When comparing immunotherapy vs chemotherapy, it’s important to understand how these cancer treatments work differently. Immunotherapy uses the body’s immune system to target and eliminate cancer cells, making it particularly effective for certain resistant cancers. Chemotherapy, a more traditional cancer treatment, utilizes powerful drugs to kill rapidly dividing cancer cells and is widely used across various cancer types. Understanding the differences between immunotherapy and chemotherapy is crucial for patients and healthcare providers alike. This article delves into their types, success rates, side effects, and costs, providing a detailed comparison based on recent studies.
Immunotherapy vs Chemotherapy: What Are the Key Differences?
Immunotherapy is a novel cancer treatment designed to enhance the body’s immune system, enabling it to better identify and attack cancer cells. Unlike chemotherapy, which directly targets cancer cells, immunotherapy boosts the immune system’s ability to fight cancer naturally.
How Immunotherapy Works: Cancer can evade immune detection because it originates from the body’s own tissues. Immunotherapy changes this dynamic by:
- Checkpoint Inhibitors: These drugs remove the “brakes” that limit the immune response, allowing immune cells to attack cancer more effectively.
- Cancer Vaccines: Stimulate the immune system to recognize cancer-specific markers and trigger an immune attack.
- CAR T-Cell Therapy: Patient’s T-cells are modified to specifically hunt and destroy cancer cells, particularly in some blood cancers.
Chemotherapy: What It Is and How It Compares to Immunotherapy
Chemotherapy employs drugs to destroy fast-dividing cancer cells. It aims to kill cancer cells, shrink tumors, and prevent the spread of the disease.
How Chemotherapy Works: Chemotherapy targets rapidly dividing cells by:
- Disrupting DNA: Chemotherapy interferes with cancer cells’ ability to replicate DNA, preventing them from multiplying.
- Stopping Cell Division: Chemotherapy blocks the processes that cancer cells use to divide and grow.
While chemotherapy is effective across many types of cancer, it also affects healthy cells, leading to side effects. Despite this, chemotherapy remains a cornerstone in cancer treatment.
How Do Immunotherapy and Chemotherapy Differ in Their Mechanisms?
Immunotherapy and chemotherapy are both powerful cancer treatments, but they work differently at the cellular level. Chemotherapy disrupts rapidly dividing cells by inhibiting DNA synthesis and cell division, leading to cell death. However, it is non-selective, affecting both cancerous and normal cells, which leads to common side effects like hair loss and immune suppression.
In contrast, immunotherapy boosts the immune system to fight cancer. Checkpoint inhibitors block proteins that prevent immune cells from attacking cancer, effectively “releasing the brakes” on the immune system. CAR T-cell therapy involves modifying a patient’s T-cells to specifically target and kill cancer cells. Cancer vaccines introduce tumor-associated antigens, helping the immune system recognize and destroy cancer cells.
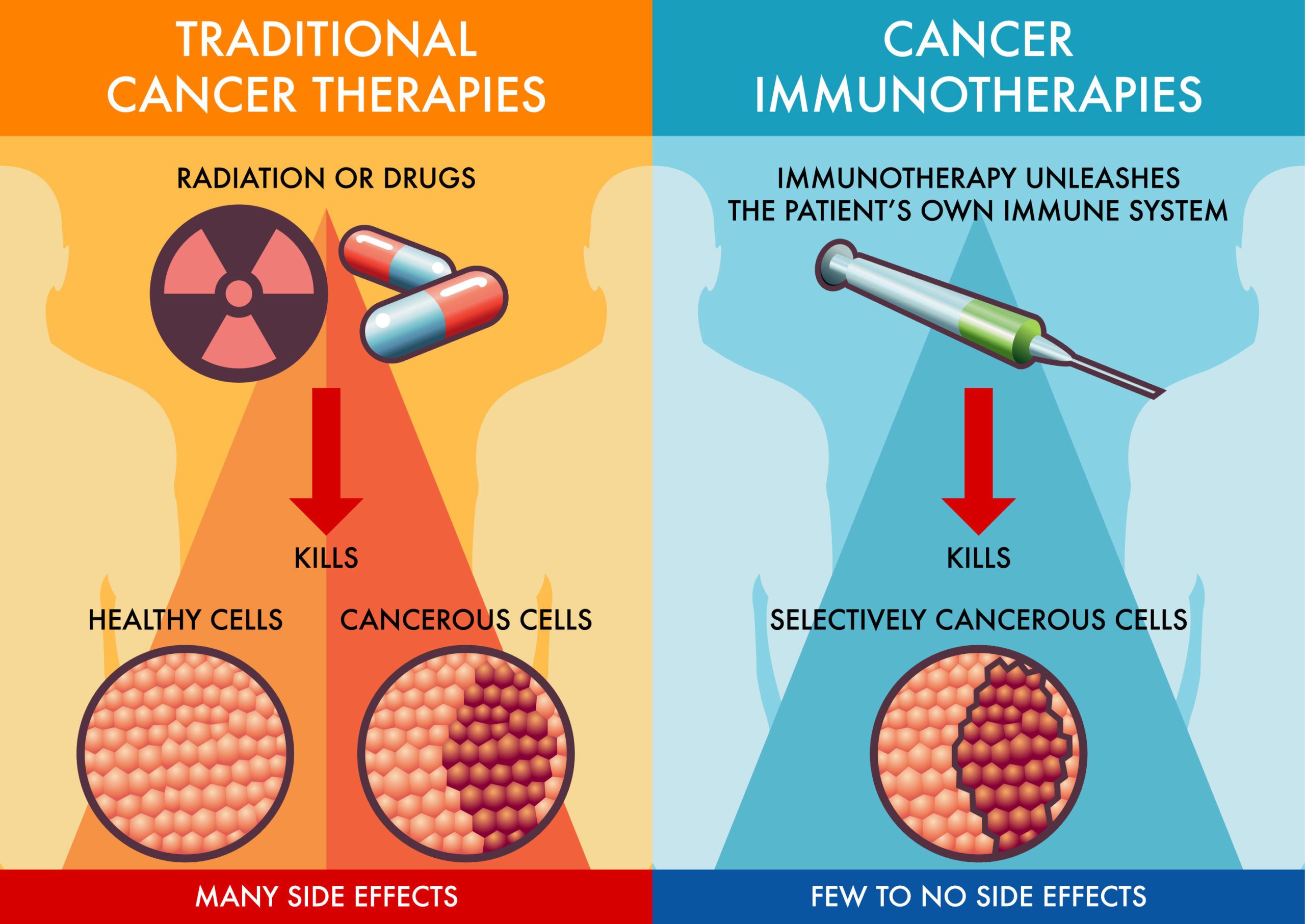
Unlike chemotherapy, immunotherapy is more selective in targeting cancer cells, often resulting in fewer side effects. However, it can still lead to immune-related adverse events due to the immune system’s heightened activity.
Comparing Success Rates of Immunotherapy vs Chemotherapy
The success rates of immunotherapy vs chemotherapy vary significantly depending on the type of cancer. Here’s a comparison of the key findings from recent studies:
How Effective is Chemotherapy for Advanced Melanoma?
- Chemotherapy (Dacarbazine – DTIC): Response rates of 10-20% with median survival of less than one year.
- Immunotherapy (Checkpoint Inhibitors – Pembrolizumab, Nivolumab): Response rates of 30-40%, with five-year survival rates reaching 30-40% (Larkin et al., 2019).
What are the Success Rates of Chemotherapy vs Immunotherapy for Advanced NSCLC?
- Chemotherapy: Response rates of 20-30%, with a median survival of 10-12 months (Schmid et al., 2018).
- Immunotherapy (Pembrolizumab): Response rates of 45%, with median survival extending to 30 months in patients with high PD-L1 expression according to Reck et al., 2018.
Can Immunotherapy Outperform Chemotherapy in Hodgkin Lymphoma?
- Chemotherapy (ABVD regimen): 90% cure rates in early-stage cases, with 70-80% five-year survival in advanced stages (Connors et al., 2018).
- Immunotherapy (Nivolumab): Promising 69% response rates in relapsed or refractory cases (Ansell et al., 2019).
What is the Impact of Immunotherapy vs Chemotherapy in Renal Cell Carcinoma (RCC)?
- Chemotherapy: Typically ineffective, with response rates below 10%.
- Immunotherapy (Nivolumab + Ipilimumab): 42% response rate, with durable outcomes (Motzer et al., 2019).
Triple-Negative Breast Cancer (TNBC): Immunotherapy vs Chemotherapy
- Chemotherapy: 30-40% response rate, with survival under 18 months.
- Immunotherapy + Chemotherapy (Atezolizumab): Improves response rates to 53%, with survival extending to 25 months in PD-L1-positive tumors (Schmid et al., 2018).
