Rectal cancer originates in the final 12–15 cm of the large intestine, an area anatomically distinct from the colon and requiring specialized treatment approaches. Approximately 700,000 new cases of colorectal cancer are diagnosed annually worldwide, and rectal cancer accounts for a significant portion of these cases (Sung et al., 2021). Because of its location in the pelvis, rectal cancer often requires a combination of surgery, radiation therapy, and chemotherapy to achieve optimal outcomes.
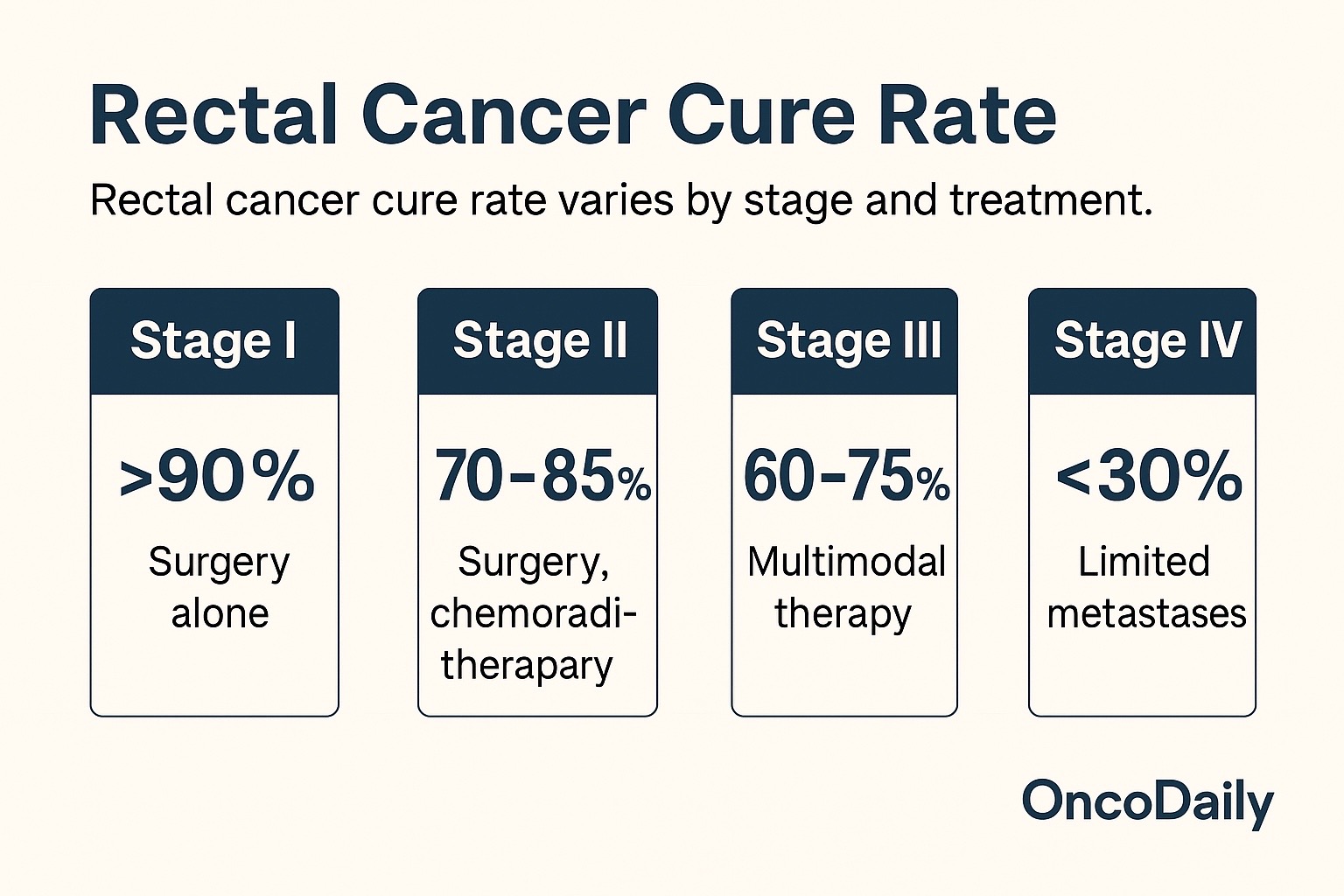
The rectal cancer cure rate varies widely depending on stage at diagnosis, tumor biology, and treatment strategy. Early-stage disease is often curable, while advanced tumors involving nearby organs, lymph nodes, or distant sites present greater challenges.

Read About Rectal Cancer on OncoDaily
What Does Cure Mean in Rectal Cancer?
In oncology, a “cure” refers to complete elimination of cancer with no recurrence over a prolonged period—typically five years or more. For rectal cancer, cure is most achievable when the tumor is localized and treated aggressively with modern multimodal therapy. Because rectal cancer can spread early to lymph nodes or recur locally, achieving cure requires precise coordination between surgical, radiation, and medical oncology teams.
As treatments evolve, including total neoadjuvant therapy and organ-preserving approaches, the rectal cancer cure rate continues to improve across all stages.
Rectal Cancer Cure Rate by Stage
Stage is the strongest determinant of the rectal cancer cure rate.
