Othman Al-Sawaf, Haematologist and Medical Oncologist at the University Hospital Cologne, Cologne, Germany, shared a post on X:
“Check out our latest paper in Journal of Clinical Oncology on surrogacy of endpoints in 1L CLL trials!
Led by Florian Simon we systematically studied the association of PFS and MRD with OS. Some findings in a brief thread:
Using OS, the most important endpoint, as a primary endpoint in CLL is challenging due to competing risks, long followups, and effective salvage tx that are difficult to account for in 1L CLL studies.
PFS is often used as a surrogate, but its correlation with OS remains unclear.
MRD has become a key 2nd endpoint in CLL, yet so far only the prognostic effect of MRD has been validated, while the surrogacy remains to be fully explored.
A recent paper by Talal Hilal and the colleagues started to shed light on this important question:
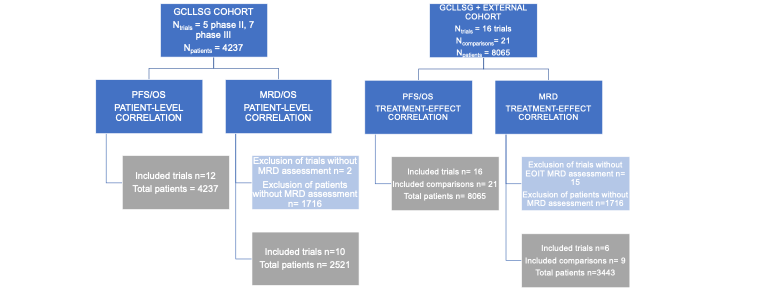
To study the surrogacy of PFS and MRD in CLL, we analyzed data from 12 GCLLSG trials and 9 additional phase III trials, covering over 8,000 patients.
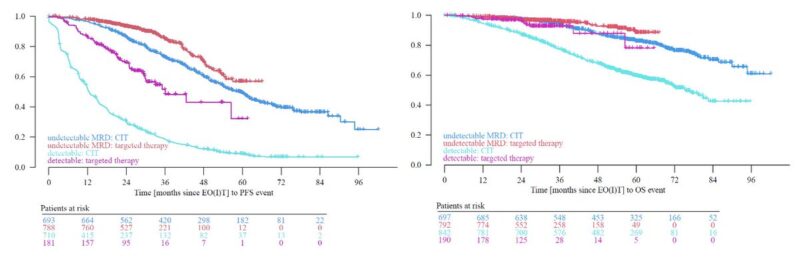
At an individual level, a strong correlation was found between PFS and OS, especially in patients treated with targeted therapies (TT), where in a Joint-Frailty model a tau of 0.91 (!) was observed.
MRD status was also a strong predictor of PFS, as shown previously.
However, to prove surrogacy, a trial-level correlation is required, i.e. the effect size of the alleged surrogate has to correlate strongly with the effect size of the true clinical outcome (e.g. PFS-HR <-> OS-HR).
There is no general consensus as to what degree of correlation is needed to assume surrogacy, but the IQWiG has previously published some recommendations (that are arguably very [too?] stringent):
At the trial level, the correlation between PFS and OS was moderate (R = 0.75, R2 = 0.56), suggesting that while PFS is useful, it may not fully capture OS outcomes.
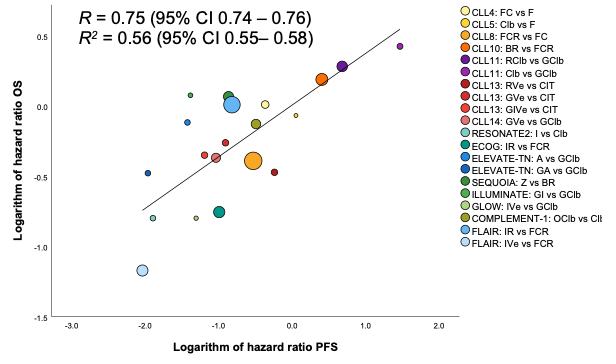
MRD showed a strong correlation with PFS (R = 0.88, R2=0.78) and a moderate link to OS (R = 0.71, R2= 0.5), however, the number of datapoints was limited as only randomized CLL studies with sufficient MRD data could be considered.
More details and multiple additional analyses in the full open-access paper here.
In summary, there is a strong individual-level correlation between PFS and OS as well as MRD and OS.
On a trial-level, the validity of surrogacy of MRD/PFS and OS appears unclear at this stage, however, with more datapoints and longer follow-up, more insights will be generated.
This work was spearheaded by Florian Simon Rudy Ligtvoet and Sandra Robrecht. We are grateful to pts & caregivers for trusting our work.
Thank you to all GCLLSG investigators and collaborators, Michael Hallek, and the Journal of Clinical Oncology editorial team.
We acknowledge support by DFG public.”
Source: Othman Al-Sawaf/X


