Radiotherapy for rectal cancer is a key treatment option that uses high-energy radiation to target and shrink tumors. It can be administered externally or internally, with different techniques depending on the tumor’s size and location. Radiotherapy can be used before surgery to shrink the tumor, after surgery to prevent recurrence, or palliatively to control symptoms in advanced cases. While effective, it comes with potential side effects like bowel issues, bladder problems, and fatigue, which may vary in severity. Success rates depend on factors like cancer stage and treatment combination, such as chemoradiation.
Types of Radiotherapy for Rectal Cancer
There are two main types of radiotherapy used for rectal cancer: external and internal radiotherapy. External radiotherapy involves targeting the tumor from outside the body using a machine, and it typically lasts only a few minutes per session. A CT scan is usually done before the treatment to plan the radiation precisely.
Internal radiotherapy, also known as brachytherapy or contact radiotherapy, involves placing radioactive sources near or inside the tumor. This method delivers a high dose of radiation directly to the cancer, minimizing damage to surrounding healthy tissues. It is especially effective for small, early-stage cancers and may be available in select cancer centers.
For certain cases, the Papillon technique, a type of contact radiotherapy, can be used. This technique is suitable for patients who are not fit for anesthesia or have small tumors. It is only available at a few specialized centers.
How Effective is Radiotherapy for Rectal Cancer?
Radiotherapy for rectal cancer can be highly effective, particularly when used as part of a treatment plan that includes surgery or chemotherapy. It is often used before surgery (neo-adjuvant radiotherapy) to shrink tumors, making them easier to remove and lowering the risk of cancer recurrence. This approach is effective in reducing tumor size and improving the chances of successful surgical removal.
When given after surgery (adjuvant radiotherapy), radiotherapy helps to eliminate any remaining cancer cells and further reduces the risk of the cancer returning. In both cases, its effectiveness is enhanced when combined with chemotherapy (chemoradiation), which not only shrinks the tumor but also lowers the likelihood of the cancer returning at the same site.
For advanced cases or when surgery isn’t an option, palliative radiotherapy can be effective in controlling symptoms, improving quality of life, and helping manage tumor-related issues like pain or obstruction. The success rate varies depending on factors such as the stage of the cancer, the location of the tumor, and the patient’s overall health.
Camma et al. (2000) in JAMA found that preoperative radiotherapy plus surgery for rectal cancer significantly reduced 5-year overall mortality (OR 0.84, p = .03), cancer-related mortality (OR 0.71, p<.001), and local recurrence (OR 0.49, p<.001) compared to surgery alone, without affecting distant metastases.
The Procedure and Preparation Steps for Radiotherapy in Bladder Cancer Treatment
Radiotherapy for rectal cancer involves careful planning and preparation to ensure effective treatment. A CT scan is often performed prior to the treatment to help identify the precise area that requires radiation. This scan assists in planning the optimal radiation doses and delivery. To ensure accuracy during the treatment, patients may be asked to follow specific instructions, such as preparing their bowel or bladder beforehand. Marks or small tattoos may be made on the skin to help position the patient correctly for each session.
The radiotherapy is typically delivered externally, using a machine to direct radiation toward the rectal area. The sessions are generally quick, lasting only a few minutes. In some cases, radiotherapy may be combined with chemotherapy to improve its effectiveness, especially for advanced cancer or to shrink the tumor before surgery. It’s crucial for patients to follow the preparation instructions and communicate with their medical team to ensure the treatment is as effective as possible.
Know Your Doctor, Read Special Article by OncoDaily on Who is a Radiation Oncologist?
What are the Side Effects of Radiotherapy for Rectal Cancer?
Radiotherapy for bladder cancer is an effective treatment option, but like any medical intervention, it can come with side effects. These can range from short-term issues, such as fatigue and bladder irritation, to long-term effects that may develop after treatment. Understanding these potential side effects helps patients manage their symptoms and plan for the future care they may need.
Bosset et al. (2004) in the European Journal of Cancer compared preoperative chemoradiation (5-FU + LV + XRT) vs. radiotherapy alone in T3-T4 M0 rectal cancer patients (EORTC 22921 trial). Acute diarrhea (Grade 2+) was higher in the chemoradiation group (34.3% vs. 17.3%, P<0.005), while other toxicities were similar. Compliance with radiotherapy was 98.5% (XRT) and 95.5% (XRT-CT). Early postoperative mortality was 1% in both groups.
Early Effects of Radiotherapy for Rectal Cancer
During the early stages of radiotherapy for rectal cancer, patients may experience fatigue and skin soreness in the treated area. Additionally, bowel issues such as diarrhea, cramps, and an increased urgency to use the bathroom are common. These symptoms typically improve within a few months after completing the treatment, though they may be bothersome during the course of therapy.
