab (Opdivo) are two widely used immunotherapy drugs, both of which cost over $10,000 per dose.
- Treatment often involves multiple doses over the course of several months or years, significantly increasing the overall cost.
Factors like treatment duration, the specific drug regimen, and individual insurance plans will ultimately affect the patient’s final out-of-pocket costs. Fortunately, financial assistance programs, including those provided by non-profit organizations, can help mitigate these expenses.
Additionally, clinical trials can offer access to cutting-edge immunotherapy treatments at little to no cost, giving eligible patients a valuable alternative.
The financial burden of both targeted therapy vs immunotherapy can be significant, but there are many resources available to assist patients. Pharmaceutical companies, non-profits, and cancer centers often provide financial aid and co-pay assistance, helping to reduce out-of-pocket costs. While the cost of immunotherapy is generally higher than targeted therapy, both options offer advanced cancer treatment that can improve patient outcomes.
Factors to Consider
When evaluating targeted therapy or immunotherapy, several key factors should guide the treatment choice:
- Tumor Genetics: The presence of specific genetic mutations (e.g., HER2, EGFR) often makes targeted therapy the best option. Immunotherapy, on the other hand, requires the expression of biomarkers like PD-L1 for optimal effectiveness.
- Patient Health Status: Individuals with autoimmune diseases might face higher risks with immunotherapy due to its potential to trigger immune-related side effects. Overall health, organ function, and other pre-existing conditions also influence treatment tolerance.
- Previous Treatments: Past chemotherapy or radiation can affect the success of future treatments, as resistance may develop. In these cases, a combination of therapies might be required to improve outcomes.
- Cancer Stage: For advanced or metastatic cancers, immunotherapy or a combination of treatments is often considered, especially when traditional treatments are less effective.
- Side Effect Profiles: Patients might opt for a specific therapy based on their ability to handle side effects. Targeted therapy tends to have more predictable and manageable side effects, while immunotherapy may involve more unpredictable immune-related adverse events.
- Patient Preferences: The method of treatment (oral vs. IV), frequency of administration, and overall impact on quality of life also play a role. Patients may prioritize less frequent treatments or prefer therapies that allow them to maintain a higher quality of life.
By weighing these factors, patients and their oncology team can develop a personalized treatment plan that suits their unique needs.
Consulting with Your Oncologist
When considering cancer treatment options, having an informed discussion with your healthcare provider is essential. Here are some questions to guide the conversation:
- Understanding Treatment Goals: Ask, “What is the main goal of this treatment? Is it designed to cure the cancer or control its growth?”
- Effectiveness and Outcomes: “What are the expected success rates for my specific cancer type and stage?”
- Side Effects: Inquire about the most common and severe side effects for each treatment option and how they will be managed.
- Alternatives: “Are there other treatments or combinations that might be more effective for me?”
- Cost and Coverage: Discuss the financial aspects of the treatment, including insurance coverage and out-of-pocket expenses. Ask about available financial assistance programs if needed.
- Clinical Trials: “Are there any clinical trials available that I could participate in?”
- Quality of Life: “How will this treatment impact my daily life, and what can be done to maintain my well-being during treatment?”
By asking these questions and reviewing all options, you’ll be able to make a more informed decision about which treatment is right for you.
FAQ
How does targeted therapy vs immunotherapy differ?
Targeted therapy directly targets specific genes or proteins within cancer cells to block their growth. Immunotherapy, on the other hand, activates the body’s immune system to recognize and attack cancer cells.
Can targeted therapy and immunotherapy be combined in cancer treatment?
Yes, combining targeted therapy and immunotherapy is an area of ongoing research. Some cancers respond well to a combination, allowing for both precise targeting and an enhanced immune response.
Which cancers respond better to immunotherapy than targeted therapy?
Cancers such as melanoma, lung cancer, and kidney cancer often respond better to immunotherapy better vs targeted therapy, especially when there are high levels of biomarkers like PD-L1 that indicate an immune response is possible.
What role do biomarkers play in selecting between targeted therapy and immunotherapy?
Biomarkers like HER2 or EGFR are essential for determining the effectiveness of targeted therapy, while PD-L1 is a key biomarker for immunotherapy. These markers help oncologists choose the most effective treatment.
Are the side effects of targeted therapy different from those of immunotherapy?
Yes, targeted therapy tends to have more predictable side effects, such as skin rashes and fatigue. Immunotherapy can cause unpredictable immune-related side effects like colitis, pneumonitis, or thyroid dysfunction.
Is genetic testing required for both targeted therapy and immunotherapy?
Genetic testing is often required for targeted therapy to identify specific mutations that the therapy targets. Immunotherapy typically requires testing for biomarkers like PD-L1 but not for genetic mutations.
How do response rates compare between targeted therapy and immunotherapy?
The response rates for both therapies vary depending on cancer type. For example, targeted therapy can produce rapid responses in cancers with specific mutations, while immunotherapy often provides more durable, long-term responses.
Can patients develop resistance to targeted therapy or immunotherapy?
Yes, cancer cells can develop resistance to targeted therapy by mutating or activating alternative pathways. Immunotherapy resistance can also occur if the cancer cells find new ways to evade the immune system.
How long do the effects of immunotherapy last compared to targeted therapy?
Immunotherapy can result in long-lasting responses, sometimes continuing after treatment stops. Targeted therapy is effective as long as the cancer relies on the specific target, but resistance can shorten the duration of its effect.
How do oncologists decide between using targeted therapy or immunotherapy?
Oncologists use factors like tumor genetics, the presence of specific biomarkers, patient health status, and cancer stage to determine whether targeted therapy or immunotherapy is the best option for treatment.
What are new Targeted and Immunotherapy Drugs in 2024 that can be used in cancer treatment?
In the fast-growing field of oncology, we are witnessing significant advances in several treatment modalities that may soon change how cancer is treated. While not yet FDA-approved, these ten future cancer drugs can hold promise. Read moreabout latest cancer drugs in the article for physicians and patients.

Read also about Immunotherapy Vs Chemotherapy
Written by Toma Oganezova, MD