Ovarian cancer ranks among the most challenging gynecologic malignancies, consistently presenting at an advanced stage due to nonspecific symptoms. While it remains the fifth most common cause of cancer death among women, advances in surgical techniques, chemotherapy, targeted therapies, and early detection efforts have improved outcomes. The ovarian cancer cure rate continues to climb, offering hope to many patients. However, cure is a complex notion—often defined clinically as complete remission with negligible risk of recurrence after five years. Understanding cure potential requires examining each individual’s cancer type, stage, biology, treatment plan, and overall health.
Read About Ovarian Cancer on OncoDaily
Understanding Cure in Ovarian Cancer
Unlike some other cancers, ovarian cancer frequently returns after initial treatment. As a result, clinicians often frame “cure rate” in terms of long-term remission. Five-year survival rates, stratified by stage, histologic subtype, and response to treatment, serve as practical surrogates for cure. A patient is often considered cured at five years without recurrence, though longer follow-up is ideal. Factors such as subtype (e.g., high-grade serous vs. endometrioid), stage at diagnosis, and response to chemotherapy are pivotal in determining the likelihood of cure (Torre et al., 2018; Lheureux et al., 2019).
Epidemiology and Initial Diagnosis
Globally, ovarian cancer accounts for approximately 300,000 new cases annually and over 180,000 deaths, making it one of the most lethal cancers in women (Torre et al., 2018). Its deadliness is primarily due to late-stage diagnosis; more than two-thirds of cases are detected at Stage III or IV, when the tumor has spread within the pelvis or metastasized beyond (Torre et al., 2018). In high-income countries, slight improvements have been achieved through better surgical care and systemic therapy, but five-year survival remains under 50% overall (Lheureux et al., 2019).
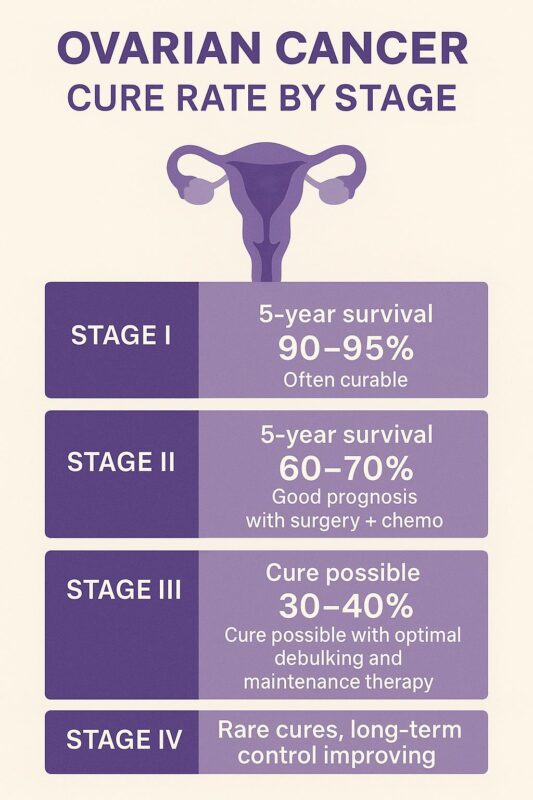
Staging and Survival by Stage
Stage I ovarian cancer is confined to the ovaries. Individual five-year survival rates vary depending on specific factors: Stage IA (cancer in one ovary, no surface involvement) is associated with a survival rate of approximately 90–95%. Stage IB (both ovaries, no spread outside) carries similar rates. Stage IC (surface involvement, capsule rupture, or malignant ascites) reduces survival slightly to 80–85%. Complete surgical staging and adjuvant chemotherapy improve outcomes and significantly increase the likelihood of cure (Tanner et al., 2014; Wright et al., 2017).
Stage II indicates pelvic extension, such as uterus or fallopian tube involvement. Here, five-year survival ranges between 60–70%, depending on surgical success and tumor grade. Optimal debulking surgery plus platinum-based chemotherapy is standard and can lead to long-term remission in many cases (Tanner et al., 2014; Wright et al., 2017).
