Michelle Kirschner, Clinical Lead and Medical Advisory Board Chairman at OneVillage, shared a post on LinkedIn:
“I’m grateful for the incredible opportunities to learn from leaders in cancer rehabilitation. Tonight, I had the privilege of spending time with Dr. Michael Stubblefield, Medical Director of Cancer Rehabilitation at Kessler Institute for Rehabilitation and National Medical Director for Select Medical’s ReVital Cancer Rehabilitation Program.
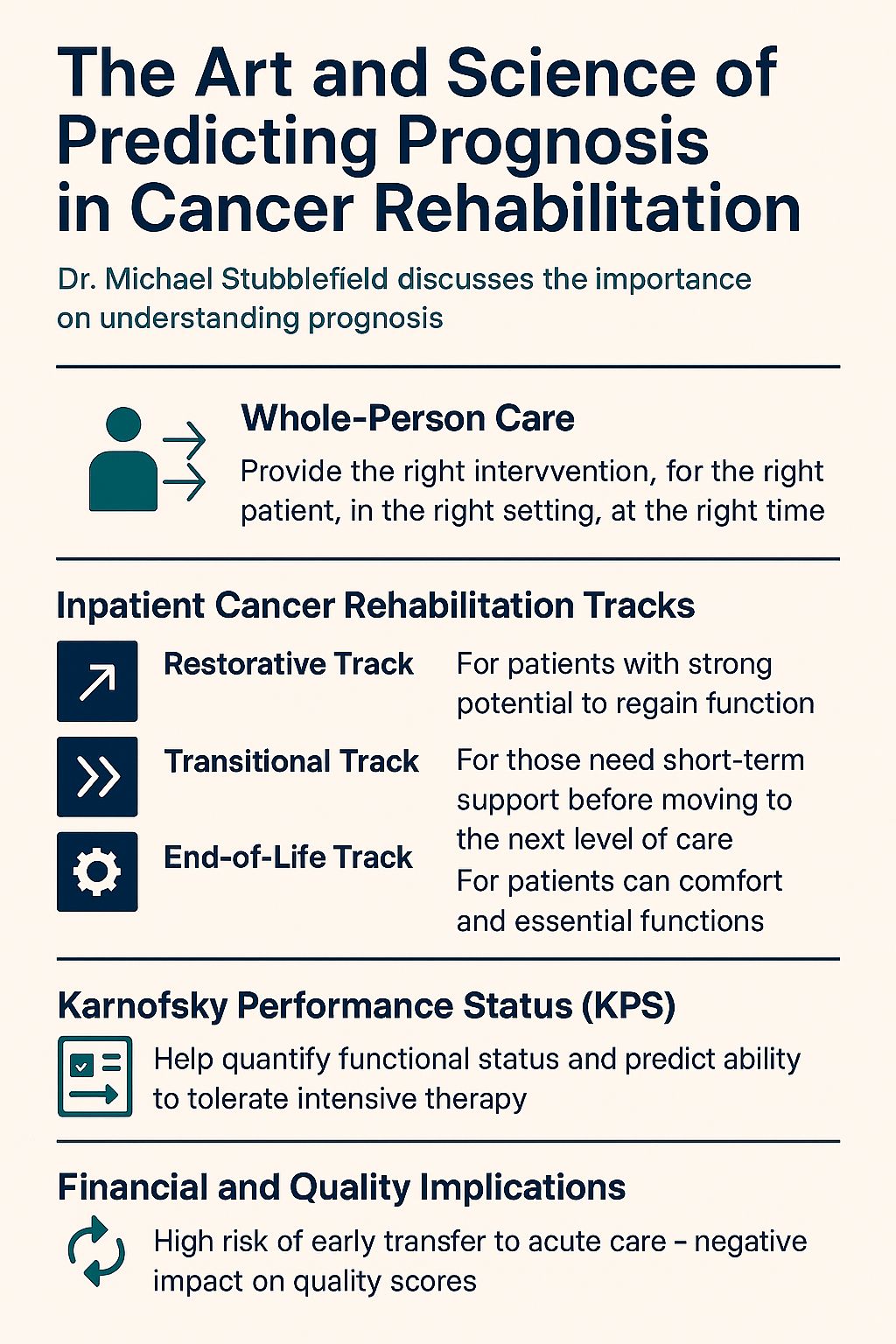
Our discussion centered on one of the most critical—and often overlooked—elements of cancer care: the art and science of predicting prognosis in cancer rehabilitation. Why does this matter so much? Because whole-person care means delivering the right intervention, for the right patient, in the right setting, at the right time.
Too often, patients who are no longer receiving active cancer treatment are transferred to inpatient rehabilitation when hospice would better serve their needs. This can create tremendous stress for patients who are physically unable to meet the 3-hour therapy requirement for inpatient rehab—and distress for therapists who feel pressured to push unrealistic goals.
Dr. Stubblefield emphasized the importance of understanding the three tracks of inpatient cancer rehab:
- Restorative Track – For patients with strong potential to regain function.
- Transitional Track – For those who need short-term support before moving to the next level of care.
- End-of-Life Track – For patients whose goals should focus on comfort and essential functions, like safe transfers, to allow them to return home for hospice care if possible.
Tools like the Karnofsky Performance Status (KPS) are invaluable in this process. KPS helps quantify a patient’s functional status and predict their ability to tolerate intensive therapy.
Why is this so important? Beyond patient well-being, there are significant financial and quality implications. Sending end-of-life patients to inpatient rehab often results in early transfers back to acute care—over 50% in some cases—which negatively impacts quality scores and adds unnecessary cost.
Predicting prognosis isn’t easy—oncologists themselves are often off by a factor of 3 to 5—but improving this process is essential for better outcomes, reduced stress for patients and clinicians, and more sustainable healthcare.
Cancer rehabilitation is about hope and function—but it must also be about honesty and appropriateness. The conversation tonight reinforced that accurate prognosis is the foundation for compassionate, effective care.
Join the CSPN to access session recordings and resources provided by Dr. Stubblefield.”
More posts featuring Michelle Kirschner.


