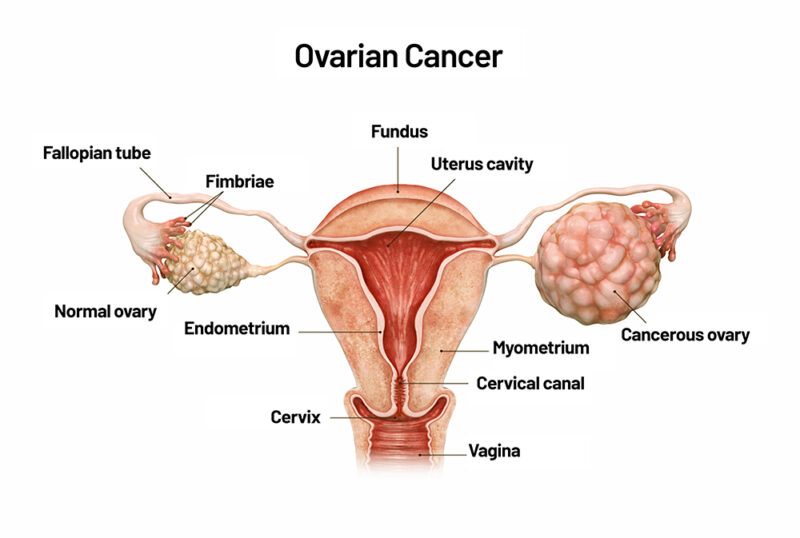
Ovarian cancer is a malignancy originating in the ovarian tissues, which are integral to the female reproductive system. The ovaries are responsible for producing eggs and secreting hormones such as estrogen and progesterone. In 2025, the American Cancer Society estimates that approximately 20,890 women in the United States will receive a new diagnosis of ovarian cancer, and about 12,730 women will die from the disease. The lifetime risk for a woman to develop ovarian cancer is about 1 in 91, with a lifetime chance of dying from it at approximately 1 in 143.
This article aims to provide a comprehensive overview of ovarian cancer, including its symptoms, causes, types, diagnostic methods, staging, and available treatment options. By enhancing awareness and understanding of this disease, we hope to contribute to earlier detection and improved outcomes for those affected.
What Are the Symptoms of Ovarian Cancer?
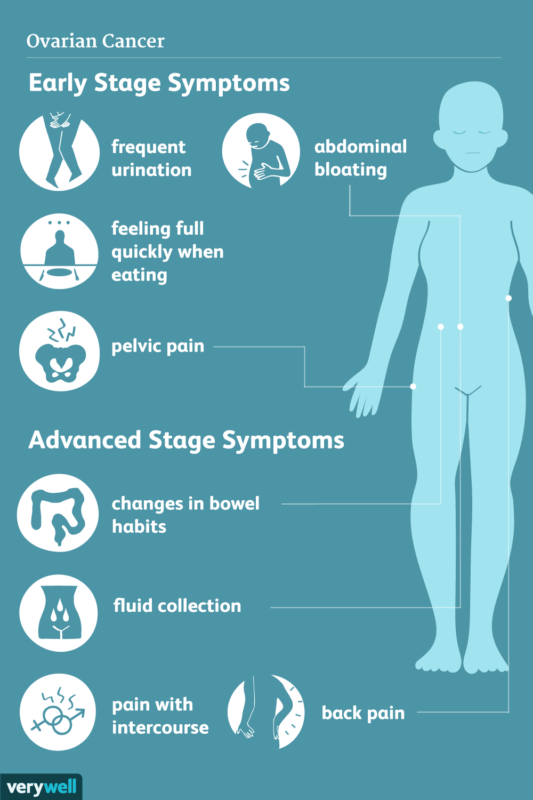
Ovarian cancer often presents with subtle and nonspecific symptoms, which can lead to delayed diagnosis. Common symptoms include persistent bloating, pelvic or abdominal pain, and increased urinary frequency.
- Bloating: Persistent abdominal bloating is a frequent symptom reported by women with ovarian cancer. A study led by Bankhead et al. in the BJOG: An International Journal of Obstetrics and Gynaecology identified persistent abdominal distension as significantly associated with ovarian cancer (odds ratio [OR] 5.2, 95% confidence interval [CI] 1.3–20.5).
- Pelvic or Abdominal Pain: Chronic discomfort in the pelvic or abdominal region is another common manifestation. The same study by Bankhead et al. found that abdominal pain was reported by 77% of women diagnosed with ovarian cancer.
- Frequent Urination: Increased urinary urgency or frequency can occur when an ovarian tumor exerts pressure on the bladder.
The nonspecific nature of these symptoms often leads to misdiagnosis or delayed diagnosis. Research published in the Journal of the American Medical Association by Goff et al. reported that 95% of women with ovarian cancer experienced symptoms prior to diagnosis, yet more than three-fourths were not diagnosed until the disease had advanced to later stages.
What are the Causes and Risk Factors for Ovarian Cancer?
Ovarian cancer arises from a complex interplay of genetic, environmental, and lifestyle factors. Understanding these elements is crucial for identifying at-risk individuals and implementing preventive strategies.
- BRCA1 and BRCA2 Mutations: Inherited mutations in the BRCA1 and BRCA2 genes markedly increase the likelihood of developing ovarian cancer. A study by Kuchenbaecker et al., published in JAMA, reported that by age 80, the cumulative risk for ovarian cancer is approximately 44% for BRCA1 mutation carriers and 17% for BRCA2 mutation carriers.
- Hereditary Breast and Ovarian Cancer Syndrome (HBOC): This syndrome, often resulting from BRCA1 or BRCA2 mutations, predisposes individuals to both breast and ovarian cancers. The Journal of the National Cancer Institute notes that approximately 4% of ovarian cancer patients have a family history of breast cancer, and about 12% have a family history of ovarian cancer.
- Age: The risk of ovarian cancer escalates with age, particularly after menopause. The American Cancer Society indicates that most ovarian cancers develop after menopause, with half of all cases occurring in women aged 63 or older.
- Family History: A family history of ovarian, breast, or colorectal cancer heightens the risk. The American Cancer Society reports that having close relatives with these cancers increases one’s likelihood of developing ovarian cancer.
- Hormone Replacement Therapy (HRT): Postmenopausal use of hormone therapy has been linked to a modestly increased risk of ovarian cancer. A meta-analysis in The Lancet found that women who use HRT for menopause symptoms have about a 40% increased risk of developing ovarian cancer compared to non-users.
- Reproductive History: Factors such as early menstruation, late menopause, and infertility are associated with a higher risk of ovarian cancer. Conversely, pregnancies and the use of oral contraceptives have been shown to reduce the risk. A study in the International Journal of Cancer highlighted that each full-term pregnancy decreases the risk, and long-term use of oral contraceptives can halve the risk of ovarian cancer.
Recognizing these risk factors is essential for early detection and prevention strategies. Individuals with a significant family history or known genetic predispositions are encouraged to seek genetic counseling and consider regular screenings.
What Are the Types of Ovarian Cancer?
Ovarian cancer is categorized into distinct types based on the cell of origin within the ovaries. Understanding these types is crucial for determining appropriate treatment approaches and predicting outcomes. The three main types of ovarian cancer are:
- Epithelial Ovarian Cancer (EOC)
- Germ Cell Ovarian Cancer
- Sex Cord-Stromal Tumors
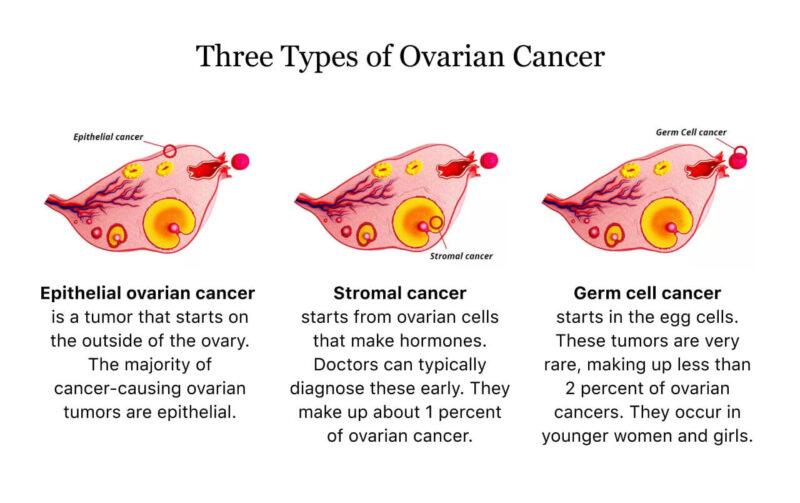
Epithelial Ovarian Cancer
According to an article published in Nature Reviews Clinical Oncology in 2024 by first author Penny Webb, epithelial ovarian cancer is the most prevalent form, accounting for more than 95% of all ovarian cancer cases. This cancer originates from the epithelial cells lining the ovary’s surface and encompasses various histological subtypes, including serous, endometrioid, clear cell, and mucinous carcinomas.
Survival outcomes also differ among histological subtypes of EOC. Research by Wang et al., published in the Journal of the National Cancer Institute, found that low-grade serous carcinoma had the best survival among distant-stage histotypes, with a 10-year survival rate of 37.3% (95% CI = 29.0% to 45.7%). In contrast, carcinosarcoma exhibited the poorest prognosis, with a 10-year survival rate of 29.0% (95% CI = 22.4% to 35.9%).
The prognosis for EOC varies based on factors such as stage at diagnosis A study by Howlader et al., published in BMC Cancer, reported an improvement in the 5-year relative survival rate from 57.2% during 1995–1999 to 63.8% during 2010–2014 (P < 0.001). However, the majority of patients are diagnosed at an advanced stage (70%-80%), where the long-term (10-year) survival rate is poor, estimated at 15%-30%.
Germ Cell Ovarian Cancer
Germ cell ovarian tumors are a rare subset of ovarian cancers, predominantly affecting younger women, particularly those under 30 years of age. These tumors originate from the primordial germ cells of the ovary and encompass various histological subtypes, including dysgerminomas, yolk sac tumors, and immature teratomas.
The prognosis for patients with germ cell ovarian tumors has improved significantly, especially with advancements in treatment modalities. According to data from the American Cancer Society, the 5-year relative survival rate for these tumors is approximately 92% across all stages. Specifically, localized cases have a survival rate of 97%, regional cases 94%, and distant cases 71%.
Sex Cord-Stromal Tumors
According to an article published in Cancers in 2023 by first author Alexis Trecourt, sex cord–stromal tumors are a rare subset of ovarian neoplasms, accounting for approximately 8% of all primary ovarian tumors. These tumors originate from the ovarian stroma and sex cords, which are essential components of the embryonic gonad. They encompass various subtypes, including granulosa cell tumors, Sertoli-Leydig cell tumors, and thecomas. The most common subtype is the granulosa cell tumor, known for its potential to secrete hormones, particularly estrogen. This hormonal activity can lead to symptoms such as irregular menstrual cycles or postmenopausal bleeding.
The prognosis for patients with ovarian germ cell tumors has improved significantly with advancements in treatment. A study published in Cancers in 2023 by first author Yuki Matsumoto reported a 5-year overall survival rate of 98.3% and an event-free survival rate of 84.9% among patients under 39 years old diagnosed with malignant ovarian germ cell tumors.
How Is Ovarian Cancer Diagnosed?
Accurate diagnosis of ovarian cancer involves a combination of clinical evaluations and imaging techniques. Each diagnostic tool plays a specific role in detecting the disease at various stages, contributing to effective management and improved patient outcomes.
- Pelvic Examination: A pelvic exam is often the initial step when ovarian cancer is suspected. During this procedure, a healthcare provider manually examines the uterus, ovaries, and other pelvic organs for abnormalities. However, early-stage ovarian cancers are frequently asymptomatic and may not produce noticeable changes detectable through a pelvic exam. Consequently, the sensitivity of pelvic examinations in identifying early ovarian malignancies is limited.
