At the Society for Integrative Oncology (SIO) 2025 Annual Meeting, one of the most talked-about plenary sessions explored psychedelics and cancer care, bringing together leading experts from Yale, Harvard, and international research institutions. Moderated by Dr. Miriam A. Lberg of Yale Cancer Center and Dr. Linda Carlson, the session examined how psychedelic-assisted therapy could transform the management of psychological, spiritual, and physical suffering in cancer patients.
Background
Cancer, as described by Dr. Anna Yusum of Yale University, is “an existential earthquake.” Beyond pain and physical symptoms, patients often experience anxiety, demoralization, and a loss of meaning. Psychedelics, she explained, offer a unique dual-action pathway—acting biologically on serotonin signaling and inflammation, while simultaneously addressing existential and spiritual distress.
Early studies from Johns Hopkins University and NYU have shown that a single psilocybin-assisted session can lead to rapid and sustained reductions in anxiety and depression among patients with life-threatening cancers. In some cohorts, over 60% achieved full remission of depressive symptoms, with effects lasting six months or longer. Patients frequently described their psychedelic experiences as among the most meaningful of their lives, often reporting new feelings of peace, forgiveness, and connection.
The Clinical Evidence and Evolving Guidelines
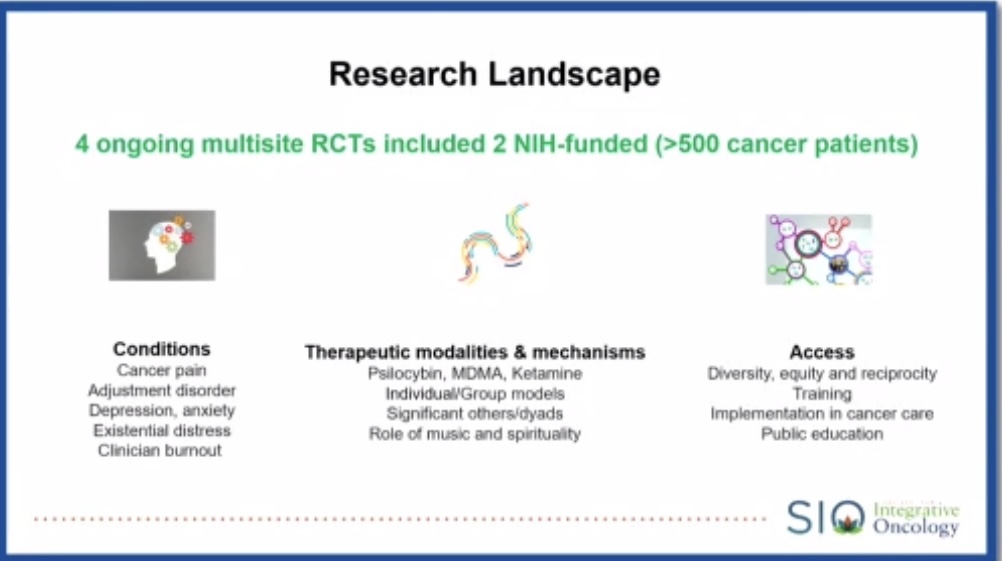
Dr. Yvan Beaussant from Dana-Farber Cancer Institute and Harvard Medical School presented a comprehensive review of clinical trials, noting that between 2011 and 2024, more than 10 modern studies have evaluated psilocybin, MDMA, and related compounds for depression, anxiety, and existential distress in cancer patients.
Most trials demonstrate both safety and feasibility, including those in patients undergoing active chemotherapy. The emerging data have been strong enough that 2023 JAMA Psychiatry guidelines formally mentioned psychedelics as a potential adjunct in treating cancer-related depression and demoralization, marking a historic milestone for integrative oncology.
Dr. Beaussant highlighted the first group-based psilocybin study in cancer patients with major depressive disorder. Eighty percent of participants showed significant improvement, and over half reached remission within eight weeks. Group settings were found to enhance safety, connection, and emotional openness, suggesting a feasible model for clinical integration.
