Myositis—inflammation of the skeletal muscles—is one of the rarer but more serious immune-related adverse events (irAEs) linked to immune checkpoint inhibitors (ICIs). These agents, including ipilimumab and nivolumab, have dramatically reshaped the treatment landscape for advanced cancers such as melanoma by blocking inhibitory pathways like CTLA-4 and PD-1, thereby unleashing the immune system against tumors. However, this immune re-activation comes with a price: a diverse range of irAEs that can target almost any organ system.
But what happens when a patient develops severe myositis… and CK stays perfectly normal?
Authors: Klajdi Begaj, Raphael Wilhelm, Alisa Lepper, Maike Kaufhold, Jakob Veeser, Stephan Grabbe, Henner Stege
Published: Frontiers in Oncology
The Case
A 58-year-old woman with advanced melanoma had already navigated a complex cancer journey—tumor excision, lymph node dissection, targeted BRAF/MEK therapy, radiosurgery for brain metastases, and combined ipilimumab-nivolumab immunotherapy. She had previously developed immune-mediated colitis, which resolved with steroids.
By mid-2024, her scans were clear, and nivolumab was stopped. Two months later, without any active cancer treatment, she began experiencing progressive hip and lower back muscle pain, followed by significant weakness that made walking difficult.
The Diagnostic Challenge
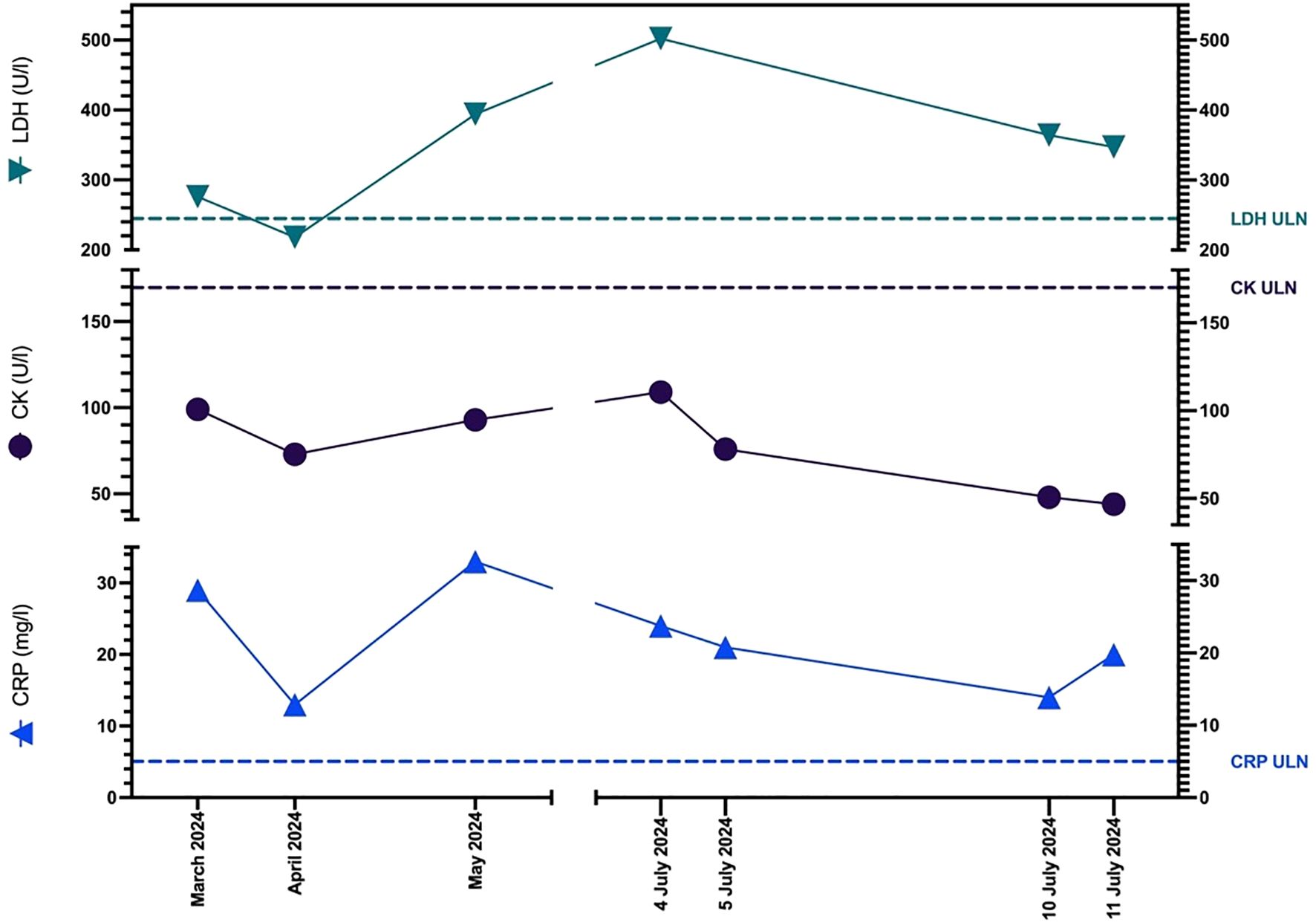
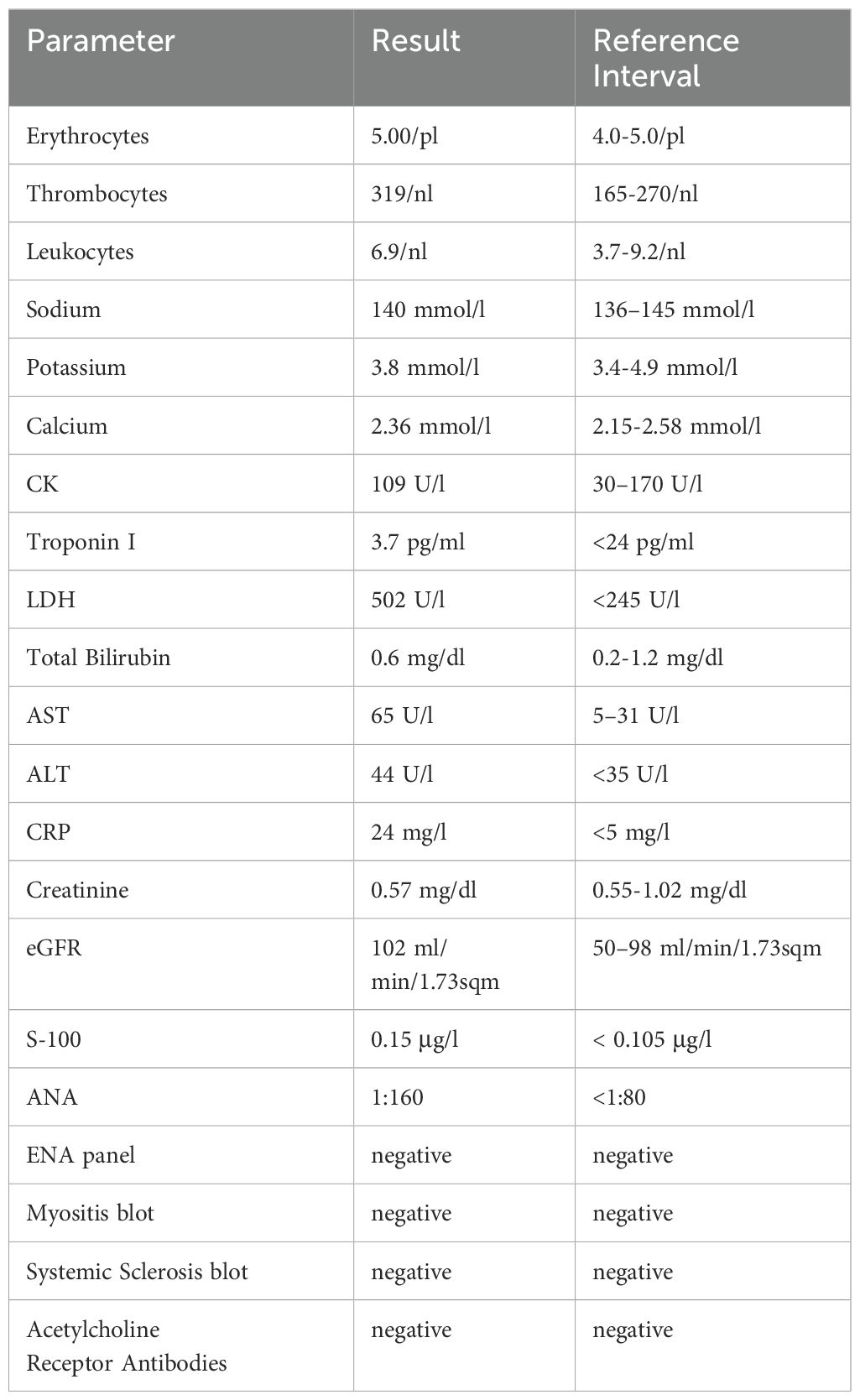
Routine labs looked deceptively reassuring: CK levels never rose above normal. However, a closer look revealed:
-
MRI: Bright (hyperintense) signals in spinal and gluteal muscles, suggesting inflammation.
-
Electromyography (EMG): Abnormal short-duration, low-amplitude signals consistent with muscle fiber injury.
-
Normal troponin and absence of acetylcholine receptor antibodies ruled out myocarditis and myasthenia gravis.
-
Autoantibody panels were largely negative, consistent with seronegative ICI-induced myositis.
This was ICI-induced myositis without CK elevation—a presentation so rare it is barely described in the literature.
Management and Recovery
High-dose intravenous prednisolone for three days, followed by an eight-week taper, produced a steady improvement. Within three months, she had regained full muscle strength, walking without difficulty. Six months later, she remained symptom-free, with no relapse.
Why This Case Matters
-
Breaking the “CK Rule”: CK is a valuable marker for muscle injury—but its absence does not rule out myositis. This case proves that normal CK can mask serious ICI-related muscle inflammation.
-
Delayed Onset: Symptoms emerged two months after stopping immunotherapy, highlighting that irAEs can strike well beyond active treatment.
-
Multimodal Diagnosis is Key: In atypical cases, clinical exam, MRI, and EMG become essential for diagnosis, especially when biomarkers fail.
-
Steroid Responsiveness: Early recognition and immunosuppression can reverse symptoms and prevent long-term disability.
You can read the full abstract here