Conroy et al. (2021) in The Lancet Oncology reported that in locally advanced rectal cancer, neoadjuvant chemotherapy caused neutropenia (17%) and diarrhoea (11%). During chemoradiotherapy, lymphopenia occurred in 28% (neoadjuvant group) vs. 30% (standard group). Serious adverse events during adjuvant therapy were lower in the neoadjuvant group (11% vs. 23%, p=0.0049).
Late Effects of Radiotherapy for Rectal Cancer
Some patients may experience long-term changes in bowel function after radiotherapy, which can include persistent diarrhea or difficulty controlling bowel movements. There can also be discomfort in the pelvic area, with potential bone damage that leads to fractures. Additionally, sexual health may be affected, and in some cases, the bladder can become irritated. These late effects may require ongoing management and should be discussed with a healthcare provider to explore possible treatments.
Bruheim et al. (2010) in International Journal of Radiation Oncology Biology Physics found that rectal cancer radiotherapy increased bowel frequency (>8 times/day: 19% vs. 6%, p<0.001) and fecal incontinence (49% vs. 15%, p<0.001). Daily urinary incontinence was higher in RT+ patients (9% vs. 2%, p=0.001). Radiotherapy negatively affected social function and quality of life.
What Should Patients Expect During Radiation Treatment?
During radiation treatment for rectal cancer, patients can expect a carefully planned process to ensure the radiation is targeted precisely at the tumor. Before starting treatment, a CT scan is often used to map out the exact location for radiation delivery. This helps the healthcare team determine the best approach for each individual case. During the treatment itself, patients are positioned on a treatment table, and the area being treated is marked to maintain accuracy. The actual radiation session is typically brief, lasting only a few minutes, and patients will be asked to remain still to help ensure precise targeting.
While the treatment is non-invasive, patients may experience some discomfort from having to remain in a specific position. The treatment does not cause pain, but the healthcare team will monitor the patient’s comfort and make adjustments if necessary. Communication with the medical team is essential, and patients should feel comfortable asking questions or expressing any concerns. After the treatment, patients can usually resume their normal activities, although they may be advised to follow specific care instructions to manage side effects.
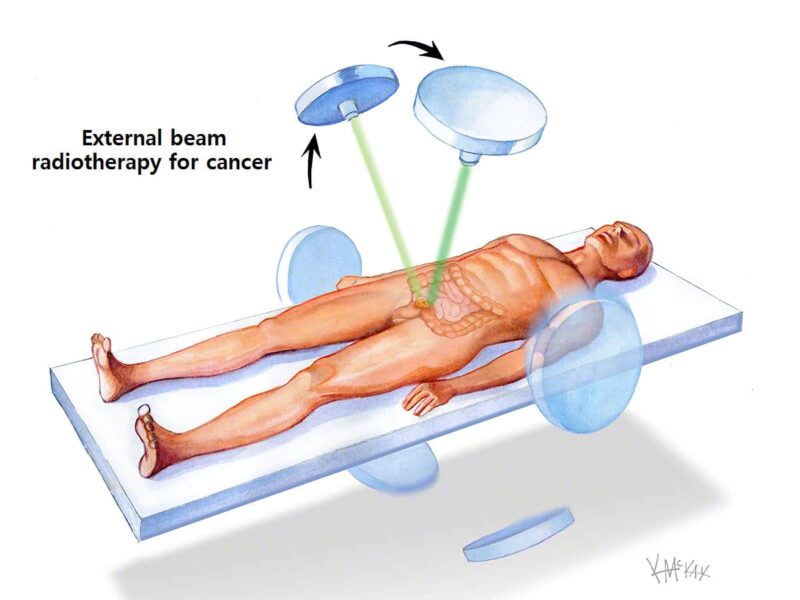
source: www.colorectalsurgeonssydney.com
How Long Does It Take to See Results?
The time it takes to see results from radiotherapy for rectal cancer varies depending on individual factors such as the type of treatment and the tumor’s response. If radiotherapy is given before surgery, it may shrink the tumor, making it easier to remove and reducing the risk of the cancer returning. This effect can take several weeks to become noticeable. When radiotherapy is administered after surgery, its goal is to eliminate any remaining cancer cells and lower the chance of recurrence. In this case, the results might take a few weeks to be evident.
For patients undergoing palliative radiotherapy, the effects are often seen in terms of symptom relief rather than tumor shrinkage. This form of treatment aims to reduce discomfort and improve quality of life, with improvements typically observed within a few weeks after treatment. Each patient’s experience will be different, so it’s important to maintain regular communication with the healthcare team to assess progress and manage any side effects.
What Are the Costs of Radiotherapy for Rectal Cancer?