- Transvaginal Ultrasound (TVUS): TVUS utilizes high-frequency sound waves to create detailed images of the ovaries and surrounding structures. It is particularly useful in distinguishing between solid masses and fluid-filled cysts. According to the American Cancer Society, ultrasound is often the first test performed if an ovarian problem is suspected, as it helps determine the nature of ovarian masses. However, while TVUS is effective in detecting ovarian abnormalities, it cannot definitively determine malignancy.
- Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) Scans:CT and MRI scans provide comprehensive cross-sectional images of the body, aiding in assessing the extent of disease spread. CT scans are particularly useful for evaluating the abdominal and pelvic regions to detect metastases. MRI offers superior soft tissue contrast, which can be advantageous in characterizing adnexal masses. A study by Kinkel et al., published in Radiology, reported that MRI has a sensitivity of 92% and a specificity of 85% in differentiating benign from malignant ovarian masses. These imaging modalities are instrumental in staging the disease and planning surgical interventions.
- Positron Emission Tomography (PET)/CT Scans: PET/CT combines metabolic and anatomical imaging, enhancing the detection of malignant lesions. Research by Grab et al., published in the Journal of Clinical Oncology, demonstrated that PET/CT has an accuracy of 92% in distinguishing malignant from benign ovarian tumors, compared to 83% for pelvic ultrasound. Despite its high accuracy, PET/CT is not routinely used for initial diagnosis due to cost and availability constraints but is valuable in evaluating suspected metastases and recurrent disease.
- Biopsy: Definitive diagnosis of ovarian cancer is achieved through histopathological examination of tissue samples. Biopsies are typically performed during surgical procedures, such as laparotomy or laparoscopy, where suspicious tissues are excised and analyzed microscopically. The Canadian Cancer Society emphasizes that a biopsy is the only way to confirm an ovarian cancer diagnosis. Preoperative biopsies are generally avoided to prevent potential spread of malignant cells.
Genetic Testing for Ovarian Cancer
Genetic testing for BRCA1 and BRCA2 mutations is crucial for women at high risk of ovarian cancer, as it significantly influences both preventive and therapeutic strategies. Women carrying harmful mutations in BRCA1 or BRCA2 genes face a markedly increased risk of developing ovarian cancer. The National Cancer Institute reports that approximately 39%–58% of women with a BRCA1 mutation and 13%–29% with a BRCA2 mutation will develop ovarian cancer in their lifetime, compared to about 1.1% in the general population.
Identifying BRCA mutations not only aids in assessing cancer risk but also informs treatment choices. For instance, the use of PARP inhibitors, a class of targeted therapy, has shown efficacy in treating BRCA-mutated ovarian cancers. A study highlighted by the National Cancer Institute found that individuals with harmful BRCA1 or BRCA2 mutations who underwent risk-reducing bilateral salpingo-oophorectomy experienced a lower risk of dying from ovarian and breast cancers.
Early identification of BRCA mutations allows for proactive measures to mitigate cancer risk. Preventive options include increased surveillance, chemoprevention, or prophylactic surgeries. The National Cancer Institute notes that prophylactic mastectomy can reduce the risk of breast cancer by over 90%, and prophylactic oophorectomy has a similar effect on ovarian cancer risk.
What Are the Treatment Options for Ovarian Cancer?
Treatment for ovarian cancer involves a multidisciplinary approach, with several therapeutic options tailored to the cancer type, stage, and individual patient factors. The primary treatment methods include:
- Surgery: Surgery is often the first line of treatment and involves the removal of as much of the tumor as possible, known as debulking. The extent of surgery depends on the cancer’s stage and spread.
- Chemotherapy: Chemotherapy uses powerful drugs to kill cancer cells or prevent them from dividing. It is typically administered after surgery (adjuvant chemotherapy) or before surgery (neoadjuvant chemotherapy) in certain cases.
- Radiation Therapy: Though less commonly used for ovarian cancer, radiation therapy employs high-energy rays to target and destroy cancer cells, particularly in cases where cancer has spread or for symptom management.
- Targeted Therapy: This treatment focuses on specific genetic mutations or molecular markers present in cancer cells. PARP inhibitors, for instance, are commonly used in patients with BRCA mutations.
- Hormone Therapy: In some cases, hormone-blocking treatments may be used, especially for certain rare types of ovarian cancers that are hormone-sensitive.
Surgical Options for Ovarian Cancer
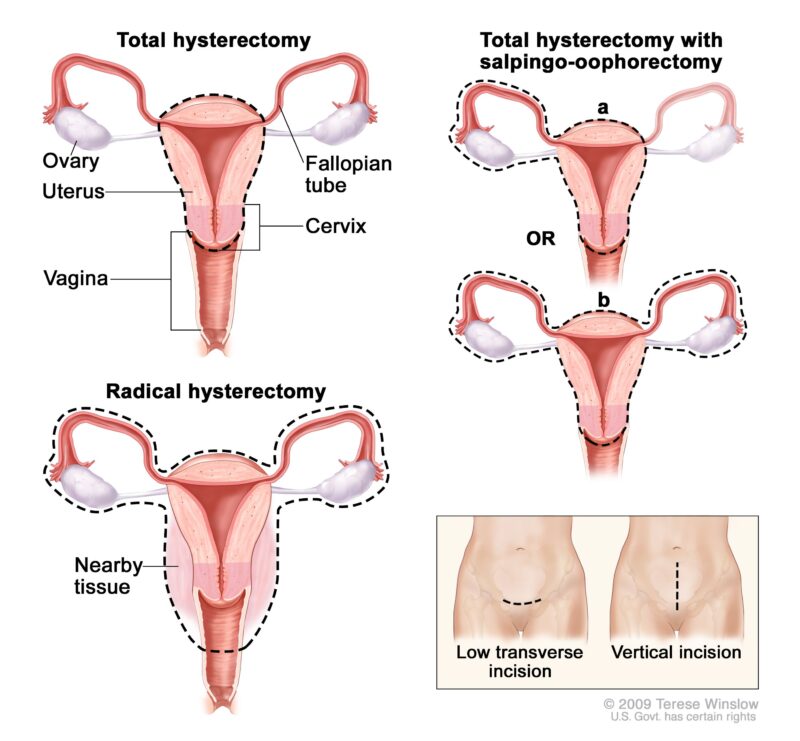
Surgical intervention is a cornerstone in the management of ovarian cancer, with procedures tailored to the disease’s stage and the patient’s overall health. The primary surgical options include hysterectomy and oophorectomy, each serving distinct purposes in treatment.
- Hysterectomy: A hysterectomy involves the removal of the uterus and is often performed when ovarian cancer has spread to or involves the uterus. This procedure may be part of a comprehensive surgical approach, including the removal of ovaries and fallopian tubes (salpingo-oophorectomy), especially in advanced stages of ovarian cancer. Recovery typically spans four to six weeks, during which patients may experience discomfort, fatigue, and limitations in daily activities. Risks associated with hysterectomy include infection, bleeding, and injury to surrounding organs. Additionally, premenopausal women will enter menopause post-surgery, leading to symptoms such as hot flashes and increased risk of osteoporosis. According to the American Cancer Society, patients whose tumors have been optimally debulked, which may include hysterectomy, have a better prognosis than those with residual larger tumors.
- Oophorectomy: Oophorectomy entails the surgical removal of one or both ovaries and is indicated in cases where cancer is confined to the ovaries or as a preventive measure for high-risk individuals carrying BRCA1 or BRCA2 gene mutations. Recovery time is similar to that of a hysterectomy, approximately four to six weeks. Potential risks include infection, bleeding, damage to adjacent organs, and, if both ovaries are removed, immediate onset of menopause with its associated symptoms. The Mayo Clinic notes that prophylactic oophorectomy can significantly reduce the risk of ovarian cancer in high-risk women but may increase the risk of cardiovascular disease and osteoporosis, particularly if performed before age 45.
- Cytoreduction: Cytoreductive surgery aims to remove as much of the tumor mass as possible, especially in advanced stages where complete resection isn’t feasible. This approach enhances the effectiveness of adjunct therapies like chemotherapy. Optimal debulking, where minimal residual disease remains, is associated with improved survival rates. Recovery can be extensive due to the complexity of the surgery, with potential risks including infection, bleeding, and organ dysfunction. The American Cancer Society emphasizes that patients whose tumors have been optimally debulked have a better prognosis than those with larger residual tumors after surgery.
Chemotherapy for Ovarian Cancer
Chemotherapy plays a pivotal role in the management of ovarian cancer, especially in advanced stages. It involves the use of cytotoxic drugs to eradicate cancer cells, reduce tumor burden, and prevent disease progression.
In advanced epithelial ovarian cancer, chemotherapy is typically administered after surgical intervention to address residual disease. The standard regimen often includes a combination of platinum-based compounds, such as carboplatin, and taxanes, like paclitaxel. This approach aims to target microscopic cancer cells that may remain post-surgery, thereby enhancing overall survival rates. However, despite initial responsiveness, recurrence is common, with studies indicating that advanced epithelial ovarian cancer often recurs months or years after the initial treatment. In such cases, additional chemotherapy may be recommended, with the choice of drugs depending on the duration of remission and previous treatments.
Research published in the Journal of Clinical Oncology indicates that the addition of bevacizumab (a targeted therapy) to standard chemotherapy significantly improves overall survival in patients with advanced ovarian cancer. The study reported a hazard ratio of 0.62, suggesting a 38% reduction in the risk of death.
Chemotherapy affects both malignant and healthy rapidly dividing cells, leading to a range of side effects. Common adverse effects include:
- Gastrointestinal Symptoms: Nausea, vomiting, and loss of appetite are frequently observed. These symptoms can often be managed with antiemetic medications.
- Hematologic Effects: Bone marrow suppression can result in anemia, increased susceptibility to infections, and easy bruising or bleeding due to decreased blood cell counts.
- Alopecia: Hair loss is a common and distressing side effect, typically occurring within weeks of initiating treatment.
- Neuropathy: Some chemotherapeutic agents, particularly paclitaxel, can cause peripheral neuropathy, manifesting as numbness, tingling, or pain in the extremities.
Long-term survivors may experience persistent side effects. A study published in the Journal of Clinical Oncology reported that moderate-to-severe fatigue, sleep disturbances, neurotoxicity, and anxiety affected 20%–30% of patients even at 42 months post-treatment.
Recent Advancement in Breast Cancer
Recent advancements in ovarian cancer research have led to significant improvements in early detection and treatment strategies, offering hope for better patient outcomes.
A groundbreaking blood test developed by the University of Queensland’s Centre for Extracellular Vesicle Nanomedicine has shown a 94% accuracy rate in detecting early-stage ovarian cancer. This test analyzes extracellular vesicles to identify cancer presence and is currently undergoing clinical trials with 1,500 women to validate its effectiveness. Researchers at the University of Oxford have secured funding from Cancer Research UK to develop OvarianVax, the world’s first vaccine aimed at preventing ovarian cancer. This vaccine is designed to train the immune system to recognize and attack early-stage ovarian cancer cells, with human clinical trials expected to commence within the next five years.
The FDA has approved mirvetuximab soravtansine (Elahere), an antibody-drug conjugate targeting folate receptor-alpha, for treating platinum-resistant ovarian cancer. Clinical trials have demonstrated its efficacy in patients who have undergone multiple prior treatments. GSK’s recent trial combining Jemperli (dostarlimab) with standard chemotherapy and Zejula (niraparib) as maintenance therapy has shown improved progression-free survival in advanced ovarian cancer patients. While overall survival benefits were not statistically significant, the combination therapy represents a promising avenue for treatment. Studies on interferon epsilon (IFNε) have revealed its potential in instructing immune cells to target and eliminate ovarian cancer cells, offering a multifaceted defense against tumor growth. This discovery opens new possibilities for immunotherapy treatments in ovarian cancer.
What Are the Stages of Ovarian Cancer?
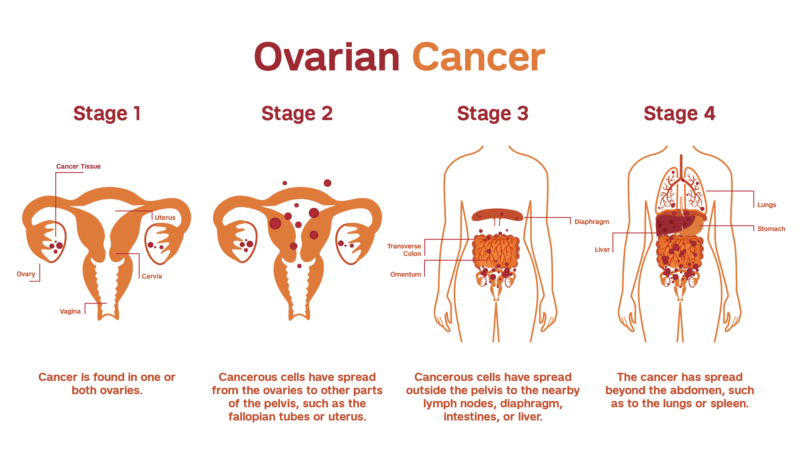
Ovarian cancer is classified using a staging system that reflects how far the disease has spread at diagnosis. This system helps guide treatment decisions and predict outcomes.
- Stage I (Localized): In this early stage, cancer is confined to one or both ovaries. It is often divided into sub-stages: Stage IA (limited to one ovary), Stage IB (present in both ovaries), and Stage IC (cancer is found on the ovary’s surface, or cells are detected in abdominal fluid). Survival rates are highest at this stage due to the localized nature of the disease.
- Stage II (Regional Spread): Here, cancer has spread beyond the ovaries to nearby pelvic organs, such as the uterus or fallopian tubes. This stage is also broken down into IIA (spread to the uterus or fallopian tubes) and IIB (involvement of other pelvic tissues). The disease remains within the pelvis but indicates a more advanced local spread.
- Stage III (Abdominal Spread): Cancer has now extended beyond the pelvis into the abdominal cavity, possibly involving lymph nodes or tissues like the peritoneum. Stage III is further classified into IIIA (microscopic spread), IIIB (visible tumors under 2 cm), and IIIC (tumors larger than 2 cm or lymph node involvement). This stage is often diagnosed due to more noticeable symptoms like bloating and pain.
- Stage IV (Metastatic): The most advanced stage, where cancer has spread to distant organs beyond the abdomen, such as the liver, lungs, or other distant lymph nodes. It is divided into IVA (fluid buildup containing cancer cells around the lungs) and IVB (spread to other organs). Treatment focuses on controlling the disease and alleviating symptoms.
After Treatment: What to Expect
The post-treatment phase of ovarian cancer focuses on recovery, managing side effects, and preventing recurrence. Physically, patients often experience fatigue, changes in appetite, and weakness, which may persist for weeks or months. For those who underwent surgery or chemotherapy, fertility issues can also arise, especially if both ovaries were removed or if treatment affected hormone levels.
Ongoing monitoring is essential to detect any signs of recurrence. Experts from the American Cancer Society recommend regular follow-up visits every 3–6 months for the first two years, which include physical exams, imaging tests, and blood tests (such as CA-125 levels). Lifestyle changes can aid recovery and reduce recurrence risk. A balanced diet, regular exercise, and stress management are encouraged. Support groups and counseling can also help address the emotional challenges faced during recovery.
How Long Does It Take to Notice and Cure Ovarian Cancer?
Recognizing ovarian cancer symptoms and promptly seeking medical attention are crucial for early diagnosis and effective treatment. The journey from symptom onset to diagnosis and subsequent treatment involves several stages, each with its own timeline and recovery considerations.