These findings highlight how immunotherapy can outperform chemotherapy success rates in certain cancers, offering higher response rates and improved survival.
Immunotherapy Success Rates
Immunotherapy has transformed cancer treatment, improving the outlook for cancers like melanoma, lung cancer (NSCLC), and bladder cancer, giving patients increased hope for long-term survival.
Melanoma
Checkpoint inhibitors such as pembrolizumab and nivolumab have achieved objective response rates (ORRs) of 30-40% in advanced melanoma, with five-year survival rates reaching 30-40%. This represents a substantial improvement over the historical survival rate of less than 10%. Research like the study by Larkin et al. (2019) confirms durable responses in patients treated with nivolumab and ipilimumab combinations.
Lung Cancer (NSCLC)
In NSCLC patients with high PD-L1 expression, pembrolizumab has delivered an ORR of 45%, with a median overall survival of 30 months, compared to 14.2 months for chemotherapy. The KEYNOTE-024 trial demonstrated these significant improvements. Additionally, the KEYNOTE-189 trial found that combining immunotherapy with chemotherapy reduced the risk of death by 51% compared to chemotherapy alone.
Bladder Cancer
For advanced or metastatic bladder cancer, atezolizumab and pembrolizumab have shown ORRs of 15-25%, particularly in patients ineligible for cisplatin-based chemotherapy or those who have progressed post-chemotherapy. Some studies report median overall survival rates of up to 21 months for responders, as supported by research like the Powles et al. study published in the New England Journal of Medicine (2018).
These studies underscore the transformative potential and high immunotherapy success rates, offering significant long-term survival benefits across various cancer types.
Chemotherapy Success Rates
Chemotherapy has long been a cornerstone of cancer treatment, and its effectiveness varies across cancer types and stages. Below is a summary of chemotherapy success rates for various cancers, highlighting key clinical findings:
- Early-stage breast cancer: Adjuvant chemotherapy reduces the risk of recurrence by approximately 30-40%, contributing to a five-year survival rate of over 90% for localized breast cancer.
- Triple-negative breast cancer (TNBC): Chemotherapy remains the primary treatment, with response rates around 30-40%.
- Stage III colorectal cancer: Adjuvant chemotherapy lowers the risk of recurrence by 30%, with a five-year survival rate of roughly 70%. In metastatic cases, modern chemotherapy regimens extend median overall survival to 20-30 months.
- Non-small cell lung cancer (NSCLC): Chemotherapy improves five-year survival by 5-15% in resectable cases, particularly in stages II and IIIA. Advanced NSCLC treated with chemotherapy alone typically shows an ORR of 20-30%, with median survival between 10-12 months.
- Hodgkin lymphoma: The ABVD chemotherapy regimen achieves cure rates exceeding 90% in early-stage disease, with a five-year survival rate over 85-90%. Even in advanced-stage cases, chemotherapy remains effective, with five-year survival rates between 70-80%.
- Testicular cancer: Particularly germ cell tumors respond exceptionally well to chemotherapy, with the BEP regimen curing over 90% of early-stage cases. In metastatic testicular cancer, chemotherapy cures about 70-80% of patients, offering long-term survival.
Chemotherapy continues to be a critical component of cancer treatment, offering substantial survival benefits across a variety of cancers. Despite variability in outcomes, it remains essential in improving survival rates and achieving cures, especially in aggressive or advanced cancers.
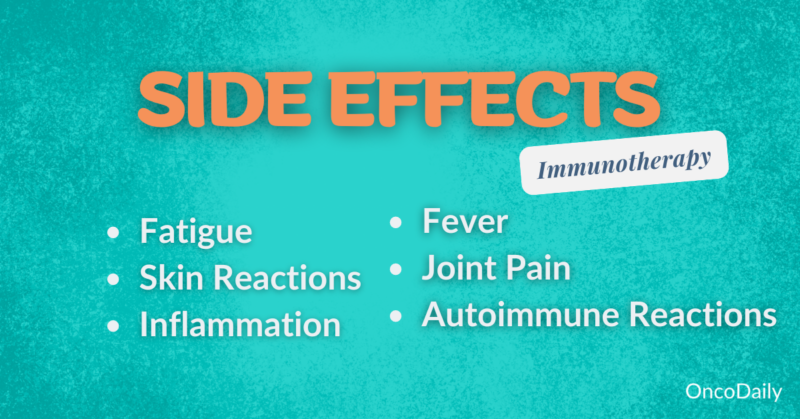
Side Effects: Immunotherapy vs Chemotherapy
When comparing immunotherapy vs chemotherapy, understanding their side effects is crucial for patients choosing between these cancer treatments. Both are effective, but their side-effect profiles differ significantly. Here’s a detailed look at how chemotherapy and immunotherapy impact the body.