Stage III involves peritoneal spread into the pelvis or abdomen, while Stage IV denotes distant metastases (e.g., liver parenchyma, pleural effusion, lung nodules). Five-year survival drops to around 30–40% for Stage III and 15–20% for Stage IV (Lheureux et al., 2019). Nonetheless, aggressive cytoreductive surgery achieving no visible residual disease and platinum-taxane chemotherapy have increased cure chances, with some long-term survivors reported (Lheureux et al., 2019; Colombo et al., 2019).
Histologic Subtype and Survival
High-grade serous carcinoma constitutes the majority of ovarian cancers and shows modest improvements in survival with contemporary approaches, including maintenance therapy (Lheureux et al., 2019). Other subtypes—clear cell, mucinous, and low-grade endometrioid—have different prognoses and treatment strategies. Low-grade and early-stage tumors often respond well to surgery alone, whereas clear cell and mucinous subtypes, especially in Stage III/IV, can be resistant to standard chemotherapy, reducing cure rates (Colombo et al., 2019).
Treatment Advances Improving Cure Rates
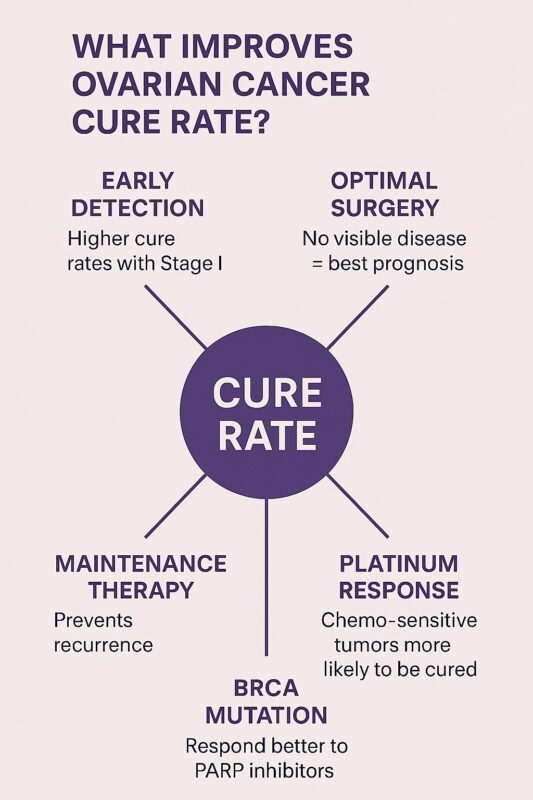
Optimal Cytoreductive Surgery: Surgery aims to remove as much visible cancer as possible. Extensive efforts to achieve no gross residual disease are linked to dramatic improvements in survival. Data show that women with complete cytoreduction who receive adjuvant chemotherapy can have five-year survival rates exceeding 60%, even at Stage III (Chi et al., 2017; du Bois et al., 2019).
Platinum-Based Chemotherapy and Maintenance Therapy: Following surgery, platinum-taxane chemotherapy forms the backbone of treatment. Trials such as SOLO-2/PRIMA demonstrated that adding maintenance therapies—PARP inhibitors (e.g., olaparib, niraparib) or bevacizumab—can significantly prolong progression-free survival and even overall survival. These advancements increase the prospect of cure, especially in patients with BRCA-mutated tumors (Tewari et al., 2018; González-Martín et al., 2019).
Secondary Cytoreduction: For patients who recur after first-line therapy, secondary debulking surgery may lead to improved outcomes, provided it is performed in selected cases with limited disease and favorable prognosis. The DESKTOP III trial established that complete secondary cytoreduction, followed by chemotherapy, significantly enhanced survival compared to chemotherapy alone (Harter et al., 2021).
