Radiotherapy for thyroid cancer involves using radiation to target and destroy cancer cells, a process carefully planned by a specialized team to ensure precise targeting and minimal harm to healthy tissues. This treatment can be delivered in two primary ways: from inside the body, known as internal radiotherapy or radioactive iodine (RAI) therapy, and from outside the body, referred to as external radiotherapy or external beam radiation therapy (EBRT).
What is Radiotherapy for Thyroid Cancer?
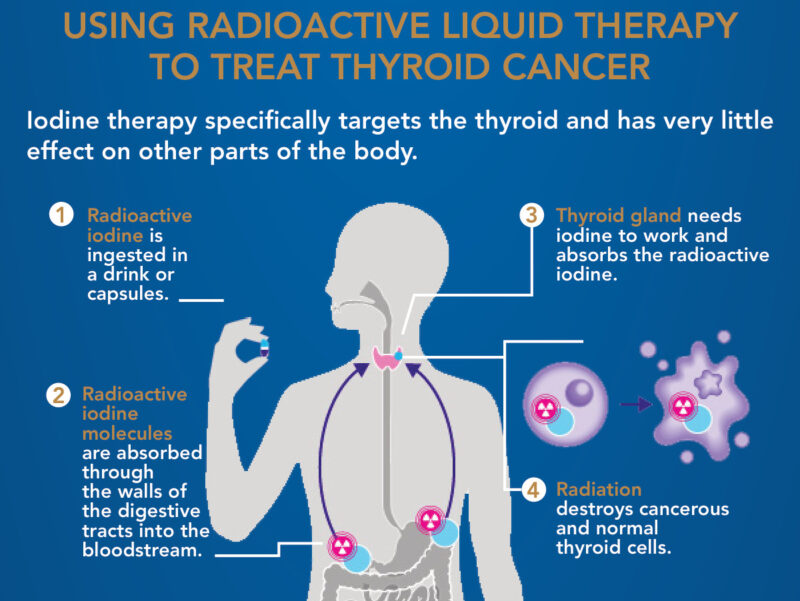
Internal radiotherapy, or radioactive iodine (RAI) therapy, involves taking radioactive iodine (I-131) as a capsule or drink. Thyroid cells, including specific cancer cells, absorb this iodine, emitting radiation to kill them. It’s primarily used for differentiated thyroid cancers (like papillary or follicular) after surgery or for spread, and requires preparation to boost TSH levels and a low-iodine diet. Patients are temporarily radioactive and must follow precautions to protect others. Side effects can include neck tenderness, salivary gland issues, and in rare cases, long-term concerns like dry eyes or slight fertility impacts.
External radiotherapy (EBRT) uses a machine to aim high-energy radiation beams at the cancer from outside the body. This method is employed for thyroid cancers that don’t absorb iodine (like medullary or anaplastic types), if other treatments fail, or for symptom control. EBRT does not make the patient radioactive. Treatment involves precise planning with scans and skin markings or a mask. Side effects, particularly when aimed at the neck, can include skin reactions, swallowing difficulties, and fatigue.
Internal Radiotherapy (Radioactive Iodine – RAI)
Radioactive iodine therapy utilizes a radioactive form of iodine, specifically iodine 131 (I-131), which is taken as a capsule or a liquid. Thyroid cells naturally absorb iodine, and this property is exploited in RAI therapy; the radioactive iodine circulates through the bloodstream and is primarily taken up by thyroid cells and any remaining thyroid cancer cells. Once absorbed, the radiation emitted by the iodine kills these cells. The high dose of radiation delivered to the thyroid cells has little effect on other cells in the body because they don’t absorb iodine similarly.
RAI is a type of radioisotope therapy and is particularly effective for differentiated thyroid cancers, such as papillary and follicular thyroid cancers, including Hurthle cell cancer, as these types are more likely to absorb iodine. It’s often used after surgery to eliminate any cancer cells that might have been left behind, to reduce the risk of the cancer returning, or to treat cancer that has spread to lymph nodes or other parts of the body. However, RAI is not used for anaplastic or medullary thyroid cancers because these types typically do not take up iodine. A test dose might be given to see if the cancer cells absorb the iodine effectively.
External Radiotherapy (EBRT)
External radiotherapy uses a specialized machine to aim high-energy radiation beams, similar to X-rays or protons, at precise points on the cancer. This method is different from internal radiotherapy as the radiation comes from outside the body, and it does not make the patient radioactive, meaning it’s safe to be around others, including pregnant women and children.
EBRT is primarily used when other treatments, like radioactive iodine, are not suitable or effective, or if the cancer has recurred. It is often recommended for medullary or anaplastic thyroid cancers because these types do not take up iodine. It can also be used if cancer has not been completely removed by surgery and RAI, if there’s a high risk of recurrence, or to control symptoms like pain caused by cancer that has spread to nearby tissues or bones, serving as a palliative treatment.
What are the Side Effects of Internal Radiotherapy (Radioactive Iodine – RAI)?
Radioactive iodine (RAI) therapy, a form of internal radiotherapy for thyroid cancer, can lead to various side effects, which vary based on the dose administered, the patient’s age, and other existing medical conditions. These side effects can be categorized into short-term and long-term effects.
Short-Term Side Effects
Immediately following radioactive iodine treatment, patients may experience several temporary side effects. These can include neck tenderness and swelling, particularly if a significant portion of the thyroid gland remained. Patients might also feel nausea and vomiting in the first few days after treatment. Inflammation of the salivary glands is common, which can cause swelling and pain, leading to dry mouth and changes in taste or smell. This dry mouth sensation often improves over time, and chewing gum or sucking on hard candy might offer some relief. Some individuals might also feel flushed or experience a feeling of tightness in their neck.
Rarely, inflammation of the stomach lining (gastritis) and bladder (cystitis) can occur, potentially causing heartburn, diarrhea, or pain and urgency when urinating. Any such symptoms should be reported to the healthcare team, as painkillers or anti-sickness medicines can often help manage them.
Long-Term Side Effects
While most side effects resolve within weeks or months, some can persist or appear later. Inflammation of the salivary glands can, for a few individuals, become a persistent issue, leading to chronic dry mouth and altered taste or smell. Tiredness is a very common long-term side effect, with many people feeling fatigued for up to a year after treatment, though energy levels typically return to normal. Radioactive iodine can also affect the lacrimal glands that produce tears, potentially leading to dry or watery eyes.
Regarding fertility, RAI treatment generally should not affect a woman’s ability to have children, though some women might experience irregular periods for up to a year after treatment. For men, repeated high doses of radioactive iodine can, in rare cases, lead to lower sperm counts or infertility, though this often improves over time, and sperm banking might be offered as a precaution. Doctors typically recommend that women wait at least 6 months and men at least 4 months before trying to conceive after treatment to minimize any potential risk to a future pregnancy.
Rarely, RAI can affect the bone marrow, causing a small and usually temporary drop in blood cell counts, which typically causes no issues unless combined with external radiotherapy to the bones. If thyroid cancer has spread to the lungs and requires repeated RAI treatments, there’s a very rare risk of developing lung problems, such as radiation fibrosis, where lung tissue becomes less stretchy and can make breathing more difficult. Finally, there is a slightly increased, but generally very low, risk of developing a second cancer in the future, such as leukemia, stomach cancer, or salivary gland cancer, after RAI therapy. Your healthcare team will discuss these risks and benefits with you.
How is RAI Administered?
Preparation for RAI treatment is crucial to enhance its effectiveness. Patients might need to stop taking thyroid hormone tablets for several weeks or receive injections of a man-made thyroid stimulating hormone (TSH) called recombinant human TSH (rhTSH) to increase their TSH levels. High TSH levels encourage thyroid cancer cells to absorb more radioactive iodine. Additionally, a low-iodine diet is often recommended for one to two weeks before treatment. This diet involves avoiding foods high in iodine, such as seafood, dairy products, eggs, and iodized salt, while allowing foods like fruits, vegetables, meat, and fresh bread.
During the treatment, the patient swallows a radioactive iodine capsule or drink and is usually asked not to eat or drink for a couple of hours afterward to aid absorption. Following this, drinking plenty of fluids is encouraged to help flush the radioactive iodine out of the system. Since the patient becomes radioactive for a few days, precautions are necessary to protect others. This often involves staying in a single, isolated hospital room until radiation levels drop to a safe limit. Hospital staff might use radiation monitors, serve meals on disposable cutlery, and ask patients to flush the toilet multiple times and shower daily.
When returning home, further precautions are advised, such as avoiding close, lengthy contact with others (especially babies, young children, pregnant women, and pets), not sharing a bed, avoiding sexual contact for a period, and practicing good hygiene by using separate towels, cutlery, and flushing the toilet twice. Women are generally advised to use reliable contraception for at least 6 months, and men for at least 4 months, after treatment. Travelers might need a certificate from the hospital to explain their treatment if they plan to travel abroad, as radioactive iodine can trigger airport radiation alarms.
source: www.thecentertx.com
External Radiotherapy (EBRT) Side Effects
External radiotherapy (EBRT) for thyroid cancer, which uses external radiation beams, can lead to various side effects, primarily affecting the area treated. These side effects can be categorized into short-term and, less commonly, long-term effects.
Short-Term Side Effects
Side effects from EBRT usually begin gradually during the course of treatment and tend to be most noticeable around 10 to 14 days after the treatment concludes, typically improving over the following 2 to 3 weeks. When radiation is aimed at the neck, common side effects include sore, red skin in the treatment area, similar to a sunburn. Patients may experience a sore mouth or throat (mucositis), leading to difficulty swallowing (dysphagia), a dry mouth, and a hoarse voice.
Some individuals might also notice swelling in their face or neck (lymphoedema). Additionally, a general feeling of tiredness (fatigue) is a common side effect. The healthcare team can provide assistance with managing these symptoms, including painkillers if the throat is very sore.
Long-Term Side Effects
While many side effects of External Beam Radiation Therapy (EBRT) for thyroid cancer are short-term and resolve within weeks to months after treatment, some can persist or appear as long-term effects.
These can include permanent dry mouth (xerostomia) and changes in taste, which can affect quality of life and increase the risk of tooth decay. Skin changes in the treated area, such as altered color or texture, scarring, and increased sensitivity to sunlight, can be long-lasting or permanent. The soft tissues and muscles of the neck may become stiff or scarred, leading to reduced flexibility and movement, or chronic swelling. In some cases, difficulty swallowing due to scarring and narrowing of the throat can be a persistent issue, potentially requiring interventions.
Hoarseness or changes in voice can also last for several months or, rarely, be permanent. There’s also a possibility of an underactive thyroid gland (hypothyroidism), which usually requires lifelong hormone replacement. While rare, more severe long-term complications can include damage to bones (fractures), nerve injury, and a slightly increased, though generally low, risk of developing a second primary cancer in the future.
How External Radiotherapy (EBRT) Administered?
Before treatment begins, a planning appointment is essential. This involves a planning CT scan to precisely identify the cancer and the surrounding areas, allowing the medical team to determine the exact radiation dose and angles for the beams. During this planning, small, permanent pin-point sized tattoo marks are made on the patient’s skin, and sometimes temporary ink marks are added, to ensure consistent positioning for every treatment session. If the treatment is for the head and neck, a custom-made plastic mask is also created. This mask helps the patient remain very still, and marks on it are used to align the radiotherapy machine accurately.
The treatment itself is typically given five days a week, from Monday to Friday, over several weeks, although the exact duration can vary. Each session is painless and lasts only a few minutes, similar to a regular X-ray, though the time spent getting the patient into the correct position on the treatment couch can take longer, up to 30 minutes. During the treatment, the patient lies very still on a table while the large radiotherapy machine moves around them without making any physical contact. Radiographers monitor the patient from a separate room using a CCTV screen and communicate via an intercom, ensuring the patient’s comfort and stillness throughout the procedure.

Read OncoDaily’s Special Article About Radiotherapy Masks
What Are the Costs of Radiotherapy for Thyroid Cancer?
A 2022 study by Uppal et al. in JAMA Otolaryngology – Head & Neck Surgery revealed that thyroid cancer carries a significant financial burden in the US, with survivors experiencing higher bankruptcy rates than those with other cancers. Initial out-of-pocket costs range from $1,425 to $17,000, influenced by age, surgery, and insurance. Risk factors for financial strain include younger age, no insurance, and incomes below $49,000. Bankruptcy rates one year after diagnosis were highest for thyroid cancer at 9.3 per 1000 person-years. The authors call for improved research methods and data sources to better understand and alleviate this financial burden.
A 2023 study by Li et al., published in Value in Health, investigated the economic burden of thyroid cancer management in France, a country significantly impacted by overdiagnosis. The research aimed to quantify these costs and determine the proportion attributable to overtreatment of overdiagnosed cases.
Between 2011 and 2015, an estimated 33,911 women and 10,846 men in France were diagnosed with thyroid cancer, with an average cost per person of €6,248. The study found that between 8,114 and 14,925 women and 1,465 and 3,626 men among those treated were cases of overdiagnosis.
The total cost of thyroid cancer management in France was an estimated €203.5 million. A substantial portion of this, between €59.9 million (29.4% of total cost) and €115.9 million (56.9% of total cost), was attributed to the treatment of overdiagnosed cases. The authors concluded that thyroid cancer management poses a significant economic burden in France, largely driven by overdiagnosis and subsequent treatments.
What Are The Recent Advancements in Radiotherapy for Thyroid Cancer?
A 2024 study by Tan et al. in the European Thyroid Journal investigated a promising combination therapy for aggressive anaplastic thyroid cancer (ATC), which typically has poor outcomes. In a case series of five ATC patients, a regimen combining hypofractionated radiotherapy (QUAD-shot) with pembrolizumab immunotherapy showed an 80% best overall response rate (two complete responses and two partial responses) at a median follow-up of 32.6 months. The median progression-free survival was 7.6 months, with a 40% one-year PFS and overall survival rate. This well-tolerated treatment, possibly synergizing local and systemic anti-tumor effects, suggests a new avenue for investigation in larger cohorts.