Common Side Effects of Immunotherapy
Immunotherapy uses the immune system to target cancer cells, which leads to a different set of side effects. Unlike chemotherapy, immunotherapy’s side effects are more immune-related.
- Fatigue: A common symptom experienced by many patients undergoing immunotherapy, often described as deep, persistent tiredness.
- Management: Energy conservation, light exercise, and proper sleep hygiene can help manage this side effect.
- Skin Reactions: Rashes and itchiness are common as the immune system may mistakenly target skin cells.
- Management: Mild reactions are treated with topical corticosteroids, while severe cases may require oral antihistamines or dermatological consultations.
- Autoimmune Responses: Immunotherapy can trigger autoimmune conditions, where the immune system attacks healthy tissues, leading to conditions such as colitis, hepatitis, or pneumonitis.
- Management: Corticosteroids are typically used to suppress the immune response, with additional immunosuppressants for more severe cases.
While immunotherapy generally results in fewer systemic side effects compared to chemotherapy, the long-term risks include chronic autoimmune conditions that require close monitoring and intervention.
Common Side Effects of Chemotherapy
Chemotherapy targets all rapidly dividing cells, not just cancerous ones, which is why its side effects are often more systemic. Common side effects include:
- Nausea and Vomiting: Chemotherapy often causes nausea and vomiting due to its impact on the gastrointestinal system.
- Management: Medications like ondansetron, dietary changes, and alternative therapies like acupuncture can help alleviate symptoms.
- Hair Loss (Alopecia): Because chemotherapy targets rapidly dividing cells, it affects hair follicles, leading to hair loss.
- Management: Cold caps may help reduce hair loss, and emotional support from counseling can assist with the psychological effects of alopecia.
- Immune Suppression: Bone marrow suppression leads to lower blood cell counts, increasing the risk of infections, fatigue, and bleeding.
- Management: Growth factor injections like filgrastim boost white blood cell counts, while infection prevention and blood transfusions for anemia may be necessary.
Long-term chemotherapy side effects can include organ damage, secondary cancers, and cognitive impairment, commonly referred to as “chemo brain.”
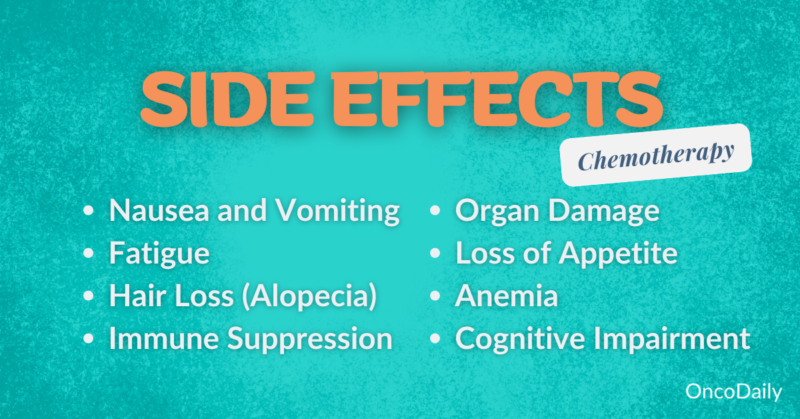
Key Differences in Side Effects: Immunotherapy vs Chemotherapy
- Chemotherapy: Side effects are more immediate and systemic, including nausea, hair loss, and immune suppression, as it targets both cancerous and healthy cells.
- Immunotherapy: Side effects are more related to immune system activity, such as fatigue and autoimmune responses, and are generally less widespread but can still be severe.
Costs: Immunotherapy vs Chemotherapy
The costs of immunotherapy vs chemotherapy treatments can vary significantly depending on factors like the type of treatment, duration, healthcare provider, and geographic location. Below is a detailed comparison of the cost of immunotherapy and chemotherapy, including insurance coverage, out-of-pocket expenses, and financial assistance options.