The costs of radiotherapy for rectal cancer can vary significantly based on several factors, including the type of radiotherapy used, the duration of the treatment, and the healthcare facility providing the service. External beam radiotherapy, which is the most common form, may involve a series of treatment sessions that span over several weeks, contributing to the overall cost. Additionally, the need for advanced imaging or planning technologies, such as CT scans or specialized techniques, can add to the expense.
For patients undergoing internal radiotherapy or brachytherapy, which is less commonly available, the cost may be higher due to the specialized equipment and expertise required. The total cost also includes any associated medical consultations, follow-up care, and management of side effects. It is important for patients to discuss with their healthcare providers the specifics of their treatment plan, potential costs, and available financial assistance options, as some of these expenses may be covered by insurance or other healthcare programs.
Hanly et al. (2015) in BMC Health Services Research estimated rectal cancer radiotherapy costs at €2,080 for short-course (5 fractions) and €3,609 for long-course (25 fractions) treatments in 2012. Costs were highest in treatment planning for short-course (€1,217, 58%) and in the radiation phase for long-course (€1,974, 60%). Efficiency improvements could reduce costs by 20% (€1,660) for short-course and 35% (€2,354) for long-course.
Raldow et al. (2019) in JAMA found that short-course radiotherapy was more cost-effective than long-course chemoradiotherapy for locally advanced rectal cancer (ICER: $133,495 per QALY). However, for distal tumors, long-course chemoradiotherapy was more cost-effective (ICER: $61,123 per QALY) due to higher LAR rates (39% vs. 19%). Patient preferences for NED-LAR and NED-APR health states influenced the cost-effectiveness outcomes.
How Does Radiotherapy Compare to Other Treatments for Rectal Cancer?
Radiotherapy is a key treatment option for rectal cancer, but its effectiveness and suitability depend on the stage and location of the cancer, as well as individual patient factors. It is often used in combination with other treatments like surgery and chemotherapy. Here’s how it compares to these options:
Radiotherapy for rectal cancer vs Surgery
Radiotherapy is often used before surgery to shrink tumors, making them easier to remove, and after surgery to reduce the risk of cancer returning. However, surgery is typically the primary method for removing rectal tumors. While surgery can offer a definitive treatment, radiotherapy helps in cases where surgery alone may not be enough, such as when the cancer is inoperable or located in a difficult-to-reach area.
Radiotherapy for rectal cancer vs Chemotherapy
Radiotherapy and chemotherapy are sometimes used together (chemoradiation) to shrink tumors before surgery and reduce the chance of cancer recurring. While chemotherapy targets cancer cells throughout the body, radiotherapy focuses on localized treatment, delivering targeted radiation to the tumor. Chemotherapy tends to cause more systemic side effects, while radiotherapy is more localized, which means it may have fewer side effects in some cases. Both treatments complement each other, and the choice between them or their combination depends on the cancer’s specifics and the patient’s overall health.
How Does Radiotherapy for Rectal Cancer Affect Sexual Health and Fertility?
Radiotherapy for rectal cancer can have significant effects on both sexual health and fertility. These effects depend on the location of the radiation, the dose, and whether any other treatments are being used simultaneously.
Sexual Health and Fertility in Women
Radiotherapy for rectal cancer can significantly affect sexual health and fertility in women. The pelvic radiation can lead to vaginal dryness, reduced lubrication, or discomfort during intercourse, which can impact sexual desire and function. In addition to these changes, the radiation may cause the ovaries to stop functioning properly, resulting in premature menopause and potential infertility. Women who wish to preserve their fertility before starting radiotherapy may consider options like egg banking. It’s essential for women to discuss the possibility of these side effects with their healthcare team and explore ways to manage them.
Bruheim et al. (2010), published in Acta Oncologica, found that female rectal cancer patients treated with (chemo-)radiotherapy had more vaginal dryness (50% vs. 24%), dyspareunia (35% vs. 11%), and reduced vaginal dimension (35% vs. 6%) compared to those treated with surgery alone. Sexual interest and worries about sex life were not significantly different.
Sexual Health and Fertility in Men
For men undergoing radiotherapy for rectal cancer, sexual health can also be impacted. Radiation in the pelvic region may cause erectile dysfunction or a decrease in sexual desire. Additionally, the testes may be affected, leading to a reduction in sperm count or quality, which can reduce fertility. Some men may experience temporary issues, while for others, fertility may be permanently affected. If fertility preservation is a concern, men may consider sperm banking before treatment. Men are encouraged to discuss potential sexual and fertility issues with their doctors before starting radiotherapy, so they are well-informed about their options.
Bruheim et al. (2010), published in International Journal of Radiation Oncology Biology Physics, found that male rectal cancer patients treated with pre- or postoperative RT had significantly poorer sexual function. Among 241 patients, RT+ patients had a 7.3 times higher risk of moderate–severe erectile dysfunction than RT– patients (p < 0.001), with erectile dysfunction linked to low serum testosterone (p = 0.01).
Can All Rectal Cancer Patients Receive Radiotherapy?
Not all rectal cancer patients are suitable candidates for radiotherapy. The decision to use radiotherapy depends on various factors, including the stage and location of the cancer, as well as the patient’s overall health and ability to tolerate the treatment. Radiotherapy is commonly used for patients with localized rectal cancer, either before or after surgery, or in cases where surgery is not an option. However, for patients with advanced or metastatic cancer, radiotherapy might not be effective, and other treatment options may be explored. Your healthcare team will assess your individual case to determine whether radiotherapy is the best approach for your treatment plan.
What Research is Being Done on Radiotherapy for Rectal Cancer?
MRI-guided radiotherapy (MRIgRT) is an advanced technique for rectal cancer treatment, enabling precise tumor targeting, daily image verification, and adaptive treatment based on functional imaging. Research by Giuditta Chiloiro, Cihan Gani, and Luca Boldrini in 2024, published in Seminars in Radiation Oncology, highlights its potential benefits, though further clinical studies are needed to confirm its efficacy.
Felchle et al. (2024), published in International Journal of Radiation Oncology Biology Physics, developed a novel orthotopic mouse model of rectal cancer using organoid injections and small-animal radiotherapy. The model enables studying tumor heterogeneity, treatment responses, and combination therapies, offering insights into improving rectal cancer outcomes.
How Can Patients Support Their Health During Radiotherapy?
During radiotherapy, patients can take several steps to support their health and manage potential side effects. Staying hydrated is important, so drinking plenty of fluids, especially water, is recommended. Avoiding alcohol and caffeine can help reduce bladder irritation, and maintaining a balanced diet can support overall health and energy levels. Patients should also follow their healthcare team’s guidance on managing side effects, such as skin care for any radiation burns, and taking prescribed medications to manage bowel or bladder issues. Regular communication with healthcare providers is crucial to address any concerns or symptoms that arise. Additionally, keeping a positive outlook and incorporating stress-reduction techniques can contribute to better overall well-being during treatment.
What Support is Available for Patients Undergoing Radiotherapy for Rectal Cancer?
Patients undergoing radiotherapy for rectal cancer have access to various support resources. Healthcare teams provide guidance on managing side effects and addressing concerns. Emotional support is available through counseling and support groups, while nutritional advice helps maintain a healthy diet. Patients are encouraged to reach out to their healthcare team for questions about treatment, follow-up care, or symptom management, ensuring they feel informed and supported throughout their journey.
Written by Aren Karapetyan, MD
FAQ
What types of radiotherapy are used for rectal cancer?
Radiotherapy for rectal cancer includes external radiotherapy, where radiation is directed from outside the body, and internal radiotherapy (brachytherapy), which involves placing radioactive sources near the tumor.
How is radiotherapy for rectal cancer given?
Radiotherapy can be delivered externally using a machine or internally using radioactive sources placed close to the tumor. The treatment is planned based on imaging scans for accuracy.
When is radiotherapy given for rectal cancer?
Radiotherapy can be used before surgery to shrink the tumor, after surgery to reduce the risk of recurrence, or as palliative treatment to relieve symptoms in advanced cases.
What are the common side effects of radiotherapy for rectal cancer?
Common side effects include tiredness, sore skin, bowel problems like diarrhea or constipation, bladder issues, and sexual health concerns. These may improve after treatment ends.
What are the long-term side effects of radiotherapy for rectal cancer?
Long-term effects can include bowel changes, pelvic bone damage, bladder irritation, and fertility issues. Some patients may also experience ongoing sexual health problems.
How should patients prepare for radiotherapy for rectal cancer?
Patients may need a CT scan for treatment planning. They should follow instructions on bowel preparation and may be asked to wear specific clothing or avoid certain activities before treatment.
Can radiotherapy affect fertility and sexual health?
Radiotherapy can affect fertility and sexual health, particularly in the pelvic area. It may cause infertility and impact sexual function in both men and women, though support options are available.
How long does it take to see results from radiotherapy for rectal cancer?
Results from radiotherapy may take weeks to months to become apparent. Tumor shrinkage or symptom relief is often observed after the treatment course is completed.
What support is available for rectal cancer patients undergoing radiotherapy?
Support includes counseling for emotional well-being, nutritional guidance, and assistance in managing side effects. Healthcare teams are available to address any concerns and provide information.
How can patients support their health during radiotherapy for rectal cancer?
Patients should maintain a healthy diet, manage stress, and stay hydrated. Regular communication with the healthcare team and following prescribed care plans helps manage side effects and promotes recovery.


