Chemotherapy is a cornerstone in the treatment of many cancers, offering hope for patients with various malignancies. However, while effective in targeting cancer cells, chemotherapy can also cause a range of side effects, including ocular toxicity. Chemotherapy and ocular side effects are often overlooked but can significantly impact a patient’s quality of life. These effects can range from mild discomfort, like dry eyes or blurred vision, to more severe conditions that threaten vision. Understanding the potential ocular side effects of chemotherapy, their causes, and how they can be managed is essential for improving patient care and ensuring optimal outcomes.
René Magritte The False Mirror 1929, oil on canvas 54×81 sm
This article explores the relationship between chemotherapy and eye toxicity, providing insights into prevention, monitoring, and treatment options for those affected. Moreover, the importance of collaboration between the patient, oncologist, and ophthalmologist cannot be overstated. A multidisciplinary approach helps ensure timely detection, effective management, and better outcomes for patients experiencing ocular toxicity during chemotherapy.
What Are the Origins of Chemotherapy?
Chemotherapy originated in the early 20th century through experiments on tumors in rodents. In the early 1900s, Paul Ehrlich introduced the concept of chemotherapy, initially for treating diseases like syphilis, using animal models. During World War I, exposure to mustard gas led to the discovery of nitrogen mustard as a potential cancer treatment. The modern chemotherapy era began in the 1940s with the introduction of nitrogen mustard and folic acid antagonists.
In 1942, nitrogen mustard was first used to treat non-Hodgkin’s lymphoma, and in 1949, mechlorethamine became the first FDA-approved chemotherapy drug. In the 1950s, Sidney Farber demonstrated that aminopterin, a folic acid derivative, could induce leukemia remission in children, and in 1953, researchers at the National Cancer Institute achieved the first complete cure of a solid tumor using chemotherapy. The 1960s saw the rise of combination chemotherapy, leading to curative treatments for childhood leukemia, Hodgkin’s disease, and germ cell cancers.

Dr. Jonathan Hartwell (right) and his assistant Sylvy R. Levy Kornberg conduct some of the earliest chemotherapy tests at the National Cancer Institute, about 1950.
What is Ocular Toxicity?
Systemic chemotherapy can lead to damage in multiple organs, including the heart, lungs, central nervous system, bones, and bone marrow. As more aggressive and combination chemotherapy regimens are used across different cancer stages, ocular adverse reactions have become increasingly recognized. The ocular surface relies on constant homeostasis for proper function. However, in combination therapies, identifying the specific agent responsible for an ocular adverse effect is challenging, often leading to underreporting of these reactions.
Ocular toxicities are common challenges with anticancer agents, including small molecules, antibody-drug conjugates (ADCs), and targeted antibodies, particularly those directed against Epidermal Growth Factor Receptor (EGFR), Mitogen-Activated Protein Kinase (MEK), and Cytotoxic T-Lymphocyte-Associated Protein 4 (CTLA-4).
Why is the Eye Sensitive to Chemotherapy?
The eye is highly sensitive to toxic effects due to several anatomical and physiological factors. Its unique structure consists of delicate tissues, such as the cornea, retina, and lens, which have limited regenerative capacity and are highly susceptible to damage. The specialized blood-ocular barrier regulates substance entry but can be disrupted by toxins, leading to inflammation and injury. The eye has a high metabolic demand, especially in retinal cells, making it vulnerable to toxic agents that interfere with cellular function. Constant exposure to environmental factors like UV radiation and pollutants can further amplify systemic toxic effects. Furthermore, the eye’s close connection to the nervous system means that neurological toxins can cause ocular symptoms, including photophobia and visual disturbances.

Mechanisms of Ocular Toxicity.
Chemotherapeutic agents can cause ocular toxicity through several mechanisms. Direct cytotoxicity affects ocular tissues like the cornea and conjunctiva, damaging epithelial cells and leading to conditions such as keratitis and conjunctivitis. Inflammation is another key mechanism, with chemotherapy triggering immune responses or direct tissue damage, resulting in conditions like uveitis and scleritis. Neurotoxicity can impact the optic nerve and oculomotor nerves, causing visual disturbances, as observed with vincristine. Chemotherapy can alter tear film composition, leading to dry eye syndrome. Vascular effects on retinal vasculature may cause retinal hemorrhages or ischemia. Lastly, metabolic changes induced by chemotherapy, such as altered blood flow and oxygenation, can negatively affect retinal health and function.