Cost of Immunotherapy
Immunotherapy is generally one of the more expensive cancer treatments, with annual expenses ranging from $100,000 to $200,000, depending on the specific drug and treatment duration. For example, checkpoint inhibitors like pembrolizumab and nivolumab typically cost around $150,000 per year, while CAR T-cell therapy can exceed $373,000 per treatment.
Most insurance plans, including Medicare and Medicaid, cover FDA-approved immunotherapies, but patients often face significant out-of-pocket costs, such as co-pays and deductibles. Financial assistance is available through patient assistance programs provided by pharmaceutical companies and non-profit organizations. Additionally, clinical trials may offer access to immunotherapy at no cost to the patient.
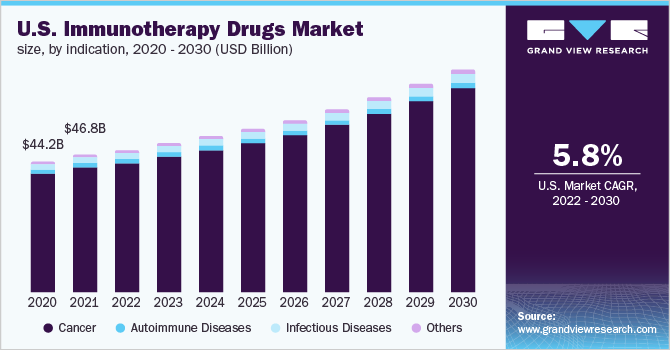
Source: Grand View Research
Cost of Chemotherapy
Chemotherapy is generally more affordable vs immunotherapy, with treatment costs ranging from $10,000 to $50,000 for a full course. Oral chemotherapy can cost between $1,000 and $10,000 per month, while intravenous (IV) chemotherapy typically costs between $1,000 and $5,000 per infusion.
Insurance often covers chemotherapy, but out-of-pocket costs can still accumulate, including co-pays, co-insurance, and the cost of supportive medications required over long treatment periods. Financial assistance is available from organizations such as the Patient Advocate Foundation and HealthWell Foundation, which offer co-pay assistance. Many pharmaceutical companies also provide patient assistance programs to help reduce the cost of chemotherapy drugs. Medicaid and state programs can offer additional support for low-income patients.
Financial Considerations: Immunotherapy vs Chemotherapy Costs
While chemotherapy is typically more affordable than immunotherapy, both treatments represent significant financial burdens for many patients. Accessing financial support and carefully managing treatment-related costs are crucial for those undergoing cancer treatment. For many, immunotherapy’s higher cost is justified by the potential for better outcomes in certain cancers, but chemotherapy remains a cost-effective and widely used treatment.
Which Treatment Is Right for You? Immunotherapy vs Chemotherapy
Choosing between immunotherapy vs chemotherapy depends on factors like cancer type, stage, patient health, and personal preferences. Immunotherapy is often preferred for cancers like melanoma and NSCLC, especially in advanced stages or when biomarkers like PD-L1 are present. Chemotherapy remains a standard option for many cancers, particularly in early stages or when immunotherapy isn’t suitable.
Key Factors in Choosing Immunotherapy or Chemotherapy
- Patient Health: Chemotherapy can be taxing, especially for patients with existing health issues, while immunotherapy may be better tolerated but can still cause immune-related side effects.
- Biomarker Testing: Immunotherapy relies on specific biomarkers like PD-L1, while chemotherapy doesn’t typically require them.
- Side Effects: Chemotherapy tends to cause immediate and widespread side effects like nausea and fatigue. Immunotherapy’s side effects can be delayed but may include serious autoimmune responses.
- Convenience: Chemotherapy usually requires frequent hospital visits, while immunotherapy may offer a more convenient schedule.
- Cost: Immunotherapy is generally more expensive than chemotherapy, though financial assistance programs are available for both.
Source: Medscape
Factors to Consider When Deciding Between Immunotherapy and Chemotherapy
- Tumor Genetics and Biomarkers: Biomarkers like PD-L1, TMB, and MSI help determine if immunotherapy is effective.
- Patient Health: Healthier patients may tolerate aggressive chemotherapy, while those with comorbidities may benefit from less intensive immunotherapy.
- Previous Treatments: Response to previous chemotherapy can influence the choice; resistance may push toward immunotherapy.
- Cancer Type and Stage: Some cancers respond better to immunotherapy, especially in later stages. Early-stage cancers may still be treated with chemotherapy.
- Side Effects: Chemotherapy often causes nausea and fatigue, while immunotherapy can trigger autoimmune conditions. Choose based on your tolerance for side effects.
