Thyroid cancer is a type of cancer that begins in the thyroid gland, a small, butterfly-shaped gland located at the base of the neck. The thyroid produces hormones that regulate heart rate, blood pressure, body temperature, and metabolism. When cells in the thyroid grow uncontrollably, they can form a tumor and spread to other parts of the body.
According to the American Cancer Society, about 44,000 new cases of thyroid cancer are expected in the U.S. in 2025, with women making up the majority. It’s typically diagnosed around age 51, which is younger than most other adult cancers. Women are nearly three times more likely to be affected than men, and the disease is 40–50% less common in Black individuals than in other racial or ethnic groups.
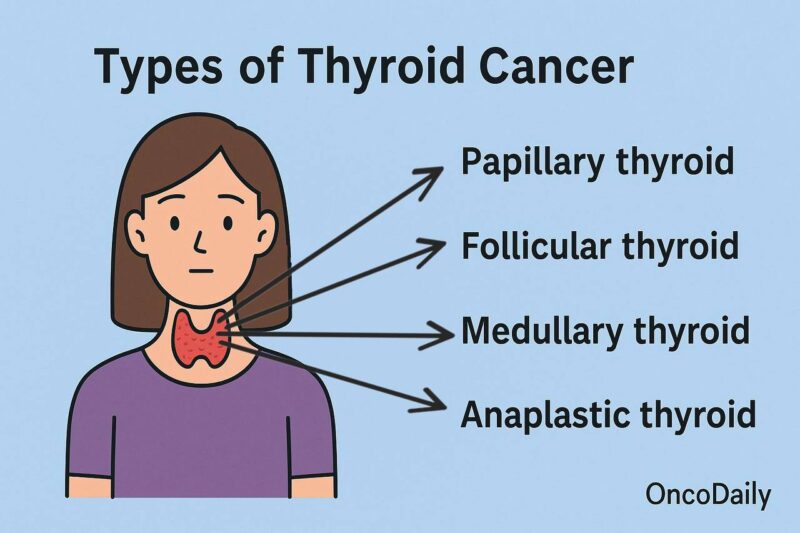
Types of Thyroid cancer
The thyroid plays a key role in regulating the body’s metabolism and calcium balance through the hormones it produces. It comes in several forms, depending on the type of cell it originates from. The most common types include differentiated, medullary, and anaplastic thyroid cancer.
The gland contains two main types of cells:
- Follicular cells use iodine to produce thyroid hormones that control metabolism.
- C cells (or parafollicular cells) make calcitonin, a hormone that helps manage calcium levels in the body.
There are also other less common cells, like immune system (lymphocyte) and supportive (stromal) cells. Different types of thyroid cancer can arise depending on which cell type becomes abnormal.
According to the American Cancer Society, thyroid cancer comes in several types based on the cells it originates from. The most common is papillary thyroid cancer, making up about 80% of cases, followed by follicular thyroid cancer at around 10%. These are classified as differentiated thyroid cancers because their cells resemble normal thyroid tissue. Less common types include medullary thyroid cancer, which accounts for 2-4% of cases, and anaplastic thyroid cancer, a rare and aggressive form that makes up about 1%.
Differentiated Thyroid Cancers
These are the most common types and develop from follicular cells. Under a microscope, the cancer cells look similar to normal thyroid tissue.
Papillary thyroid cancer is the most common type (80%). It grows slowly, often in one lobe of the thyroid, and may spread to the neck lymph nodes. Even when it spreads, it usually responds well to treatment.
- Papillary microcarcinoma,
- Follicular variant of PTC
- Encapsulated variant of PTC,
- Papillary microcarcinoma,
- Columnar cell variant of PTC,
- Oncocytic variant of PTC
Follicular thyroid cancer is another form of differentiated cancer that is more likely to spread through the bloodstream than to lymph nodes. It can metastasize to distant organs, such as the lungs or bones, and is more common in areas where iodine intake is low.
Variants include:
- FTC, minimally invasive
- FTC, encapsulated angioinvasive
- FTC, widely invasive
Oncocytic carcinoma (Hürthle cell cancer) is a rare subtype, harder to detect and treat, with a higher risk of recurrence.
Medullary Thyroid Cancer
Medullary thyroid cancer (MTC) arises from C cells in the thyroid, which are responsible for producing calcitonin. This cancer is distinct from differentiated types and has unique clinical features.
There are two main forms of MTC:
- Sporadic MTC is the most common type. It usually occurs in adults and typically affects only one lobe of the thyroid. This form is not inherited and develops without a known family history.
- Familial MTC is inherited and often appears in childhood or early adulthood. It usually affects both lobes of the thyroid and may be part of a genetic syndrome known as multiple endocrine neoplasia type 2 (MEN2). People with this inherited form may also be at risk for other types of endocrine tumors.
Because of its potential to be inherited, genetic testing is often recommended for individuals diagnosed with MTC to guide treatment and help identify at-risk family members.
Anaplastic and Rare Thyroid Cancer
Anaplastic thyroid cancer is a rare and extremely aggressive form. It often develops from pre-existing papillary or follicular thyroid cancer and tends to spread quickly, making it one of the most challenging thyroid cancers to treat.
There are also other rare types of thyroid cancer, which include thyroid lymphoma, sarcoma, squamous cell carcinoma, and a few other very uncommon tumors. These rare forms each have unique characteristics and may require different treatment approaches compared to the more common types of thyroid cancer.
Risk Factors for Thyroid Cancer
Thyroid cancer risk factors can increase your chances of developing the disease. While having one or more risk factors doesn’t guarantee thyroid cancer, recognizing them can aid in early detection and prevention efforts.
Gender and Age
This type of cancer is significantly more common in women than in men, with women being about three times more likely to develop the condition. The disease can affect people of any age, but it is most commonly diagnosed between the ages of 30 and 60, particularly in women.
Family History and Genetics
A family history of thyroid cancer or certain genetic conditions can increase your risk. Key inherited conditions linked to thyroid cancer include:
- Multiple Endocrine Neoplasia type 2 (MEN2): Increases the risk of medullary thyroid cancer.
- Familial Adenomatous Polyposis (FAP): Often associated with papillary thyroid cancer.
- Cowden Syndrome: Linked to papillary and follicular thyroid cancer.
- Carney Complex: A rare condition that can lead to early-onset thyroid cancers.
If there is a history of these genetic syndromes in your family, consider genetic counseling and testing to assess your risk.
Radiation Exposure
Radiation exposure, especially during childhood, is a well-known risk factor for thyroid cancer. Individuals who received radiation treatments for other medical conditions early in life have a higher chance of developing thyroid cancer later on. Similarly, those exposed to nuclear fallout, such as during the Chernobyl disaster, are at increased risk. Even though the radiation from routine childhood imaging—like CT scans or X-rays—is much lower, frequent exposure over time may still contribute slightly to thyroid cancer risk.
Body Weight
Body weight can also influence the likelihood of developing thyroid cancer. Research has shown that being overweight or obese increases the risk, with the chances rising alongside a person’s body mass index (BMI). Obesity appears to be a contributing factor to both the development and progression of thyroid cancer, though the exact reasons for this link are still being studied.
Iodine Levels in Diet
The amount of iodine in a person’s diet plays a role in thyroid health and cancer risk. Low iodine intake has been associated with a higher chance of developing follicular thyroid cancer, while very high iodine levels may increase the risk of papillary thyroid cancer. In countries like the United States, where iodized salt is commonly used, iodine deficiency is rare. However, it can still occur in some regions or among people with restricted diets.
Thyroid Cancer and Gene Mutations: Causes, Types, and Testing
The cancer develops when genetic mutations cause thyroid cells to grow out of control. While the exact reason these mutations happen isn’t always known, they can be inherited or acquired over time due to environmental exposures like radiation or random errors during cell division. Most thyroid cancers result from acquired mutations rather than those passed down through families.
Understanding the Role of Gene Mutations
Genes regulate how our cells grow, divide, and repair themselves. When mutations occur in certain genes—such as oncogenes, tumor suppressor genes, or DNA repair genes—they can disrupt normal cell behavior and lead to cancer. Some mutations push cells to divide too quickly, while others stop the body from repairing damage or slowing down cell growth.
Gene Changes in Different Types of Thyroid Cancer
Each form of thyroid cancer is tied to specific genetic alterations:
- Papillary thyroid cancer (most common) often involves mutations in BRAF, RAS, or RET genes. The BRAF mutation, in particular, keeps the gene constantly active, fueling tumor growth.
- Follicular thyroid cancer typically features mutations in the RAS gene or a PAX8-PPARγ gene fusion, which disrupts normal cell function.
- Anaplastic thyroid cancer, an aggressive and fast-spreading type, usually starts from a less aggressive form and accumulates mutations like TP53, causing rapid progression.