Ocular Side Effects of Chemotherapy Drug Groups
Alkylating Agents
Alkylating Agents are a class of chemotherapy drugs that function by substituting hydrogen atoms in organic compounds with alkyl groups. These agents are commonly used to treat a variety of cancers, including leukemia, lymphoma, and solid tumors. Cyclophosphamide, a widely used alkylating agent, has ocular side effects such as keratoconjunctivitis sicca, blepharoconjunctivitis, and reversible epiphora, particularly in breast cancer patients. Blurred vision episodes have been reported, affecting approximately 17% of patients following an initial dose. Cyclophosphamide is frequently prescribed for leukemias, malignant lymphomas, and solid tumors like breast cancer. Abbas Bader Future Sci OA 2023
Oxaliplatin, another alkylating agent, causes ocular side effects including hyperlacrimation, conjunctivitis, decreased visual acuity, and narrowing of the visual field. It is commonly used for locally advanced pancreatic cancer, metastatic disease, advanced esophageal and ovarian cancers, relapsed non-Hodgkin’s lymphoma, palliative treatment of testicular cancer, and advanced colorectal cancer. Busulfan has been associated with keratoconjunctivitis sicca in patients undergoing treatment for chronic myeloid leukemia and other myeloproliferative disorders. Jun Elena Andreea Stoicescu J Med Life 2023
Antimetabolites and Mitotic Inhibitors and Antibiotics
Antimetabolites and Mitotic Inhibitors are chemotherapy agents that disrupt the growth of rapidly dividing cancer cells, commonly used for treating cancers like breast, head and neck, and gastrointestinal tumors. Methotrexate causes blepharitis, conjunctivitis, photophobia, periorbital edema, blurred vision, optic nerve and retinal changes, cataracts, and excessive lacrimation. Methotrexate is used for treating breast cancer, head and neck cancer, osteosarcoma, acute leukemia, and other malignancies. Ocular toxicity is relatively rare but can be severe.
Pemetrexed associated with visual field defects and ischemic optic neuropathy. It is used as monotherapy for advanced or metastatic non-small cell lung cancer or in combination with cisplatin for unresectable malignant pleural mesothelioma. Ocular side effects are less common compared to other antimetabolites but can include increased lacrimation and conjunctivitis 5-Fluorouracil (5-FU), an antimetabolite, is associated with ocular side effects such as blurred vision, loss of vision, ocular pain, photophobia, epiphora, eye irritation, conjunctivitis, and keratitis. Permanent intractable epiphora can occur due to canalicular fibrosis. Although 5-FU is detected in tears after intravenous administration, the concentrations do not correlate with ocular toxicity.
Capecitabine, also an antimetabolite, is linked to ocular surface adverse effects including decreased visual acuity, corneal deposits, eye irritation, tear duct stenosis, conjunctivitis, and blepharitis. This drug is commonly used for colorectal, gastric, and breast cancers.Mitotic inhibitors, such as Docetaxel, disrupt cell division by interfering with microtubules, often causing epiphora, conjunctivitis, and optic neuropathy. Nasolacrimal duct obstruction is a common issue, leading to excessive tearing. Antibiotics like Doxorubicin, an anthracycline, are frequently used for treating various cancers. It can cause ocular side effects such as conjunctivitis and epiphora. Abbas Bader Future Sci OA 2023
Monoclonal Antibodies and Targeted Therapies
Monoclonal antibodies and targeted therapies are essential treatments for various cancers, including lymphomas, by specifically targeting proteins involved in cancer growth.
Rituximab, a monoclonal antibody, is commonly used to treat non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and rheumatoid arthritis. It is associated with ocular side effects such as conjunctivitis, excessive tearing, and decreased vision. More severe ocular complications, including acute retinal necrosis and progressive outer retinal necrosis, have been reported, particularly in immunocompromised patients. Transient bilateral conjunctivitis has also been observed.Bevacizumab, primarily used for its anti-vascular endothelial growth factor (VEGF) effects, is linked to ocular side effects, especially when administered intravitreally. These effects include retinal artery occlusion and hemorrhagic macular infarction.Brolucizumab, another monoclonal antibody, has been associated with retinal vasculitis, which presents with arterial sheathing and retinal whitening. Helio V. Neves da Silva SageJournals 2022
Targeted therapies are newer agents designed to interfere with the molecular mechanisms driving cancer cell proliferation and survival. They provide more precise and potentially less toxic alternatives to traditional chemotherapy but can still cause significant ocular side effects.Vemurafenib, used primarily for treating advanced melanoma with a BRAF V600E mutation, is known to cause uveitis, retinal vein occlusion, and photophobia, affecting approximately 45.5% of patients.The Dabrafenib/Trametinib combination therapy is linked to uveitis and central serous chorioretinopathy, affecting 18.5% and 7.4% of patients, respectively. Clara M Castillejo Becerra BMJ Open Ophtalmology 2020
Trametinib can cause blurry vision, dry eye, transient vision loss, eye floaters, and visual halo. Rare reports also include retinal venous occlusion and retinal pigment epithelial detachment.Vandetanib is associated with blurry vision due to corneal opacities.Pemigatinib has been linked to bilateral multifocal serous retinopathy and subretinal accumulation, leading to serous retinal detachment. Symptoms may resolve upon discontinuation of the drug.
Diagnostic Approaches of Ocular Side effects
Regular assessment of new or worsening visual symptoms, such as blurred vision, dryness, tearing, or pain, helps identify early signs of ocular toxicity. Specialized testing, including slit-lamp biomicroscopy for corneal changes, optical coherence tomography (OCT) to evaluate retinal and optic nerve health, and fundus photography or fluorescein angiography for deeper retinal assessments if needed, can aid in early detection.
The OCT testing system can precisely track the blood vessels of each patient’s eye, ensuring high-quality imaging tailored to individual anatomy. This advanced tracking allows for scans to be performed in the exact same location as previous ones, with an accuracy within one micron, enabling the detection of even the slightest changes over time. The Posterior Segment OCT test is commonly used for evaluating conditions such as macular degeneration, multiple sclerosis, visual disturbances, and drusen.Periodic eye exams during chemotherapy, particularly for agents with known ocular risks, are recommended to monitor for reversible conditions like dry eye or more severe complications such as macular edema or optic neuropathy.
A 70-year-old man with a history of neuroendocrine bladder cancer, previously treated with carboplatin and etoposide, presented four weeks after completing his fourth chemotherapy cycle with a one-week history of blurred vision in his right eye. A similar episode had occurred in his left eye two weeks after his third cycle. Suspecting carboplatin-induced ocular toxicity, chemotherapy was discontinued, and his vision remained stable thereafter. Ng J, Journal of Oncology Pharmacy Practice. 2023
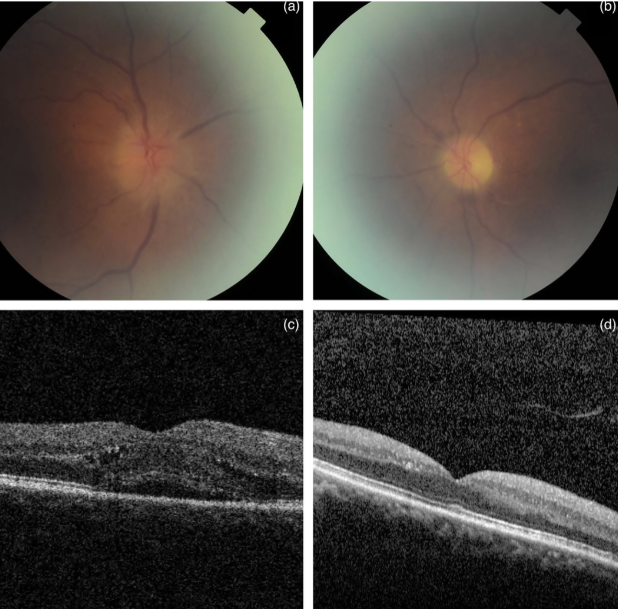
(a) Fundal examination showed segmental disc swelling superiorly associated with disc haemorrhage in OD. (b) Atrophic optic disc associated with sclerosed branch retinal artery was noted in the OS. (c and d) Optical coherence tomography showed subretinal fluid and intraretinal fluid in OD which resolved spontaneously 1 month later.
How to Know If It’s Chemotherapy Ocular Side Effects or Not?
Differentiating chemotherapeutic drug-induced ocular toxicities from ocular manifestations of metastatic disease or paraneoplastic syndromes is crucial for effective management. A structured approach involves assessing clinical history, symptom onset, and diagnostic findings. Documenting the specific chemotherapeutic agents, dosage, and duration is essential, as symptoms that arise shortly after treatment initiation are more likely drug-related.
Common chemotherapy-induced ocular toxicities include dry eyes, conjunctivitis, blurred vision, and retinal changes such as hemorrhages or edema, which may be reversible upon drug discontinuation. In contrast, metastatic disease may present with gradual vision loss, painful eye symptoms, and diplopia due to cranial nerve involvement. Paraneoplastic syndromes should be evaluated by testing for associated antibodies, such as anti-retinal antibodies, to differentiate them from direct drug toxicity. In cases of suspected metastatic disease, a tissue biopsy may be necessary to confirm the presence of malignant cells.