For Stage I rectal cancer, where the tumor is confined to the rectal wall, cure rates exceed 90% following surgery alone (Benson et al., 2023).
In Stage II disease, where the tumor invades deeper layers but has not reached lymph nodes, cure rates range between 70% and 85%, especially when treated with neoadjuvant chemoradiotherapy followed by curative surgery.
For Stage III rectal cancer, which involves regional lymph nodes, cure remains achievable in more than 60–75% of patients when multimodal therapy is applied. Total neoadjuvant therapy—treating before surgery with both chemotherapy and radiation—has raised survival rates and reduced recurrence risk.
In Stage IV rectal cancer, cure is rare but possible in select patients with limited metastases, especially when liver or lung lesions can be surgically removed. In these cases, long-term survival may exceed 30%, and functional cure has been documented (Van Cutsem et al., 2023).
These variations highlight why early detection and timely treatment are essential for improving the rectal cancer cure rate.
How Surgery Influences Cure
Surgery is central to curative treatment. Modern techniques, including total mesorectal excision (TME), have dramatically reduced local recurrence and improved cure rates. With proper surgical margins and removal of involved lymph nodes, patients with early and intermediate stage disease achieve long-term remission at high rates.
The rectal cancer cure rate is closely linked to the quality of surgery. Specialized colorectal surgeons and high-volume cancer centers consistently achieve better outcomes, including lower rates of tumor recurrence and postoperative complications.
The Role of Radiation and Chemotherapy
Unlike colon cancer, rectal cancer benefits significantly from radiation therapy. Neoadjuvant chemoradiation, administered before surgery, shrinks tumors, increases resectability, and reduces local recurrence risk. This strategy has become standard for Stage II–III disease and has contributed to rising rectal cancer cure rate statistics over the past two decades.
Total neoadjuvant therapy (TNT)—delivering both chemotherapy and radiation before surgery—has shown even greater promise. Clinical trials such as RAPIDO and PRODIGE-23 demonstrated improved disease-free survival and higher pathologic complete response rates, meaning no cancer remains at surgery (Bahadoer et al., 2021). Pathologic complete response is strongly associated with a significantly higher chance of cure.
Read About Radiotherapy for Rectal Cancer on OncoDaily
Can Rectal Cancer Be Cured Without Surgery?
In selected patients, especially those achieving a complete response after chemoradiotherapy, a non-operative strategy known as “watch-and-wait” may be considered. This approach avoids surgery and preserves rectal function while maintaining excellent cancer control.
Early data show that patients with sustained complete response can achieve cure rates comparable to those who undergo surgery, offering a new pathway to improve the rectal cancer cure rate while preserving quality of life (Habr-Gama et al., 2022).
Cure Rate in Advanced and Metastatic Rectal Cancer
When rectal cancer spreads to distant organs, cure becomes far less common, but it is not impossible. The introduction of combination chemotherapy, targeted therapy, and molecular profiling has transformed outcomes.
Patients with resectable liver or lung metastases who undergo curative metastasectomy can achieve five-year survival rates of 20–40%, particularly when chemotherapy produces a strong response. In the era of precision oncology, molecular subtypes such as MSI-H tumors respond well to immunotherapy, further improving the rectal cancer cure rate in select populations.
Factors Influencing Cure Rate
The rectal cancer cure rate depends on multiple factors: tumor stage, response to neoadjuvant therapy, quality of surgery, lymph node involvement, and genetic mutations such as KRAS, BRAF, or MMR status. Lifestyle factors, including smoking, obesity, diet, and exercise, also influence survival and recurrence risk.
Access to high-quality, multidisciplinary care remains one of the strongest predictors of long-term cure.
Early Detection and Screening
Screening colonoscopy remains the most effective tool for identifying rectal cancer early. Removing precancerous polyps or detecting tumors before they invade deeply significantly improves the rectal cancer cure rate. Awareness of symptoms such as rectal bleeding, changes in bowel habits, or unexplained weight loss also supports earlier diagnosis.
Living Beyond Rectal Cancer
Patients who achieve remission after treatment may live long, healthy lives. Regular follow-up—including colonoscopy, imaging, and physical examinations—is essential to detect recurrence early. Survivorship care also addresses long-term effects of treatment, such as bowel changes, fatigue, neuropathy, and emotional well-being.
For many, achieving cure is not only possible but increasingly common thanks to advancements in therapy and precision medicine.
Future Directions in Improving Cure Rates
Ongoing clinical trials continue to refine treatment sequencing, develop novel radiotherapy techniques, and evaluate immunotherapy combinations. Molecular profiling of tumors is leading to highly personalized therapy strategies, and the integration of artificial intelligence into imaging and pathology is expected to improve early detection.
As innovation accelerates, the global rectal cancer cure rate is likely to improve steadily in the coming years.
Conclusion
The rectal cancer cure rate depends heavily on stage, treatment strategy, and tumor biology, but modern care has dramatically improved long-term outcomes. Early-stage disease is often curable, and even advanced cases can achieve long-term survival with multimodal therapy.
Advances in surgery, radiation, immunotherapy, and targeted treatment continue to raise the prospect of cure for more patients worldwide.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD