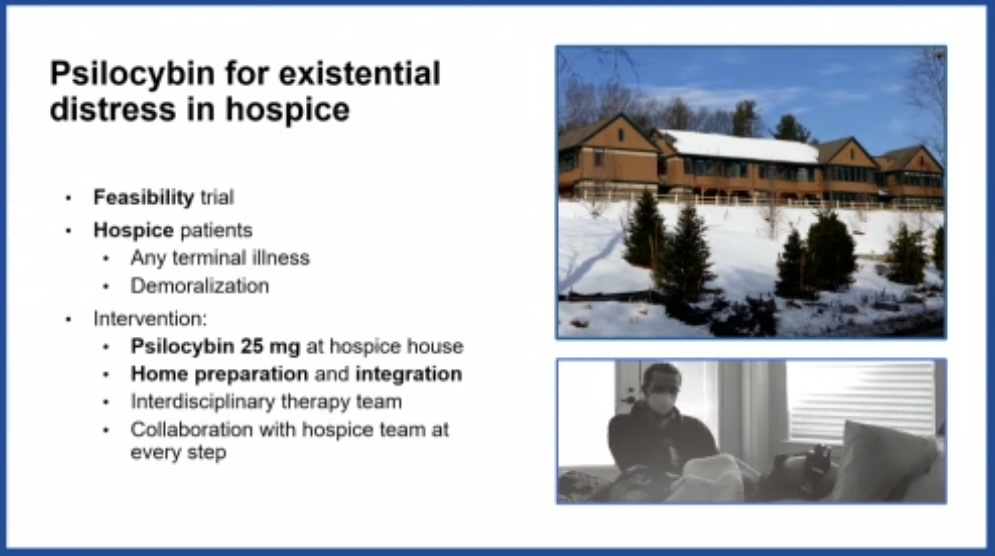
Another feasibility trial at Dana-Farber tested psilocybin in patients with terminal cancer and demoralization syndrome, supported by a multidisciplinary team of palliative physicians, chaplains, and music therapists. Despite severe symptom burden, participants achieved a 50% reduction in demoralization within three weeks, and both patients and families described profound emotional healing.
Mechanisms and the Therapeutic Alliance
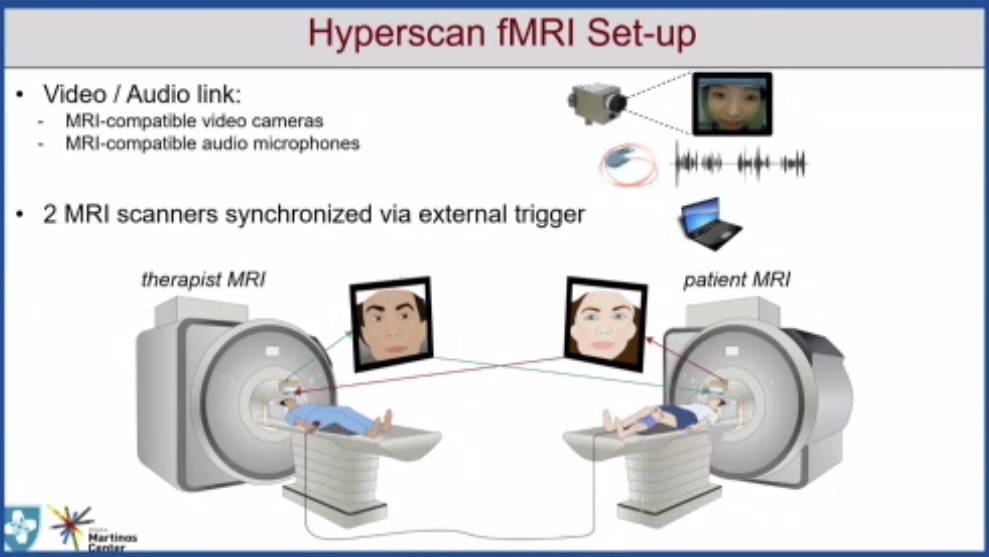
The final plenary talk by Prof. Vitaly Napadow of Harvard Medical School delved into the neurobiological mechanisms underlying psychedelic therapy, focusing on the therapeutic alliance—the empathic connection between patient and clinician.
Using “hyperscanning” neuroimaging, his team simultaneously recorded brain activity in both therapist and patient during treatment. They discovered synchronized activation in regions associated with empathy and social connection—particularly the temporal-parietal junction (TPJ)—correlating with greater pain relief and emotional resilience.
Prof. Napadow’s upcoming FDA-approved MDMA study will further test whether strengthening this brain-to-brain synchrony can amplify clinical benefits in patients with chronic and cancer-related pain. He emphasized that psychedelics should be viewed not merely as drugs but as tools to deepen human connection and enhance the art of medicine.
Integration Into Cancer Care
Panelists agreed that psychedelics are not anticancer agents; they do not shrink tumors or extend survival. Instead, their promise lies in alleviating suffering, restoring agency, and redefining meaning in the face of mortality. The therapy’s structure—comprising preparation, dosing, and integration—requires trained facilitators, careful screening, and ethical oversight.
Future research will focus on optimizing protocols, ensuring accessibility, and exploring group-based and telehealth models for scalable implementation. As Dr. Beaussant summarized, “These substances help patients reconnect—to themselves, to others, and to life—even as they confront death.”
Conclusion: Science, Spirituality, and Suffering
The SIO plenary concluded with a unifying message: psychedelics bridge the biological, psychological, and spiritual dimensions of cancer care. As data mature, oncologists may soon integrate psychedelic-assisted therapy alongside conventional palliative and psycho-oncological approaches—not as an alternative, but as an enhancement of holistic healing.
The speakers collectively called for larger, randomized, controlled trials to validate efficacy, establish safety, and guide clinical practice. For now, this growing body of research signals a paradigm shift: moving from the management of disease to the restoration of wholeness.
For more information clik here.


