The final week of October 2025 delivered major updates in GI Oncology, spanning immunotherapy, hepatobiliary surgery, genomics, epidemiology, and patient safety. From the NCCN colon cancer guideline updatemandating DPYD testing to groundbreaking results in NICHE2 + FOXTROT, MSI-H colorectal cancer, and robotic cholangiocarcinoma surgery, global experts continue to redefine standards of care.
New publications in ESMO Open, Gastroenterology, and npj Precision Oncology unveiled advances in HCC genomics, synthetic-lethal targets in PDAC, and early-onset cancer trends, while translational research in CLDN18.2 CAR-T toxicity offered critical insights for next-generation therapies.
This week’s highlights reflect the convergence of precision medicine, surgical innovation, and evidence-based prevention, marking another step toward more personalized, data-driven GI cancer care.
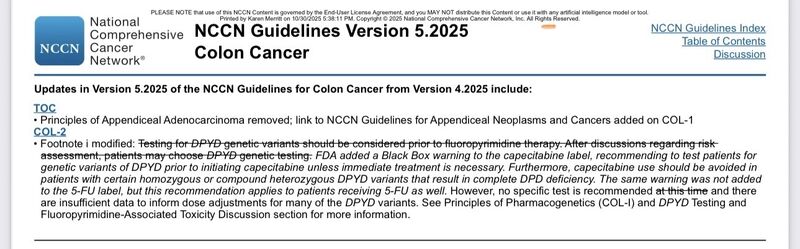
Karen Merritt – Patient Advocate for Universal DPD/DPYD Testing
“NCCN updated Colon cancer guidelines today, 10/30/2025!
FDA says test. NCCN says test .
Now every cancer center must implement testing.
Protect patients. Test DPYD before chemo.”
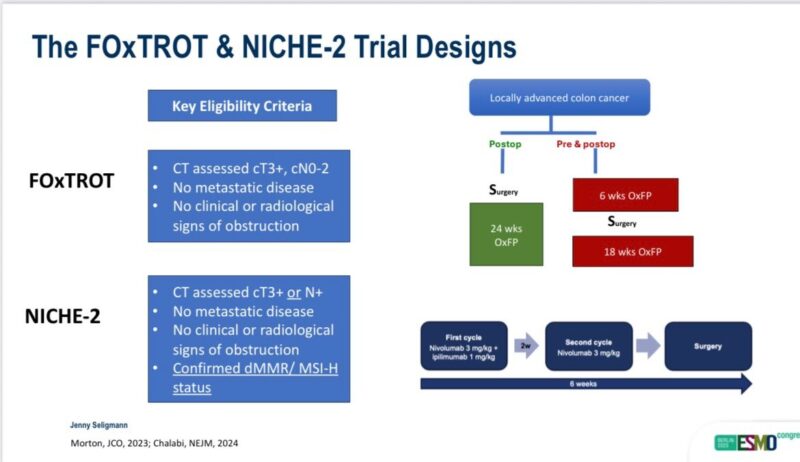
Jenny Seligmann, MD – Professor of Gastrointestinal Oncology, University of Leeds
“Proud to present combined NICHE2 + FOXTROT analysis at ESMO25
In summary
IO superior to chemo (pre or post surgery)
Little role of chemo in dMMR CC (!ATOMIC)
CT staging identified high risk pt
20% recurrence in “good prognosis” pts relevant with effective rx!
Further data to support neoadjuvant IO for routine use! ESP for T4 pts
Privilege to work with super NKI team”
Joep IJspeert, MD, PhD – Gastroenterologist, Antoni van Leeuwenhoek, Amsterdam
“Excited to share our latest study in Endoscopy Journal:
Individuals with polyps ≥10mm without other high-risk features have a similarly low post-colonoscopy colorectal cancer risk as those with no polyps.Our findings suggest that individuals with ≥10mm polyps as their sole high-risk feature have a comparable 5-year risk of post-colonoscopy colorectal cancer to those without polyps — challenging the need for strict 3-year surveillance intervals. Lengthening surveillance intervals would affect 46% of high-risk individuals if limited to those with 10-20mm polyps without other high-risk features.
This work, led by Nanette van Roermund (first author), is a collaboration between Antoni van Leeuwenhoek, Amsterdam UMC, and Erasmus MC.
A great step toward more personalized and sustainable colonoscopy surveillance!”
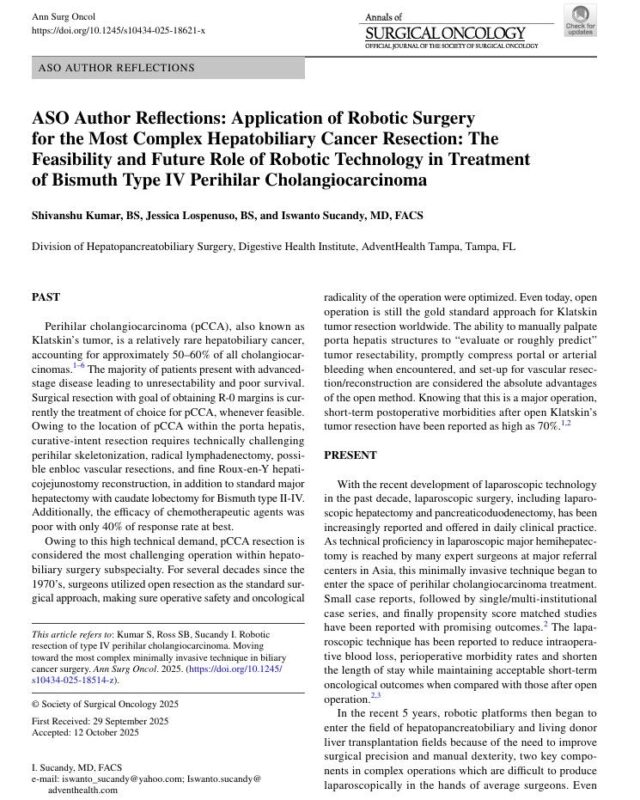
Iswanto Sucandy, MD, FACS – Professor of Surgery, Hepatopancreatobiliary, Robotic, and Gastrointestinal Surgery, AdventHealth, Tampa
“Sharing our recent contribution on the development of robotic surgery technique for Type IV perihilar cholangiocarcinoma. This is the most complex hepatobiliary resection undertaken via robotic surgery at this time. Refer to our paper on the Annals of Surgical Oncology with link to download technical video below.
We continue to work on this difficult disease treatment from our Hepatobiliary Center in Tampa Florida. We are also excited to continue to collaborate with our esteemed colleagues from around the World comparing short and hopefully soon long-term outcomes of minimally invasive robotic and open Klatskin bile duct cancer surgery.”
Matthias W., PhD – Group Leader, Universitätsmedizin Göttingen
“Proud to share our latest publication in Gastroenterology:
“Targeting Mutual Dependence of PI3K α/δ and SUMO Signaling in Pancreatic Cancer.” Congratulations to first author Hazal Köse and special thanks to Günter Schneider and Ulrich Keller for their great collaboration.The study reveals a synthetic-lethal interaction between these pathways, offering a new therapeutic strategy for PDAC.”
Axelle Braggion, MD – PhD Student in Cancer Epidemiology
“More early-onset pancreatic cancers, but no higher risk ?
Check out our Matters Arising just published in npj Precision Oncology, in which we discuss:
The role of population growth and ageing
Caveats with prevalence measures
Burden vs risk — different public health implications
“The rise in early-onset cancers, including pancreatic cancer, has attracted major attention from the media, clinicians, and researchers. This growing cancer burden is largely driven by population growth and ageing rather than by an increase in risk, estimated by age-adjusted incidence. Distinguishing between cancer burden and risk is essential to avoid misinterpretation and unwarranted alarm, as each carries distinct implications for public health interventions.””
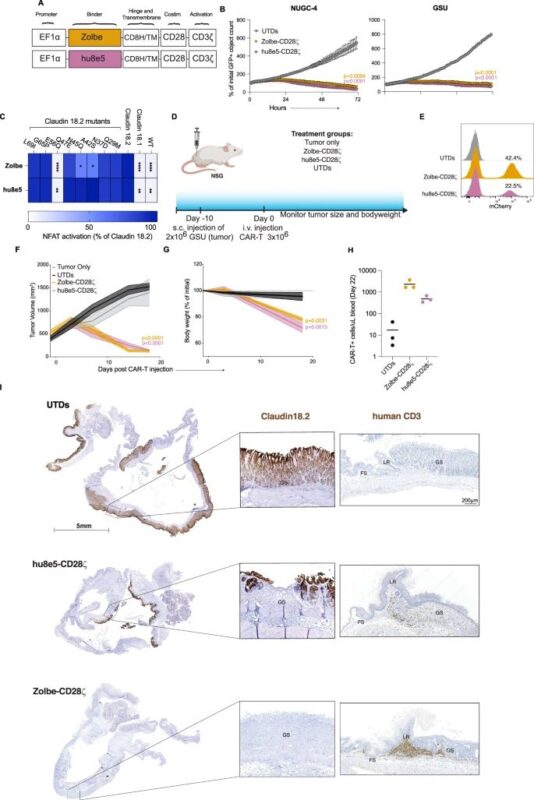
Hung Trinh, PhD – Managing Director, Cell & Gene Therapy, Oncology, Vaccine, CMC/MFG
“On-target off-tumor toxicity of claudin18.2-directed CAR-T cells in preclinical models
Claudin 18.2 (CLDN18.2)-targeted CAR-T cell therapies have shown promising clinical efficacy in gastric cancer. However, early-phase trials have reported gastrointestinal adverse events due to on-target off-tumor recognition of CLDN18.2 in the gastric mucosa. By leveraging shared CLDN18.2 epitopes and expression in humans and mice, we establish an in vivo model that replicates the on-target off-tumor toxicity of CLDN18.2 CAR-T.
Our findings confirm that this toxicity is independent of the CAR construct’s design, co-stimulatory domain, and tumor model. Additionally, we demonstrate the utility of this model in testing strategies to mitigate on-target toxicity, such as Boolean-logic AND-gate approaches.
Our results offer insights into the use of mouse models that recapitulate on-target off-tumor toxicities, with the caveat that although we are often concerned that models will undercall toxicities in humans, they may also overcall the incidence and severity of toxicities, prematurely discarding promising therapeutic agents from further clinical development.”
Hannes Jansson, MD, PhD – Attending Surgeon, Division of HPB Surgery, Karolinska University Hospital
“Very proud to be able to continue our collaboration with Cancer Institute Hospital of the Japanese Foundation for Cancer Research after my fellowship
Our bi-institutional experience in surgical resection for biliary tract cancer recurrence, now in pre-print at European Journal of Surgical Oncology Karolinska Universitetssjukhuset
Re-resection (9% of patients with recurrence) an independent prognostic factor, together with time to recurrence >12 months, CA19-9 <500, less advanced disease at primary diagnosis. Systemic therapy used as a test of time in oncological high-risk setting (e.g. early recurrence, advanced primary disease, higher CA19-9)
Best prognosis after re-resection for recurrent CCA confined to the liver. Gallbladder cancer recurrence no survival benefit with re-resection.
Careful selection for re-resection as part of the multimodal treatment in recurrent BTC”
Andrea Casadei Gardini, MD, PhD – Associate Professor, Università Vita-Salute San Raffaele
“New insights into the genomic landscape of advanced HCC!
Our latest work, now out in ESMO Open, provides one of the largest real-world analyses of comprehensive genomic profiling in advanced hepatocellular carcinoma (HCC), leveraging the Flatiron Health–Foundation Medicine clinico-genomic database.
370 patients with advanced HCC who received systemic therapy were analyzed.
The most frequent alterations were TERT promoter (61.5%), CTNNB1 (34%), and TP53 (33%), highlighting key pathways involved in cell
cycle/apoptosis, DNA damage control, WNT, and p53.
Viral-related HCC was significantly associated with TERTp and CTNNB1 alterations, whereas non-viral forms more frequently showed RTK/RAS pathway involvement.”
Yan Leyfman, MD – Physician | Director & Host, MedNews Week
“Microsatellite instability-high (MSI-H) colon cancer shows strong responsiveness to immune checkpoint inhibition—but the best strategy for patients with isolated peritoneal metastases (iPM) remains unclear.
Using national real-world data, this study found that:
Immunotherapy significantly improved survival vs chemotherapy (median OS: 33 vs 18 mo)
Surgery + immunotherapy offered the greatest survival benefit
Findings challenge the notion that surgery should be avoided in metastatic disease
These results support a multimodal approach integrating immunotherapy and surgical resection for this biologically distinct, clinically challenging subgroup—and underscore the need for prospective trials to define optimal sequencing.”

You can also read about 10 Must-Read Posts in GI Oncology from the first week of Oncober on OncoDaily.


