At OncoDaily Immuno-Oncology, we spotlight this week’s defining conversations — from cabozantinib + atezolizumab data in endocrine tumors and the upcoming CONDOR symposium on sarcoma IO, to radiotherapy–immune crosstalk at Immunorad and NICE’s durvalumab approval in SCLC. Add in fresh insights on CAR T-cell persistence and CheckMate 214 in RCC, and you have the science, strategy, and voices shaping the next era of cancer immunotherapy.
This Week’s Expert Highlights in Immuno-Oncology
Enrique Grande (Head of Oncology at MD Anderson Cancer Center Madrid):
” New evidence in aggressive and refractory endocrine tumors.
The combination of cabozantinib + atezolizumab shows a promising safety and response profile in adrenocortical carcinoma (ACC) and anaplastic thyroid cancer (ATC), with response durations over one year.
Phase II multicenter study (CABATEN/GETNE-T1914) including 93 patients across 6 cohorts. Exploring the synergy between immune checkpoint inhibitors and multikinase inhibitors.”

Italiano Antoine (Head of Precision Medicine at Gustave Roussy):
” Join us for the 3rd CONDOR Symposium — Microenvironment and Immunotherapy of Sarcomas
- 25–26 September 2025
- Domaine Haut-Carré, Talence (Bordeaux area), France
- On-site only, in English
This edition brings together clinicians, translational scientists, and industry leaders to dive deep into the sarcoma tumor microenvironment and immuno-oncology. Expect high-level science, practical exchanges, and plenty of networking.
- Registration deadline extended to 15 September 2025
- Register now
If sarcoma, immunotherapy, or tumor microenvironment is your world, you should be in the room. Please share with colleagues who shouldn’t miss it!”
James Good (Clinical Director of Stereotactic Radiotherapy at GenesisCare):
“First morning at Immunorad in Paris: the immune effects of hashtag#radiotherapy are central to clinical outcomes. Lunch was pretty good, too…
This is a great meeting that explores the ever-evolving interplay between local radiation therapy and the systemic immune context within which cancer arises. I first attended nearly a decade ago, along with Crispin Hiley and Kevin Harrington, two longstanding friends as well as colleagues committed to advancing radiation oncology. It’s great to be back in Paris with them again.
Ralph Weichselbaum, a father-of-the-field and regular feature at the meeting, gave a characteristically detailed keynote on his group’s work. His editorial (‘The Dark Side of Radiotherapy’) had caused some controversy on X recently but that doesn’t undermine the quality of the science, the clinical implication being we should strive to deliver ablative doses to all metastases, given that sub-ablative doses may induce a secretome conducive to systemic disease progression. Crispin pointed out that radiation to the primary site has been shown to improve outcomes in prostate cancer, nasopharyngeal cancer and others, highlighting that translatability will vary between cancer types.
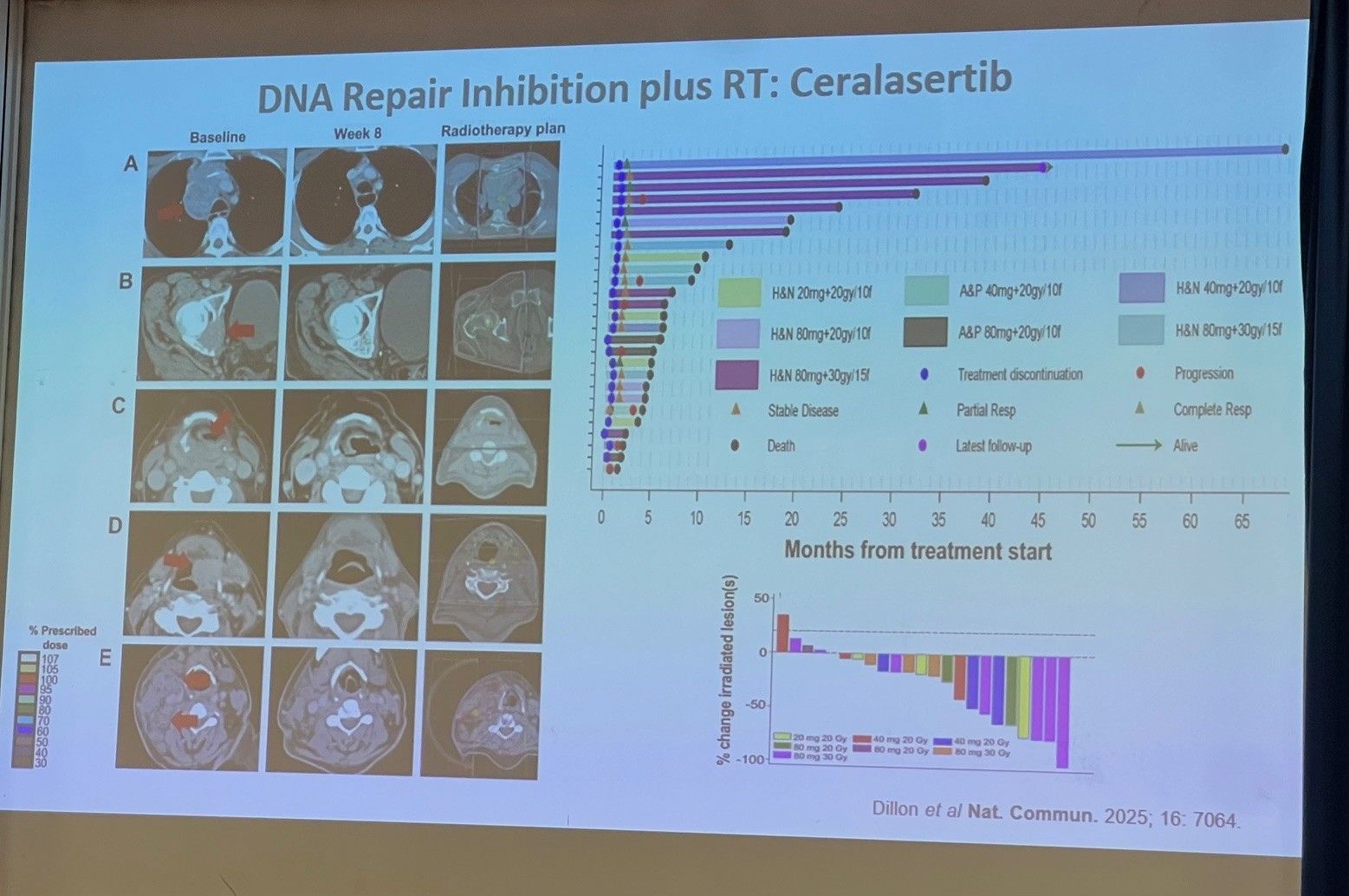
With his usual clarity and aplomb, Kevin then presented his group’s work on the clinical and immunological effects of combining DDR manipulation with palliative radiotherapy — several patients in a trial run by Magnus Dillon achieving long term disease remission — as well as the radiosensitisation potential of novel nanoparticles under development by Kamyar Farahi at Johnson and Johnson.
The two talks together provoked the following thoughts:
- The patient’s systemic immune context is probably of equal or greater importance than the tumour micro-environment in determining the outcome of local therapies such as RT
- Technological innovation, such as the hashtag MRI-guided radiotherapy programme we have developed at GenesisCare UK, offers greater flexibility in delivering ablative doses to multiple and/or anatomically challenging targets, as investigated by David Palma and others in the SABR COMET-10 and ARREST studies
- Biologically-driven innovation, such as combining novel agents with sub-ablative doses, may expand the role of radiation in managing polymetastatic disease and cancer that threatens the physiologic capacity of a particular organ, such as HCC/liver-only metastatic disease, leptomeningeal disease, etc.
- Intra-tumoral therapy may be a useful adjunct to conventionally fractionated and hypofractionated radiation with further interesting systemic effects if they potentiate immunogenic cell death, but heterogenous distribution within the tumour may limit efficacy. I see this frequently when offering patients salvage hashtag SBRT after incomplete responses to intra-arterial therapies for hashtag HCC.
As for the afternoon session… I’m afraid I have no idea, because I was still digesting the eclair”
Marco Donia (Associate professor at OUH Odense University Hospital, shared Lina Hua Bisgaard’s post):
“Kudos to Lina Hua Bisgaard for the brilliant results obtained, and congratulations for the PhD position in the prestigious lab of Tanja de Gruijl!
Honoured for the opportunity to supervise Lina for the past year, and witness her incredible growth”
Quoting Lina Hua Bisgaard’s, MSc. Student in Immunology and Inflammation at University of Copenhagen
“Last week, I successfully defended my Master’s thesis titled: “Tissue-Specific Features of Tumor-Infiltrating Lymphocytes.”
This project was conducted in the TIL group at CCIT-DK – National Center for Cancer Immune Therapy of Denmark. I am incredibly grateful to my supervisors, Marco Donia and Mario Presti, for their invaluable support and guidance throughout my Master’s thesis project.
A heartfelt thank you as well to the entire team at CCIT-DK – National Center for Cancer Immune Therapy of Denmark for their support and collaboration throughout this journey. I would also like to thank Kræftens Bekæmpelse (Danish Cancer Society) for the scholarship supporting this project.
This defense marked the official completion of my Master’s degree in Immunology and Inflammation from the Københavns Universitet – University of Copenhagen. It has been an incredible journey of learning, collaboration, and scientific growth.
New Chapter
I’m excited to share that I will be starting a PhD at Amsterdam UMC, under the supervision of Tanja de Gruijl, as part of the Marie Skłodowska-Curie T-RAFIC – Tracking and controlling therapeutic immune cells in cancer. This opportunity marks the beginning of an exciting new chapter where I’ll continue advancing my work in immune-oncology, grow both professionally and personally, and gain valuable experience living abroad in Amsterdam.
As I prepare for the move to Amsterdam, I would greatly appreciate any advice, housing leads, or local connections. Please feel free to reach out – I’d love to connect! ”
“Progress in lung cancer treatment
NICE (England & Wales) has recommended durvalumab (Imfinzi) as the first immunotherapy for people with limited-stage small-cell lung cancer whose disease has not progressed after chemoradiotherapy.
For a cancer where treatment options have remained largely unchanged for decades, this represents an important step forward.
It also highlights a wider issue: the need for timely and equitable access to innovation across Europe.”
Arndt Vogel (Head of the Center for Personalized Medicine, MHH at Medical University of Hanover):
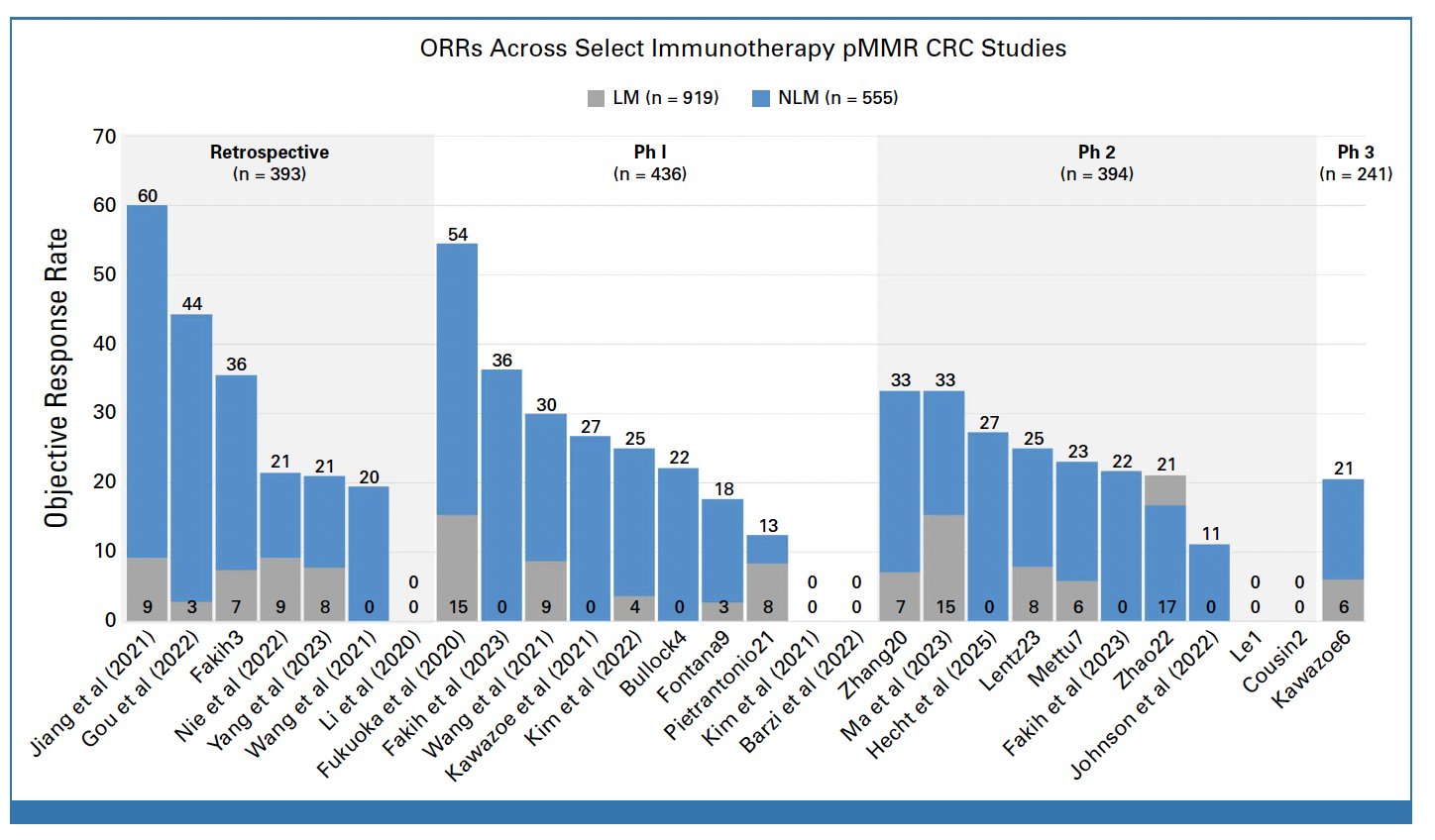
” Immunotherapy Efficacy in MSS CRC Patients With and Without Liver Metastases
- consistent higher benefit for ICI in NLM CRC
- After “sidedness” another clinical biomarker in CRC
- We need prospective data..”
Raffaele Di Giacomo (Director predictive AI at ByronInsight AG):
” Monoclonal antibodies are redefining immunotherapy—faster delivery, broader impact, and fresh approvals landing now. From oncology to RSV prevention, the curve is bending toward real-world gains.
Since 2011, IO mAbs have driven >150 FDA approvals—17 in 2024 alone. And a subcutaneous Keytruda could cut chair time to 2 minutes, a major access win.
Beyond cancer, nirsevimab shows strong real-world protection in infants, while new mAb combos (e.g., Vectibix + KRAS inhibitor) expand precision options.
Clinicians: prep for site-of-care shifts and companion testing. Payers: model budgets for earlier-line use. Patients: convenience and durability are improving.
Are we ready for the operational and equity ripple effects of making powerful mAbs both broader and faster to deliver?”
John Gordon (Co-Founder, Director, VP Scientific Affairs at Celentyx Ltd):
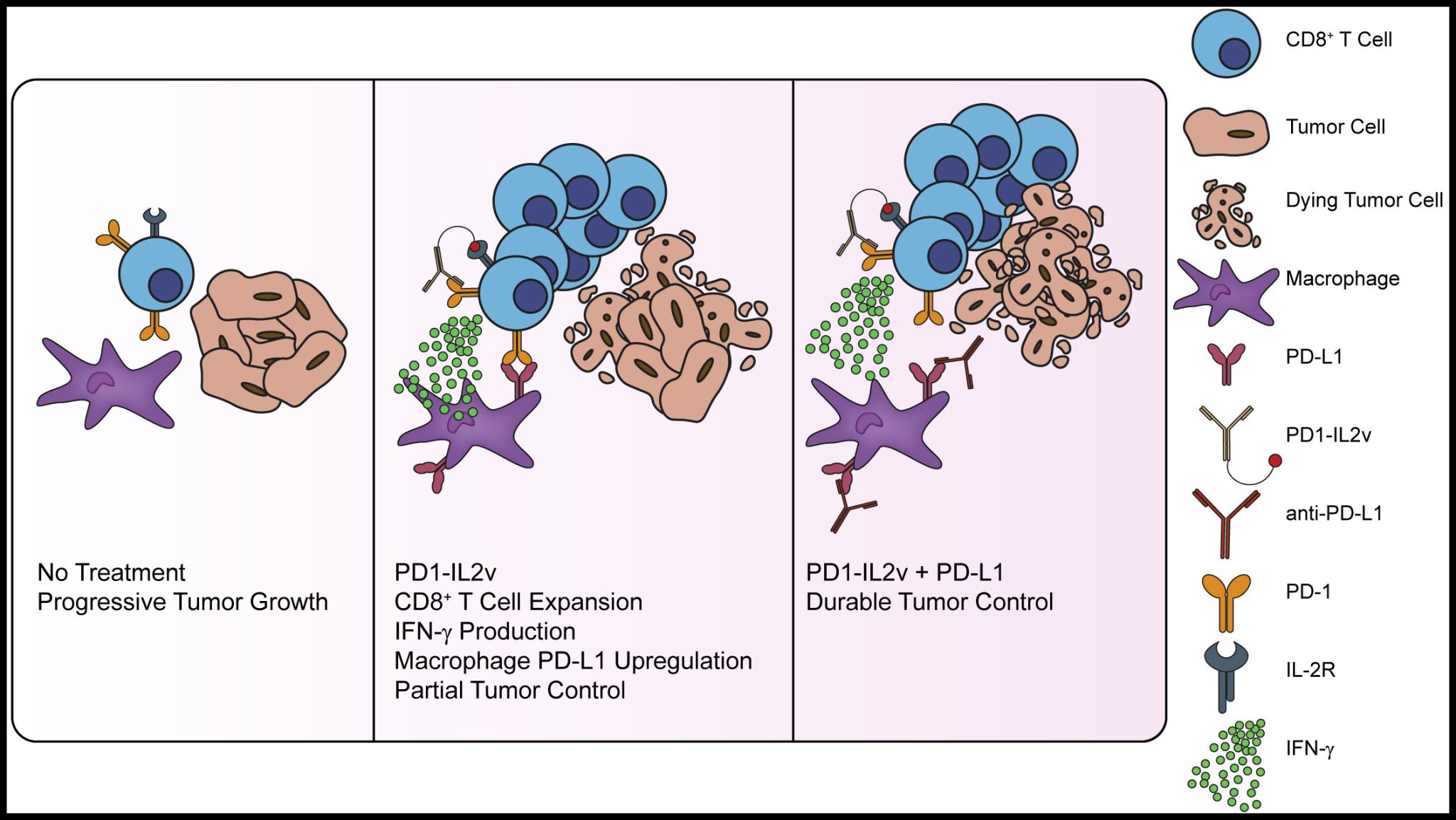
“”Immunotherapy PD1–targeted cis-delivery of an IL2 Variant induces a multifaceted anti-Tumoral Tcells response in Human Lung Cancer | Study from Alfred ZIppelius and Co. now breaking at Science Magazine TM
Interleukin-2 (IL-2) is a cytokine that affects various immune cell populations and has been evaluated as an immunotherapy treatment but is associated with clinical toxicities. Efforts have been made to improve IL-2 treatment by creating antibody drug conjugates, such as PD1-IL2v, that improve cytotoxic and proliferative functions of stem-like precursor exhausted CD8+ T cells.
Here*, Fusi et al. show that PD1-IL2v affects globally exhausted T cells by activating and increasing the number of terminal effector T cells and acting on CD4 T cells. They provide a mechanistic evaluation of the effect of PD1-IL2v on human T cell activity, supporting the further clinical development of next-generation immunocytokines for cancer treatment.
FIGURE | Taken from Brendan Horton and Stefani Spranger | Combined PD1-IL2v and anti-PD-L1 mediate durable tumor control PD1-IL2v induces robust CD8+ T cell expansion in the TME, but CD8+ T cell production of IFN-γ drives macrophage PD-L1 expression that blunts tumor control. The addition of an anti-PD-L1 antibody to PD1-IL2v counteracts PD-L1 upregulation to bring about durable tumor control. A Preview article on Mélanie Tichet et al: Bispecific PD1-IL2v and anti-PD-L1 break tumor immunity resistance by enhancing stem-like tumor-reactive CD8+ T cells and reprogramming macrophages ”
Jeremy Grenier (Attending Physician, Cancer Center at Children’s Hospital of Philadelphia):
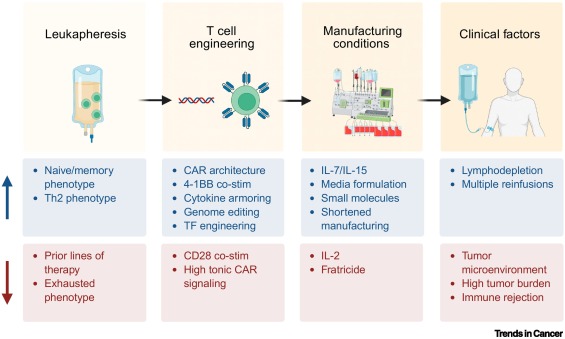
“Persistence of CAR T cells is critical for the success of this revolutionary therapy in patients with cancer, begging the question: What makes a CAR T cell persist after infusion? In our latest review published in Trends in Cancer, Katherine Mueller, Evan Weber, and I attempt to answer this question by exploring the complex world of CAR T cell persistence.
We start by reviewing clinical observations of how CAR T persistence impacts outcomes in liquid and solid malignancies. We then delve into the biological mechanisms thought to support long-term CAR T responses by highlighting insights from recent correlative multiomics datasets from CAR T-treated patients. Next, we discuss next-generation engineering approaches to enhance CAR T longevity, including CAR design, manufacturing conditions, and cell fate reprogramming.
We conclude our discussion by proposing a new conceptual framework that distinguishes persistence in the setting of active tumor clearance vs. long-term immune surveillance. We believe this framework enables us to distinguish mechanisms of persistence which may be relevant at different time points of therapy and provides a template for fine-tuned engineering strategies to address individual barriers to persistence.
Despite tremendous progress in the field, consistent CAR T persistence for all patients remains elusive. Our hope is that by mapping out the current knowledge gaps and highlighting promising research directions, we can accelerate the path toward more reliable treatments that provide lasting benefit for patients.”
You Can Read The Full Article Here
Arun Shahi (Assistant Professor and Senior Consultant of Medical Oncology at Patan Hospital):
“Honored to have delivered a Talk at the Best of ASCO 2025 (Officially Licensed), organized by the Medical Oncology Society in Bangladesh (MOSB) on 18th September 2025.
I had the privilege to present the final analysis of the landmark CheckMate 214 trial:
- Nivolumab + Ipilimumab vs Sunitinib in first-line treatment of advanced renal cell carcinoma.
This trial has been practice-changing, establishing the role of dual immunotherapy in improving survival and long-term outcomes for patients with advanced RCC.
My sincere thanks to MOSB and the organizing committee for this opportunity, and to colleagues and friends for the engaging academic discussions. Always a pleasure to connect, learn, and share knowledge across borders.”