A 2024 study by Chen et al. in the International Journal of Hyperthermia evaluated the effectiveness of combining radiofrequency ablation (RFA) with external beam radiation therapy (EBRT) for inoperable, recurrent differentiated thyroid cancer (rDTC) with critical organ invasion. This retrospective study included 11 patients with 14 rDTC lesions treated between April 2020 and January 2022.
With a median follow-up of 33.7 months, the results showed high efficacy and safety: all patients maintained locoregional control, and the 2-year survival rate was 90.9%. The combined treatment achieved a substantial volume reduction ratio of 92.1% ± 5.1%. The mean nadir thyroglobulin level for patients without initial distant metastases was 1.40 ± 0.81 ng/ml. Regarding complications, one patient (9%) experienced temporary hoarseness after RFA, while grade 2 radiation dermatitis occurred in 3 patients (27.2%) and grade 2 dysphagia in 4 patients (36.4%). No severe (grade 3 or greater) toxicities were observed. The authors concluded that salvage RFA followed by EBRT is a feasible, effective, and safe treatment option for these challenging rDTC cases.
How Can Patients Support Their Health During Radiotherapy?
During both radioactive iodine (RAI) and external beam radiation therapy (EBRT), the healthcare team plays a crucial role in explaining treatments, benefits, side effects, and helping patients manage them. Patients should maintain open communication with their specialists and nurses, reporting any symptoms or side effects without delay.
For Radioactive Iodine (RAI) treatment, patient support focuses heavily on managing the immediate effects and safety precautions. This includes rigorously following the low-iodine diet before treatment and, after receiving the radioactive iodine, drinking plenty of fluids (at least eight 8-ounce cups daily) for several days to help flush the radioactive material from the body through urine. Patients are also encouraged to urinate frequently, sitting down to avoid spills, and to ensure regular bowel movements, possibly using laxatives if constipated, as radioactive material also leaves the body through feces.
To alleviate dry mouth and salivary gland issues, sucking on sour hard candies or chewing gum can be beneficial. Strict adherence to radiation safety precautions at home, such as maintaining distance from others (especially children and pregnant women), not sharing beds, using separate hygiene items, and avoiding food preparation for others, is vital.
For External Radiotherapy (EBRT), supporting health involves managing localized side effects and maintaining overall well-being. Patients should inform their radiographers if they are uncomfortable during planning or treatment sessions, as adjustments can be made. Regarding skin care in the treated area, it’s important not to apply any lotions, powders, or creams without checking with nurses, radiographers, or doctors, and to avoid shaving to prevent irritation. For throat and mouth issues like soreness, dry mouth, or difficulty swallowing, the medical team can offer advice, including painkillers if necessary. General side effects like tiredness are common for both therapies, suggesting that adequate rest and energy management are important.
In general, patients should ensure they understand all instructions before leaving the hospital, maintain regular follow-up appointments, and discuss any concerns, including potential long-term effects like fertility issues or the very low risk of second cancers, with their healthcare team. While not explicitly detailed, general healthy practices such as a balanced diet and adequate rest can also support overall well-being during treatment.
Written By Aren Karapetyan, MD
FAQ
What are the two main types of radiotherapy for thyroid cancer?
The two main types are internal radiotherapy (radioactive iodine or RAI) and external radiotherapy (external beam radiation therapy or EBRT).
How does Radioactive Iodine (RAI) therapy work?
RAI therapy involves taking radioactive iodine (I-131) which is absorbed by thyroid cells and certain cancer cells, delivering radiation that kills them.
When is RAI therapy typically used?
RAI therapy is commonly used for differentiated thyroid cancers (like papillary or follicular) after surgery, or if the cancer has spread, as these types absorb iodine.
Why isn't RAI therapy used for all types of thyroid cancer?
RAI therapy is not used for anaplastic or medullary thyroid cancers because these types do not absorb iodine.
What preparation is needed before RAI therapy?
Preparation often includes increasing TSH levels (by stopping thyroid hormones or TSH injections) and following a low-iodine diet for one to two weeks
Will I be radioactive after external beam radiation therapy (EBRT)?
No, EBRT does not make the patient radioactive; it is safe to be around others, including pregnant women and children.
When is EBRT typically used for thyroid cancer?
EBRT is used for thyroid cancers that don't absorb iodine (like medullary or anaplastic), if other treatments are ineffective, or for symptom control when cancer has spread.
What are common short-term side effects of EBRT to the neck?
Common short-term side effects include sore, red skin, a sore mouth or throat, difficulty swallowing, dry mouth, hoarseness, and fatigue.
How can patients manage dry mouth during radiotherapy?
For RAI, sucking on sour hard candies or chewing gum can help. For EBRT, consult the healthcare team before using any lotions or creams.