You Can Also Read Antibody-Drug Conjugates and Their Ocular Effects in Cancer Treatment: Efficacy and Toxicity by OncoDaily
Is Chemotherapy Dose Changed Due to Ocular Side Effects?
Dose adjustment guidelines for chemotherapy-induced ocular toxicity involve different approaches depending on severity. For mild cases, such as mild conjunctivitis, regular monitoring without immediate intervention may be sufficient. In more severe cases, including confluent keratitis, withholding the chemotherapy dose until symptoms resolve is recommended, followed by resuming treatment at a reduced dose to minimize recurrence. For the most severe reactions, such as ulcerative keratitis or significant visual impairment, discontinuation of chemotherapy is strongly advised to prevent further ocular damage and preserve vision.
How to Prevent Ocular Side Effects of Chemotherapy
Regular eye examinations are crucial for the early detection and management of ocular side effects of chemotherapy, helping to prevent vision-related complications.. Many ophthalmic side effects can be reversed if identified early. Patients should be vigilant for symptoms such as sudden vision changes, light sensitivity, and eye infections. Severe issues like significant vision loss or intense eye pain require immediate medical attention. Regular comprehensive eye exams help detect abnormalities that may otherwise go unnoticed, allowing for timely intervention and reducing the risk of serious vision impairment.
Early consultation with an oncologist and ophthalmologist is crucial for managing ocular adverse effects.
Oncologists and Ophthalmologists: Partnering to Safeguard Ocular Health in Cancer Patients
Collaboration between oncologists and ophthalmologists is crucial in managing ocular side effects of chemotherapy, which can significantly impact a patient’s quality of life. Ophthalmologists play a key role in the early detection and management of these toxicities by regularly monitoring patients—ideally at baseline and every three months thereafter—to identify any emerging issues. Timely interventions, including dose adjustments and supportive treatments like artificial tears, can help mitigate these side effects.
A collaborative approach involves oncologists referring patients to ophthalmologists when ocular symptoms arise to differentiate between toxicity and metastases, joint management strategies such as chemotherapy dose modifications, and educating patients on the importance of reporting any visual changes during treatment. This teamwork ensures better patient outcomes and helps preserve ocular health throughout chemotherapy.
You can Also watch Integrative Medicine for Chemotherapy-Induced Neuropathy | ASCO 2024 by OncoDaily
Written by Margarita Pozlikyan MD
FAQ
What are common eye-related complications caused by cancer treatment?
Common side effects include dry eye syndrome, uveitis, conjunctivitis, keratitis, blurred vision, and tearing. Other effects can be retinal detachment, cataracts, and photophobia.
Which cancer drugs cause ocular toxicity?
Drugs like cisplatin, 5-fluorouracil, cyclophosphamide, tamoxifen, and interferon are known to cause ocular toxicity. Newer agents such as immune checkpoint inhibitors and targeted therapies can also lead to ocular issues.
How can eye toxicity be managed?
Regular eye exams are crucial for early detection. Symptoms can be treated symptomatically, but severe cases may require discontinuation of the drug. Adjusting doses or stopping the medication can often resolve temporary effects.
How often should patients on chemotherapy undergo eye exams?
Patients should undergo baseline eye exams and follow-up exams every three months to monitor for ocular toxicity.
Does chemotherapy always causes hair loss?
Hair loss during chemotherapy depends on the type and dosage of the drugs used. Not all chemotherapy treatments cause hair loss. While some patients may experience significant hair loss, others may not lose hair at all.
Can chemotherapy cause permanent vision loss?
While chemotherapy can cause ocular toxicities, permanent vision loss is rare. However, certain drugs like Methotrexate and Tamoxifen have been associated with severe ocular side effects, including optic neuropathy and retinal changes. Early detection and discontinuation of the offending drug can often prevent permanent damage. Regular ophthalmological monitoring is crucial for patients undergoing chemotherapy to ensure early intervention if needed.
What are the common ocular side effects of targeted therapies?
Targeted therapies can cause a range of ocular side effects, including conjunctivitis, dry eyes, visual disturbances, and periorbital edema. For example, Imatinib is known for causing periorbital edema and hyperlacrimation, while Gefitinib can lead to conjunctivitis and dry eyes. These side effects are generally manageable with appropriate care.