- Patient Preferences and Lifestyle: Consider whether you want fewer hospital visits (immunotherapy) or prefer the quicker impact of chemotherapy.
- Cost: Immunotherapy is more expensive but might offer better outcomes for certain cancers. Financial assistance can help.
Questions to Ask Your Oncologist
- What are the side effects of immunotherapy vs chemotherapy for my type of cancer?
- How long will the treatment last, and what are the expected outcomes?
- Is biomarker testing necessary for immunotherapy?
- How will the treatment impact my daily life?
- What are the costs, and is financial assistance available?
FAQ
Can Immunotherapy and Chemotherapy Be Combined?
Yes, immunotherapy and chemotherapy can be combined in certain cases. This combination is used to enhance the effectiveness of treatment, with chemotherapy reducing the tumor burden and immunotherapy boosting the immune system’s ability to attack remaining cancer cells. Clinical trials have shown that this combination can be particularly effective in cancers like non-small cell lung cancer (NSCLC) and triple-negative breast cancer (TNBC).
What Are the Latest Advancements in Immunotherapy?
Recent advancements in immunotherapy include the development of novel immune checkpoint inhibitors, CAR T-cell therapies, and personalized cancer vaccines. Research is also exploring combination therapies that integrate immunotherapy with targeted treatments or chemotherapy to improve outcomes across various cancer types.
What Types of Cancer Are Best Treated with Immunotherapy?
Immunotherapy is particularly effective in treating cancers like melanoma, non-small cell lung cancer (NSCLC), bladder cancer, and certain types of lymphoma. It’s often used in cases where traditional treatments like chemotherapy are less effective, especially in cancers with high PD-L1 expression.
How Does Immunotherapy Work Differently from Chemotherapy?
Immunotherapy works by enhancing the body’s immune system to recognize and attack cancer cells, while chemotherapy directly targets and kills rapidly dividing cells, including both cancerous and healthy cells. This fundamental difference leads to varying side effects and effectiveness depending on the type of cancer.
What Are the Common Side Effects of Immunotherapy Compared to Chemotherapy?
Common side effects of immunotherapy include fatigue, skin reactions, and autoimmune responses like colitis or pneumonitis. Chemotherapy side effects are typically more widespread, including nausea, hair loss, immune suppression, and fatigue, due to its non-selective nature in targeting rapidly dividing cells.
Is Immunotherapy Suitable for All Cancer Patients?
No, immunotherapy is not suitable for all cancer patients. It is most effective in cancers that express certain biomarkers, like PD-L1. Patients with autoimmune diseases or certain health conditions may not be ideal candidates for immunotherapy due to the risk of exacerbating their conditions.
How Long Does It Take to See Results with Immunotherapy vs Chemotherapy?
The timeline for seeing results with immunotherapy can vary but is often longer compared to chemotherapy. While chemotherapy might show quicker results in reducing tumor size, immunotherapy works over time to build an immune response, with some patients experiencing delayed but long-lasting responses.
What Is the Role of Biomarker Testing in Choosing Between Immunotherapy and Chemotherapy?
Biomarker testing plays a crucial role in determining the suitability of immunotherapy. For instance, testing for PD-L1 expression or microsatellite instability (MSI) helps identify patients who are more likely to respond to immunotherapy, whereas chemotherapy decisions are generally less dependent on specific biomarkers.
How Does Cost Compare Between Immunotherapy and Chemotherapy?
Immunotherapy is generally more expensive than chemotherapy, with annual costs often exceeding $100,000 to $200,000, while chemotherapy typically ranges from $10,000 to $50,000 for a full course. Financial assistance programs are available for both treatments, but the out-of-pocket costs can vary significantly based on insurance coverage.
Can Patients Switch from Chemotherapy to Immunotherapy During Treatment?
Yes, patients can switch from chemotherapy to immunotherapy during treatment, especially if chemotherapy is not effective or if the cancer progresses. This decision is usually based on the cancer’s response to treatment, the patient’s overall health, and the presence of specific biomarkers that suggest a better response to immunotherapy.
Can Immunotherapy Cause Hair Loss?
No, immunotherapy typically does not cause hair loss. Unlike chemotherapy, which targets rapidly dividing cells and often results in hair loss, immunotherapy works by stimulating the immune system to fight cancer cells specifically. Therefore, hair follicles, which are also rapidly dividing cells, are usually not affected by immunotherapy.
Written by Toma Oganezova, MD