Targeted Therapy & Personalized Medicine: Tumors harboring BRCA1/2 mutations or homologous recombination deficiency are particularly responsive to PARP inhibitors (e.g., olaparib, rucaparib, niraparib). Studies have reported median progression-free survival approaching 40 months in the frontline maintenance setting—a period conventionally thought indicative of cure—highlighting the potent benefit of precision medicine (González-Martín et al., 2019).
Long-Term Survivor Perspectives
Women who remain disease-free for five years post-treatment, particularly with Stage I–III optimally debulked disease and maintenance therapy, are often considered cured in clinical practice. Data suggest approximately 20% of Stage III patients and fewer Stage IV patients achieve such durable remission (Lheureux et al., 2019; Harter et al., 2021). The late recurrence rate beyond five years remains low, particularly among those who received PARP inhibitor maintenance and achieved optimal cytoreduction (Brown et al., 2020).
Biomarkers and Risk Stratification
Genetic testing for BRCA1/2 mutations now informs frontline management, enabling the use of effective maintenance strategies. Other emerging biomarkers—such as HRD score, CCNE1 amplification, ARID1A mutation, and tumor-infiltrating lymphocytes—are being investigated to refine risk prediction and personalize treatment further (Lheureux et al., 2019; Colombo et al., 2022). As these biomarkers are validated, cure prospects will become increasingly individualized.
Future Directions: Immunotherapy & Novel Agents
Immunotherapy has thus far produced limited success in ovarian cancer. Phase II trials involving anti–PD-1/PD-L1 agents demonstrated modest activity as monotherapy, and large phase III trials combining immunotherapy with chemotherapy or VEGF inhibitors failed to meet primary endpoints (Zamarin et al., 2020). However, combinatorial strategies—PARP inhibitors plus checkpoint inhibitors—and vaccine and cell therapy approaches remain under active investigation, offering potential breakthroughs that could further enhance cure rates.
Read About Immunotherapy for Ovarian Cancer on OncoDaily
Screening and Early Detection
Unlike breast and lung cancer, ovarian cancer lacks effective population-based screening due to non-specific early symptoms and low prevalence. While transvaginal ultrasound and CA-125 monitoring have not demonstrated mortality benefit in average-risk populations, these tools can be used in high-risk women, such as those with BRCA mutations, to detect disease earlier (Buys et al., 2011). Still, early-stage detection remains rare, limiting cure opportunities for most women.
Disparities in Cure Rates
Treatment disparities persist globally. Access to high-volume surgical teams, optimal chemotherapy, and maintenance drugs varies across socioeconomic strata. Women treated at specialized gynecologic oncology centers have better outcomes, underscoring the importance of referral to specialized care (Bruchim et al., 2020; Wright et al., 2018). Overcoming inequities in access to surgery, second-line treatment, and maintenance agents remains vital to improving cure rates across all populations.
Patient-Centered Takeaways
Understanding the landscape of ovarian cancer can empower patients:
- Stage matters: Stage I disease is frequently curable with surgery and possibly chemotherapy. Higher-stage disease requires aggressive, multimodal treatment.
- Surgical success is key: Complete cytoreduction is the strongest prognostic indicator.
- Genetic testing guides treatment: BRCA testing and HRD analysis can identify candidates for PARP maintenance, improving long-term outcomes.
- Maintenance therapy is impactful: PARP inhibitors and bevacizumab extend progression-free survival, bringing many into potential cure territory.
- Specialist care improves outcomes: Referral to high-volume centers and participation in clinical trials enhance survival prospects.
- Immunotherapy is still evolving: It is not yet a standard but likely will play a bigger role with upcoming research.
Conclusion
While ovarian cancer can be a challenging diagnosis due to advanced presentation and risk of relapse, meaningful progress has been made. Cure—understood as long-term remission greater than five years without recurrence—is now achievable for a significant proportion, particularly among women with early-stage disease who undergo complete cytoreduction and receive maintenance therapy. High-grade serous tumors with targeted intervention have shown even more promise. As precision medicine and equitable care delivery evolve, we expect cure rates to continually improve. For every diagnosis, informed treatment decisions and personalized care offer real hope and better outcomes.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD