The ESMO Congress 2025, held in Berlin from October 17–21, will be a key event in oncology this year. It will gather global cancer experts to discuss the latest advances, especially in immunotherapy.
Highlights include updates on new immunotherapy agents, personalized vaccines, bispecific antibodies, and biomarkers across lung, melanoma, and head and neck cancers. Experts will also address managing side effects, cardiovascular risks, and improving treatment delivery with options like subcutaneous injections.
Importantly, sessions will explore not only the effectiveness of immunotherapy but also its accessibility, safety, and long-term sustainability in everyday cancer care.
In the following sections, we preview key immunotherapy abstracts and sessions scheduled for October 17–21, focusing on the science, strategies, and clinical insights poised to shape the next chapter of cancer care.

Investigational Immunotherapy – Mini Oral Session
Date/Time: Friday, 17 October 2025
Room: Nuremberg Auditorium – Hall 5.2
Chair: Daniela S. Thommen (Amsterdam, Netherlands)
This mini-oral session will spotlight the next generation of investigational immunotherapies, highlighting novel mechanisms, innovative combinations, and first-in-human experiences across solid tumors and melanoma.
Key Abstracts and Presentations
- mRNA-4359 Plus Pembrolizumab in CPI-Resistant/Refractory Melanoma
Speaker: David J. Pinato (London, UK)
Early outcomes and PD-L1 expression analyses from this trial explore whether mRNA-based immunotherapy can restore responsiveness in checkpoint-resistant melanoma. - EVX-01 Personalized Cancer Vaccine in Advanced Melanoma (2-Year Follow-Up)
Speaker: Muhammad A. Khattak (Perth, Australia)
A personalized vaccine strategy demonstrates durable T-cell responses and disease control, underscoring the promise of individualized immunotherapy. - Botensilimab + Balstilimab in Advanced Solid Tumors
Speaker: Michael Gordon (Scottsdale, USA)
Phase 1b data reveal emerging survival plateaus across tumor types, suggesting durable benefit from this dual-checkpoint approach.
- ReCIPE-M1 Study: Plasma Exchange in Melanoma
Speaker: Jacob Orme (Rochester, USA)
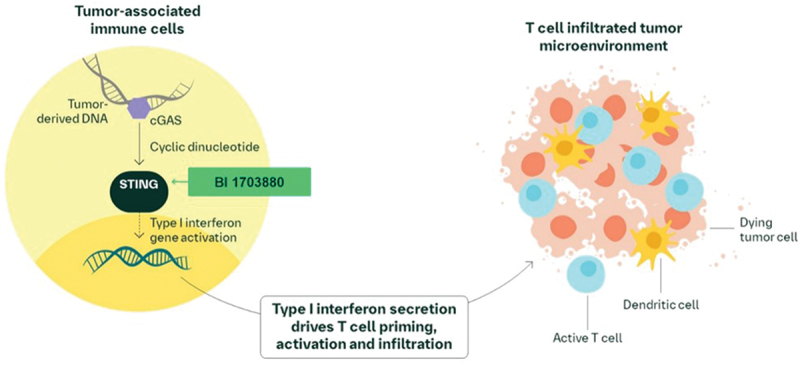
Investigates whether plasma exchange can overcome resistance to immunotherapy and rescue anti-tumor immune responses. - STING Agonist BI 1703880 + Ezabenlimab
Speaker: Eileen E. Parkes (Oxford, UK)
This first-in-human Phase Ia study (NCT05471856) explored the combination of BI 1703880, a novel STING (STimulator of INterferon Genes) agonist, with ezabenlimab, an anti–PD-1 antibody, in patients with advanced solid tumors. The rationale stems from preclinical evidence showing that STING activation enhances antigen presentation and induces type I interferon responses, potentially increasing PD-L1 expression and tumor immunogenicity.The trial employed an innovative lead-in design, where all patients initially received monotherapy with BI 1703880 during Cycle 1, followed by combination therapy with ezabenlimab starting in Cycle 2. This approach allowed investigators to assess the individual contribution and tolerability of BI 1703880 before evaluating the full combination.The primary objective was to identify dose-limiting toxicities (DLTs) and determine the maximum tolerated dose (MTD). Secondary endpoints included safety, pharmacokinetics, and exploratory biomarkers of immune activation.Preliminary findings presented by Dr. Parkes highlighted that the combination was generally well tolerated, with manageable immune-related adverse events and promising early signals of immune activation. Notably, evidence of upregulated interferon-stimulated genes, increased tumor HLA expression, and tumor-infiltrating lymphocyte recruitment were observed, supporting the proposed synergistic mechanism.
- STA551 Anti-CD137 Switch Antibody
Speaker: Diogo Silva (Portugal)
First-in-human data of a novel switch antibody, tested alone and with atezolizumab, showcase potential to selectively boost T-cell costimulation. - Solnerstotug (Anti-VISTA) + Cemiplimab
Speaker: Kyriakos P. Papadopoulos (San Antonio, USA)
Phase 1 expansion cohort results in patients resistant to prior PD-(L)1 therapy evaluate whether targeting VISTA restores immune responsiveness.
- INCA33890 (PD-1/TGFβR2 Bispecific Antibody)
Speaker: Elena Garralda (Barcelona, Spain)
INCA33890 is a novel bispecific Biclonics® antibody designed to simultaneously inhibit PD-1 and TGFβR2 signaling—two key immunosuppressive pathways implicated in tumor immune evasion. By targeting both pathways, INCA33890 aims to overcome immune exclusion and resistance to checkpoint inhibitors, especially in TGFβ-rich solid tumors.This agent was engineered with a PD-1–directed binding arm exhibiting >10-fold higher affinity than its TGFβR2 arm, enabling cell-selective blockade of TGFβ signaling in PD-1–expressing immune cells while sparing healthy tissue. Preclinical assays confirmed that INCA33890 effectively inhibits TGFβ1-induced pSMAD activation only in PD-1+ cells, and demonstrates PD-1 signaling inhibition comparable in potency to pembrolizumab in reporter assays.In functional immune assays, INCA33890 restored cytokine production in exhausted human T cells and induced IFNγ secretion in ex vivo treated ovarian ascites samples—where pembrolizumab alone showed no activity. Additionally, in humanized NSG mouse models, INCA33890 showed superior tumor growth inhibition against MDA-MB-231 and A375 xenografts compared to monotherapy PD-1 or TGFβR2 blockade.Pharmacokinetic and safety data from non-human primates (NHPs) indicated that INCA33890 was well tolerated, with no evidence of systemic toxicity linked to TGFβ pathway interference. - LBA55 START-001: Invikafusp Alfa
Speaker: Elena Garralda (Barcelona, Spain)
Early Phase 2 data for a first-in-class TCR β-chain-targeted bispecific antibody in antigen-rich, ICB-resistant solid tumors.
Why It Matters: This session captures the breadth of innovation in immuno-oncology: from mRNA vaccines and bispecific antibodies to novel costimulatory pathways and plasma exchange strategies. Together, these presentations highlight how investigators are working to overcome checkpoint resistance, deepen responses, and extend the reach of immunotherapy to more patients.
Special Symposium – Refining Strategies to Boost Immunotherapeutic Effectiveness in HNSCC
Date/Time: Friday, 17 October 2025
Room: Bremen Auditorium – Hall 6.2
Chair: Irene Braña (Barcelona, Spain)
This dedicated symposium will explore innovative strategies aimed at enhancing immunotherapy responses in head and neck squamous cell carcinoma (HNSCC), a disease where checkpoint inhibitors have transformed treatment but remain limited by resistance and heterogeneous benefit.
Key Presentations
- Patient-Derived Tumor Organoids for Guiding Treatment Decisions in Locally Advanced HNSCC
Speaker: Ingeborg Tinhofer-Keilholz (Berlin, Germany)
Highlights the use of organoid models as predictive tools to personalize immunotherapy approaches, bridging translational research and clinical application. - The Rationale Behind Drug Combinations
Speaker: Makoto Tahara (Kashiwa, Japan)
Discusses how combining immunotherapy with targeted or cytotoxic drugs may overcome resistance mechanisms and enhance anti-tumor efficacy. - The Rationale Behind Combining Drug and Radiation
Explores the synergistic potential of radiotherapy with immunotherapy, leveraging radiation-induced immune priming to improve systemic tumor control. - Combinations of Cell Death Modulators and Other Therapies
Speaker: Kevin J. Harrington (Sutton, UK)
Reviews strategies integrating immunotherapy with agents that modulate cell death pathways, aiming to potentiate immune-mediated tumor clearance. - Q&A and Discussion
An interactive discussion session for synthesis of key points, debate on clinical translation, and audience engagement with experts.
Why It Matters: HNSCC remains a major therapeutic challenge, with limited survival gains from current checkpoint inhibitors. This symposium emphasizes translational approaches—from organoids to novel combination regimens—that aim to unlock broader and more durable immunotherapy benefits. It provides a forward-looking perspective on how rational strategies may shape the next generation of head and neck cancer treatment.
Systemic Anti-Tumour Immunity in Clinical Outcomes
Date/Time: Friday, 17 October 2025
Room: Karlsruhe Auditorium – Hall 5.2
Chair: Benjamin P. Fairfax (Oxford, United Kingdom)
This educational session will highlight how systemic immune mechanisms shape cancer treatment outcomes, with a focus on state-of-the-art tools for profiling and monitoring immune responses in patients receiving immunotherapy.
- High-dimensional peripheral immune profiling – Adrian Hayday (London, UK)
Will explore advanced profiling methods capable of capturing the complexity of circulating immune cells. Such approaches can provide biomarkers for predicting response, toxicity, and long-term benefit from immunotherapies.
- Methylation profiling of peripheral immune cells – Daniel De Carvalho (Toronto, Canada)
Will discuss how epigenetic signatures, particularly DNA methylation patterns, in immune cells may serve as stable and predictive markers of treatment sensitivity and resistance, offering a new dimension to biomarker development.
- Immuno-imaging for immunotherapy – Inge Marie Svane (Herlev, Denmark)
Will present cutting-edge imaging technologies that allow real-time visualization of immune activity and distribution, enabling more precise monitoring of treatment dynamics and paving the way for personalized dosing strategies.
Why It Matters: This session underscores the critical role of systemic immunity in determining whether patients benefit from immunotherapy. By integrating high-dimensional profiling, epigenetic mapping, and advanced imaging, oncologists may soon have powerful tools to refine patient selection, predict outcomes, and guide adaptive treatment strategies.
Special Symposium – Immunotherapy of NSCLC Where Are We
Date/Time: Saturday, 18 October 2025
Room: Munich Auditorium – CityCube B
Chairs: Laura Mezquita (Barcelona, Spain) & Roberto Ferrara (Milan, Italy)
This symposium will address the evolving role of immunotherapy in non-small cell lung cancer (NSCLC), with a focus on refining patient selection, rethinking treatment strategies, and exploring innovative approaches to extend benefit.
Key Presentations
- Optimizing Patients’ Selection for Immunotherapy
Speaker: Solange Peters (Lausanne, Switzerland)
Covers biomarker-driven selection strategies and clinical criteria guiding which patients are most likely to respond to checkpoint inhibitors. - Who Should Not Receive Immunotherapy Today?
Speaker: Joachim G. Aerts (Rotterdam, Netherlands)Examines subgroups where immunotherapy has limited benefit or may be harmful, providing practical insights for treatment exclusion criteria. - Immunotherapy Rethinking Duration and Dose
Speaker: Benjamin Besse (Villejuif, France)
Discusses emerging evidence on optimal treatment duration, dosing adjustments, and how to balance efficacy with long-term toxicity and cost. - Innovative Immune Strategies for Advanced NSCLC
Speaker: Laura Mezquita (Barcelona, Spain)
Presents cutting-edge approaches including novel checkpoint targets, bispecific antibodies, and rational combination regimens for advanced disease. - Q&A and Discussion
Interactive panel with the audience, synthesizing the presented strategies and debating the future direction of NSCLC immunotherapy.
Why It Matters: Checkpoint inhibitors have transformed NSCLC treatment, yet challenges remain in defining who benefits, how long therapy should continue, and what innovative strategies can further improve outcomes. This session will provide a comprehensive update, bridging clinical practice with ongoing research directions, and helping shape the next stage of immunotherapy in lung cancer.
Educational Session – IO Biomarkers in 2025
Date/Time: Saturday, 18 October 2025
Room: Cologne Auditorium – CityCube A
Chairs: Maria Libera Ascierto (Glasgow, United Kingdom) & Jon Zugazagoitia (Madrid, Spain)
This educational session will explore the rapidly evolving landscape of biomarkers in immuno-oncology (IO), showcasing technologies that aim to refine patient selection, predict therapeutic sensitivity, and guide next-generation treatment strategies.
Key Presentations
- Quantitative Spatial Analysis
Speaker: Kurt Schalper (New Haven, USA)
Focuses on spatial mapping of immune and tumor cells within the tumor microenvironment, highlighting how spatial metrics can guide biomarker-driven therapy. - Transcriptomics
Speaker: Maria Libera Ascierto (Glasgow, UK)
Discusses transcriptome-based approaches to characterize tumor–immune interactions and identify predictive gene expression signatures for IO response. - Radiomics & ImmunoPET
Speaker: Laurent Dercle (New York, USA)
Presents cutting-edge imaging techniques, including radiomics and ImmunoPET, as non-invasive tools for monitoring immune activity and treatment response in real time. - Multidimensional Predictors of IO Sensitivity
Speaker: Aurélien Marabelle (Villejuif, France)
Integrates genomic, transcriptomic, epigenetic, and clinical data to develop multidimensional models predicting immunotherapy sensitivity across cancers. - Q&A and Discussion
An interactive discussion to synthesize insights from molecular, spatial, and imaging biomarkers, and to address their translation into clinical decision-making.
Why It Matters: Biomarkers are central to advancing immuno-oncology, yet current tools remain imperfect. This session brings together leaders in translational research to discuss how spatial biology, transcriptomics, imaging, and integrated predictors can sharpen patient stratification and optimize immunotherapy outcomes in 2025 and beyond.
Special Session – Costs and Benefits of Immunotherapy: Focus on Long-Term Effects
Date/Time: Saturday, 18 October 2025
Room: Karlsruhe Auditorium – Hall 5.2
Chairs: Karin Jordan (Potsdam, Germany) & Alice Indini (Milan, Italy)
This session addresses one of the most important challenges in immuno-oncology—balancing the remarkable benefits of immunotherapy with its long-term clinical, financial, and quality-of-life consequences. Experts will present insights on managing toxicity, evaluating benefit–risk ratios, and understanding chronic complications that shape survivorship and healthcare sustainability.
Key Presentations
- Optimizing the Management of IO-Related Toxicity
Speaker: Christina H. Ruhlmann (Odense, Denmark)
A practical overview of strategies to prevent, diagnose, and mitigate immune-related adverse events, ensuring safety while maintaining efficacy. - Adjuvant Immunotherapy in Melanoma: Balancing NNT and NNH
Speaker: Alexander M. Eggermont (Utrecht, Netherlands)
Examines how to weigh the number needed to treat (NNT) against the number needed to harm (NNH) in the adjuvant setting, providing a framework for risk–benefit assessment in melanoma. - Chronic and Late-Onset Toxicity: Diagnosis, Treatment, and Follow-Up
Speaker: Radu A. Vidra (Cluj-Napoca, Romania)
Focuses on long-term toxicities that may emerge years after therapy, emphasizing monitoring strategies, multidisciplinary management, and patient education. - Financial Burden and Clinical Implications of IO Chronic Toxicity
Speaker: Karin Jordan (Potsdam, Germany)
Explores the economic and healthcare system consequences of prolonged toxicity, including cost-effectiveness considerations and the real-world impact on patients and caregivers. - Q&A and Discussion
A dedicated exchange between faculty and audience to explore practical solutions for integrating cost–benefit evaluation into everyday immunotherapy decision-making.
Why It Matters: As immunotherapy extends survival and reshapes cancer care, the focus is shifting toward its long-term consequences. This session highlights the need to refine strategies that balance durable benefit against toxicity, financial cost, and survivorship challenges—ensuring immunotherapy remains both clinically effective and sustainable for patients and healthcare systems.
Special Session – Navigating Immunotherapy-Related Cardiovascular Risks in Cancer Patients: When Does Oncology Need a Cardiologist?
Date/Time: Saturday, 18 October 2025
Room: Koblenz Auditorium – Hall 5.2
Chairs: Evandro De Azambuja (Brussels, Belgium) & Teresa Lopez Fernandez (Madrid, Spain)
This session focuses on one of the most pressing challenges in the era of immunotherapy: the intersection of oncology and cardiology. With immune checkpoint inhibitors (ICIs) increasingly used across tumor types, recognition and management of cardiovascular toxicities are becoming essential to optimize outcomes and patient safety.
Key Presentations
- Mechanisms of Immunorelated Toxicity
Speaker: James Larkin (London, United Kingdom)
An overview of the biological pathways driving cardiovascular complications during ICI therapy, from myocarditis to arrhythmias, setting the stage for clinical management. - Clinical Case 1: Cardiovascular Surveillance During ICI Therapy
Real-world case-based learning focused on early detection and monitoring strategies while patients are actively receiving immunotherapy. - Clinical Case 2: Cardiovascular Surveillance Post-ICI Therapy
Speaker: Thomas Suter (Bern, Switzerland)
Discussion of long-term cardiac risks and surveillance approaches once ICI therapy has been completed, highlighting survivorship care. - Immunotherapy in 2025: Emerging Combinations and Evolving Cardiovascular Challenges
Speaker: Valentina Guarneri (Padova, Italy)
A forward-looking perspective on how novel IO combinations may introduce new cardiovascular risks, emphasizing the need for cardio-oncology collaboration. - Q&A and Discussion
An interactive exchange exploring multidisciplinary solutions, shared-care models, and future directions in managing cardiovascular toxicity.
Why It Matters: As immunotherapy moves into earlier disease settings and combinations expand, cardiovascular risks are increasingly recognized as a limiting factor in treatment. This session underscores the importance of proactive surveillance, multidisciplinary care, and evolving cardio-oncology collaborations to ensure that patients benefit fully from immunotherapy without compromising heart health.
EONS Industry Satellite Symposium – Subcutaneous Immunotherapy in Oncology: Optimizing Treatment Delivery Across Care Settings
Date/Time: Saturday, 18 October 2025
Room: Oldenburg Auditorium – Hall 5.1
Chair: Lena Sharp (Stockholm, Sweden)
This BMS-supported symposium focuses on the growing role of subcutaneous (SC) immunotherapy in oncology and its integration into everyday clinical practice. The session highlights multidisciplinary perspectives—from clinicians and pharmacists to nurses and patients—showing how SC delivery is reshaping cancer care.

Key Presentations
- Opening Remarks
Lena Sharp (Stockholm, Sweden) - Clinical Considerations on SC Immunotherapy Delivery
Theodoros Foukakis (Stockholm, Sweden)
Overview of clinical evidence, pharmacologic equivalence to IV formulations, and scenarios where SC delivery can optimize patient outcomes. - Implementing SC Immunotherapy Options into Practice: The Role of the Pharmacist
Christophe Bardin (Paris, France)
Insight into how pharmacists streamline workflows, ensure safety, and manage resource allocation with SC immunotherapy. - Implementing SC Immunotherapy Options into Practice: The Role of the Nurse
Zoe O’Neil (Coventry, United Kingdom)
Practical guidance on administration, patient monitoring, and managing injection-related toxicities from the nursing perspective. - SC Immunotherapy Treatment Options from a Patient Perspective
Racha Kussaibati (Birmingham, United Kingdom)
Exploration of patient-reported outcomes, convenience, reduced chair time, and quality-of-life improvements with SC delivery. - Q&A & Discussion
Led by Lena Sharp
Multidisciplinary dialogue on barriers, opportunities, and the future of SC immunotherapy adoption across diverse care settings. - Concluding Remarks
Olivia Sharp (London, United Kingdom)
Why It Matters: This session underscores how SC immunotherapy can improve patient convenience, increase healthcare efficiency, and expand access in resource-limited settings. By addressing clinical, logistical, and patient-centered considerations, it provides a comprehensive framework for integrating SC delivery into oncology practice.
Keynote Lecture – Therapeutic Cancer Vaccines: Clinical Perspectives
Date/Time: Sunday, 19 October 2025
Room: Munich Auditorium – CityCube B
Speaker: Catherine Wu (Boston, United States of America)
Session Overview
This keynote lecture is dedicated to one of the most dynamic and rapidly evolving areas in oncology: therapeutic cancer vaccines. Unlike prophylactic vaccines that prevent infections, therapeutic cancer vaccines are designed to stimulate the patient’s immune system to recognize and attack established tumors.
Structure of the Session
Introduction – A brief framing of the current challenges in cancer immunotherapy, including resistance to checkpoint inhibitors and the need for durable, antigen-specific responses.
Therapeutic Cancer Vaccines: Clinical Perspectives
Delivered by Catherine Wu (Boston, USA), a global leader in cancer immunology and vaccine development. The lecture will cover:
- Advances in neoantigen-based personalized vaccines, where unique tumor mutations are leveraged to design individualized therapies.
- Insights from clinical trials showing how vaccines can deepen responses to checkpoint inhibitors and potentially reduce relapse rates.
- The current landscape of vaccine technologies, including mRNA platforms, dendritic cell vaccines, peptide-based approaches, and viral vectors.
- Challenges such as tumor heterogeneity, immune escape, and the logistics of personalization.
The future outlook, highlighting integration of cancer vaccines with checkpoint blockade, cellular therapies, and next-generation adjuvants.
Why It Matters: Cancer vaccines represent a frontier in precision oncology. By mobilizing T cells against patient-specific tumor targets, they offer the possibility of long-lasting disease control with minimal toxicity. Catherine Wu’s lecture is expected to provide a visionary overview of how far the field has come and where it is heading—placing vaccines as a critical piece in the evolving immunotherapy ecosystem.
Special Symposium – CTLA-4 Blockade: The Story Is Not Over Yet
Date/Time: Monday, 20 October 2025,
Room: Nuremberg Auditorium – Hall 5.2
Chairs: Paolo A. Ascierto (Naples, Italy) & Suzanne L. Topalian (Baltimore, USA)
Session Overview
CTLA-4 blockade, one of the earliest immune checkpoint strategies, continues to evolve more than a decade after its first clinical success. This symposium revisits the biology, historical development, and modern applications of CTLA-4 inhibitors, while exploring how this pathway is being redefined in combination regimens and novel strategies.
Programme Highlights
- Mechanism of Action – Sergio Quezada (London, UK)
A detailed look at how CTLA-4 blockade reactivates T-cell priming and expands antitumor immunity. - Historical Development – Suzanne L. Topalian (Baltimore, USA)
A perspective on the discovery, early clinical trials, and the pivotal role of CTLA-4 blockade in launching the era of immuno-oncology. - Current Use of CTLA-4: From Monotherapy to Combinations – Paolo A. Ascierto (Naples, Italy)
Updates on where CTLA-4 inhibitors stand in modern oncology, with emphasis on combination regimens with PD-1/PD-L1 agents across tumor types. - Rediscovering CTLA-4 Blockade – Stephane Champiat (Houston, USA)
Exploration of emerging strategies to optimize CTLA-4 therapy, including novel dosing, next-generation antibodies, and biomarker-driven approaches. - Q&A and Discussion – Interactive session to debate whether CTLA-4 will remain a cornerstone or become a niche tool in precision immunotherapy.
Why It Matters: While PD-1/PD-L1 inhibitors dominate today’s landscape, CTLA-4 blockade remains clinically relevant and scientifically intriguing. Its continued evolution—particularly in rational combinations—could unlock new opportunities for durable responses and broaden the impact of immunotherapy across cancer types.