- Symptom Recognition to Diagnosis: Ovarian cancer often presents with subtle symptoms, leading to potential delays in diagnosis. A study published in the Journal of the American Medical Association by first author Barbara A. Goff found that women with ovarian cancer reported symptoms such as bloating, abdominal pain, and urinary urgency for a median duration of 3 to 6 months before diagnosis. This highlights the importance of early symptom recognition and prompt medical evaluation.
- Surgery: Surgical intervention is a primary treatment modality for ovarian cancer. According to the American Cancer Society, most patients undergoing ovarian cancer surgery require a hospital stay of 3 to 7 days. Full recovery can take approximately 6 to 12 weeks, depending on the extent of the surgery and individual patient factors.
- Chemotherapy: Chemotherapy is often administered after surgery to target residual cancer cells. The American Cancer Society notes that chemotherapy is typically given in cycles, with each cycle lasting 3 to 4 weeks. The total number of cycles varies but often ranges from 3 to 6, extending the chemotherapy course over several months.
- Monitoring and Follow-Up: Post-treatment, regular follow-up is essential to monitor for recurrence and manage any ongoing side effects. The American Cancer Society recommends that patients have follow-up visits every 2 to 4 months for the first two years after treatment, then every 3 to 6 months for the next three years, and annually thereafter. These visits typically include physical examinations, imaging tests, and blood tests to detect any signs of cancer returning.
Understanding these timelines and adhering to recommended follow-up care can significantly impact outcomes and quality of life for ovarian cancer patients.
Can Ovarian Cancer Be Prevented?
Preventing ovarian cancer involves a mix of proactive measures, especially for women at higher risk. Regular screenings, such as transvaginal ultrasounds and CA-125 blood tests, are recommended for those with genetic predispositions but are not effective for routine screening in the general population. Genetic testing for BRCA1 and BRCA2 mutations plays a vital role in identifying high-risk individuals. A study by Susan M. Domchek in the Journal of the National Cancer Institute showed that preventive surgeries, like risk-reducing salpingo-oophorectomy, lower the risk by 80%–90% in women with these mutations.
Lifestyle changes also help reduce risk. The American Cancer Society reports that using oral contraceptives for five or more years can cut ovarian cancer risk by up to 50%. Additionally, factors like full-term pregnancies, breastfeeding, maintaining a healthy weight, and staying active contribute to lowering risk. While no method guarantees prevention, combining medical advice with healthy habits offers the best protection.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What Is Ovarian Cancer?
Ovarian cancer is a type of cancer that begins in the ovaries, responsible for producing eggs and hormones like estrogen and progesterone.
What Are the Early Symptoms of Ovarian Cancer?
Common symptoms include bloating, pelvic pain, frequent urination, and difficulty eating or feeling full quickly.
What Causes Ovarian Cancer?
The exact cause is unknown, but risk factors include age, family history, genetic mutations (BRCA1/BRCA2), and hormone replacement therapy.
What Are the Stages of Ovarian Cancer?
Ovarian cancer has four stages, from localized (Stage I) to widespread metastasis (Stage IV).
How Is Ovarian Cancer Diagnosed?
Diagnosis often involves pelvic exams, ultrasound, CT scans, blood tests (like CA-125), and biopsy confirmation.
What Are the Types of Ovarian Cancer?
Main types include epithelial ovarian cancer, germ cell tumors, and stromal cell tumors, each with distinct characteristics.
How Is Ovarian Cancer Treated?
Treatment typically involves surgery, chemotherapy, targeted therapy, or a combination of these, depending on the cancer’s stage and type.
What Is the Survival Rate for Ovarian Cancer?
The 5-year survival rate is about 49%, but early-stage detection significantly improves outcomes.
Can Ovarian Cancer Be Prevented?
While not entirely preventable, risk-reducing strategies include using birth control pills, tubal ligation, and genetic testing for high-risk individuals.
Does Ovarian Cancer Have a Genetic Link?
Yes, mutations in genes like BRCA1 and BRCA2 increase the risk, and genetic counseling can help assess individual risk levels.