- Medullary thyroid cancer is commonly associated with RET gene mutations. Inherited forms—often part of syndromes like MEN2—are present in all cells and can be passed to children. Sporadic cases show mutations only in tumor cells.
Why Genetic Testing Matters?
Identifying these gene mutations is key for accurate diagnosis and treatment planning. Some therapies are specifically designed to target mutated genes. For those with a personal or family history of MTC, genetic counseling and testing can help determine inherited risk and guide early intervention.
Read more about Sofia Vergara and Thyroid Cancer: How She Went Against, How She Survived on OncoDaily.
Symptoms of Thyroid Cancer
In its early stages, The disease often develops silently. Most people don’t notice any obvious symptoms at first, and the disease is frequently discovered during routine checkups or imaging tests done for unrelated reasons.
As the tumor grows, however, it may begin to make its presence known through subtle but progressive changes. You might notice a small lump or swelling in your neck that wasn’t there before. For some, the collar of a shirt may suddenly start to feel snug around the neck, even if it fit comfortably before.
Other changes may affect your voice. A growing thyroid nodule can press on nearby structures, leading to a hoarse or raspy tone that doesn’t go away. Swallowing might also become more difficult over time, especially if the tumor is pressing on the esophagus.
In some cases, nearby lymph nodes become enlarged, causing visible or tender swelling in the neck. You might also experience persistent discomfort or a dull ache in your throat or neck.
While these symptoms aren’t always signs of thyroid cancer, it’s important to have them evaluated, especially if they don’t improve with time.
How is Thyroid Cancer Diagnosed?
Thyroid cancer is often discovered in one of three ways: during a routine checkup, while investigating other health concerns, or after noticing a lump or changes in the neck. If there’s a reason to suspect cancer, your doctor will follow up with a series of tests to confirm the diagnosis and understand how far the disease has progressed. (National Comprehensive Cancer Network, version 1.2025)
Physical Exam and Medical History
The diagnostic process for thyroid cancer typically begins with a detailed conversation between the patient and doctor. This includes reviewing symptoms, personal and family medical history, and any known risk factors—such as radiation exposure or a family history of thyroid disease. During the physical exam, the doctor carefully feels the neck for any unusual lumps, such as thyroid nodules or enlarged lymph nodes, which could indicate a problem.
Imaging Tests
If the physical exam raises concerns, imaging tests are often the next step. Ultrasound is the most commonly used tool—it helps determine whether a thyroid nodule is solid or fluid-filled and whether nearby lymph nodes look suspicious. Depending on the findings, additional imaging may be needed. CT scans or MRIs can help assess whether the cancer has spread beyond the thyroid. Radioiodine scans are sometimes used after surgery to detect any remaining thyroid tissue or cancer, especially in papillary and follicular thyroid cancers. PET scans may be used for cancers that don’t absorb iodine and require alternative imaging techniques.
Laryngoscopy
When a patient reports voice changes, a laryngoscopy may be performed to examine the vocal cords. This is especially important before thyroid surgery, as it helps assess whether the vocal cords are functioning normally.
Blood Tests
Blood tests can offer valuable insights, although thyroid function tests like TSH, T3, and T4 are often normal in thyroid cancer. After treatment, thyroglobulin levels can help monitor for recurrence. In cases of medullary thyroid cancer (MTC), calcitonin and carcinoembryonic antigen (CEA) levels are useful for both diagnosis and follow-up. For patients with a family history or genetic risk, blood tests may also be used to check for related conditions like pheochromocytomas.
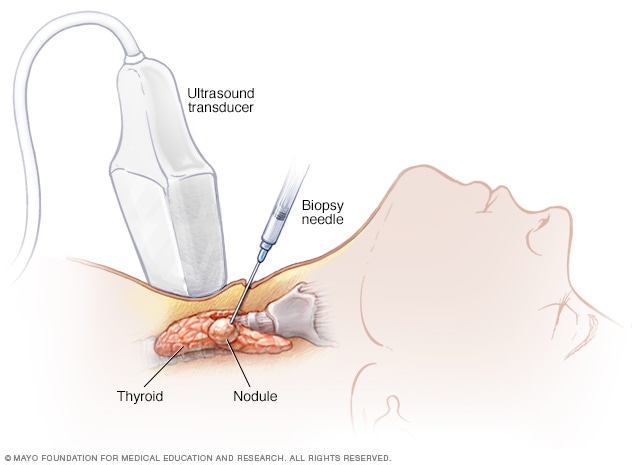
Biopsy
The only way to definitively diagnose thyroid cancer is through a biopsy. The most common approach is a fine needle aspiration (FNA), where a thin needle is used to collect cells from a suspicious nodule, often guided by ultrasound for precision.
If the FNA doesn’t provide a clear answer, further testing may involve:
- Core needle biopsy
- Surgical biopsy or lobectomy (removal of one thyroid lobe)
In some cases, molecular testing is done on biopsy samples to look for specific genetic mutations like BRAF or RET/PTC, which can guide treatment decisions.
How Thyroid Cancer Is Treated?
According to the American Cancer Society, the treatment of thyroid cancer depends on several factors, including the type, stage, and extent of the disease. The goal of treatment is to remove or destroy cancer cells while minimizing damage to surrounding healthy tissue. Treatment options typically include surgery, radiation therapy, chemotherapy, and targeted drug therapies. Each treatment plan is individualized based on the patient’s specific diagnosis and overall health.
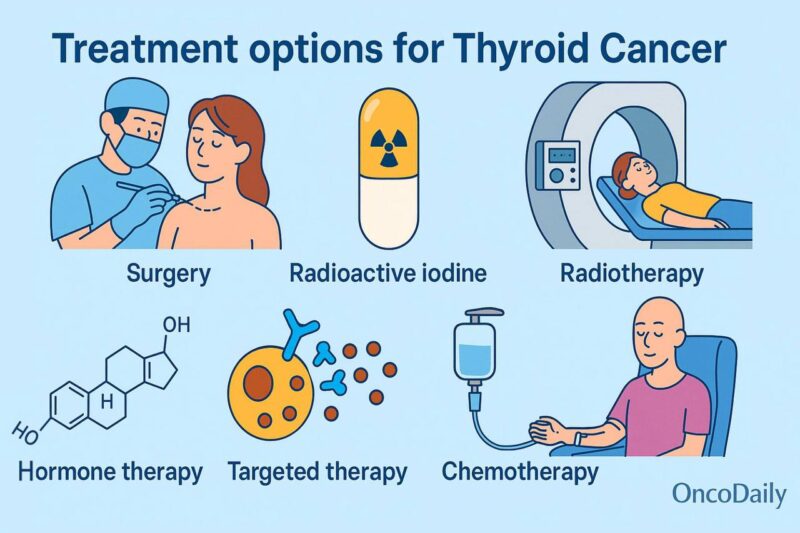
Surgery for Thyroid Cancer
Surgery is the main treatment for most thyroid cancers, except some aggressive types like anaplastic thyroid cancer. If a fine needle aspiration (FNA) confirms cancer, doctors usually recommend removing the tumor and either part or all of the thyroid gland.
Thyroidectomy
This is the most common surgery, especially for larger or higher-risk tumors. If the entire thyroid is removed, it’s called a total thyroidectomy. If most but not all of the gland is taken out, it’s a near-total thyroidectomy. After this surgery, patients need daily thyroid hormone pills (levothyroxine) for life. One advantage is better monitoring for recurrence using specialized tests like radioiodine scans and thyroglobulin levels.
Lobectomy
In this procedure, only the thyroid lobe with the cancer is removed, along with the isthmus (the thin strip connecting the lobes). This is often done for small, low-risk tumors or when a biopsy result is unclear. Since part of the thyroid remains, some people may not need hormone pills, but it might limit the accuracy of follow-up tests for recurrence.
Lymph Node Removal
If cancer has spread to nearby lymph nodes, especially in the neck, they may be removed during thyroid surgery. This is more common with larger tumors, cancers that extend beyond the thyroid, or more aggressive types like medullary or anaplastic thyroid cancer. Central neck dissection targets lymph nodes near the thyroid, while more extensive surgery (modified radical neck dissection) includes nodes along the sides of the neck.
Chemotherapy for Thyroid cancer
Chemotherapy—medications that travel through the bloodstream to attack cancer cells—is rarely used for most types of thyroid cancer.
However, in aggressive cases like anaplastic thyroid cancer, chemo may be used alongside radiation. It might also be considered when the cancer has spread and other treatments like surgery or targeted therapy aren’t an option. Even then, targeted drugs are often tried first since they tend to be more effective.
When chemo is used, it’s given in cycles with breaks in between to help the body recover. The treatment can involve a single drug or a combination, usually delivered through an IV, though some are available in pill form. Common chemo drugs for thyroid cancer include doxorubicin, cisplatin, paclitaxel, and others, depending on the case.
While chemo isn’t a frontline treatment for thyroid cancer, it can play a role in rare.
Chemotherapy Side Effects in Thyroid Cancer
Chemotherapy can impact healthy cells along with cancer cells, leading to side effects that vary depending on the drug, dose, and duration of treatment. Common issues include fatigue, nausea, appetite loss, mouth sores, hair loss, and changes in bowel habits. It may also weaken the immune system, making infections, bruising, or bleeding more likely.
These side effects are usually temporary and can often be managed with supportive medications. Some drugs, like Doxorubicin, may affect heart function, so regular heart monitoring is recommended. Others, such as cisplatin, carboplatin, and paclitaxel, can cause nerve damage, leading to pain, tingling, or sensitivity in the hands and feet, a condition known as peripheral neuropathy.
Patients are encouraged to talk to their care team about what to expect and how to manage potential side effects.
Radioactive iodine for Thyroid Cancer
RAI therapy is a targeted treatment used after thyroid surgery, mainly for papillary and follicular thyroid cancers. It works by using radioactive iodine—usually taken as a pill—to destroy any remaining thyroid tissue or cancer cells. Because only thyroid cells absorb iodine, other parts of the body are mostly unaffected.
When Is RAI Used?
RAI therapy is often recommended after surgery to remove any remaining thyroid tissue and lower the risk of cancer recurrence. It is also used to treat cancer that has spread to lymph nodes or other areas of the body. By targeting iodine-absorbing cancer cells, RAI helps ensure thorough treatment and improve long-term outcomes.
RAI is not effective for anaplastic or medullary thyroid cancers.
Before radioactive iodine (RAI) treatment, the patient’s thyroid-stimulating hormone (TSH) levels must be high to improve iodine uptake by thyroid cells. This can be achieved either by stopping thyroid hormone medication for a few weeks or by administering synthetic TSH injections (Thyrogen) while continuing the usual medication.
A low-iodine diet is also required for one to two weeks before therapy. Patients are advised to avoid iodized salt, dairy products, seafood, soy, eggs, and foods containing red dye #3 to help remaining thyroid cells absorb the radioactive iodine more effectively.
What Happens During and After RAI Treatment?
RAI is typically administered as a single dose in a hospital or outpatient clinic. After treatment, the patient’s body emits small amounts of radiation for several days. During this time, they must limit close contact with others, especially children and pregnant women, and avoid public transport. They are also encouraged to drink plenty of fluids to help eliminate the radioactive iodine through urine and to follow hygiene precautions at home to minimize radiation exposure to others.
RAI Side Effects
Short-term side effects may include nausea, dry mouth, altered taste, watery or dry eyes, and swelling of the salivary glands. In rare cases, long-term effects can occur, such as temporary menstrual changes in women, reduced sperm count in men after high doses, or a slightly increased risk of secondary cancers like leukemia or salivary gland cancer.
Physicians typically advise women to wait at least six months after treatment before attempting pregnancy.
External Radiation Therapy for Thyroid Cancer
External radiation therapy uses high-energy rays to target and destroy cancer cells or slow their growth. A machine directs focused beams of radiation from outside the body. This treatment is commonly used for medullary or anaplastic thyroid cancers, which do not absorb iodine.
While radioiodine therapy is typically preferred for iodine-absorbing cancers (like papillary and follicular thyroid cancers), external radiation may be considered if radioiodine is ineffective or if the cancer has spread beyond the thyroid. It’s often used to treat or relieve symptoms of cancers that have spread or to prevent recurrence after surgery.
How does ERT work?
External radiation to the neck is usually given five days a week for several weeks. The treatment is painless and similar to an x-ray, but it takes a few minutes, with additional time spent on positioning the patient correctly.
ERT Side Effects
While effective, radiation can also affect nearby healthy tissues. Common side effects include skin changes like sunburn, difficulty swallowing, dry mouth, hoarseness, and fatigue. To minimize damage, doctors carefully plan the treatment using advanced techniques like intensity-modulated radiation therapy (IMRT), ensuring the radiation is precisely targeted to the cancer cells.
Learn more about Side Effects of Radiotherapy: Risks and What to Know on OncoDaily.
Targeted Therapy for Thyroid Cancer
Targeted drug therapy has become a promising treatment option for this cancer in recent years. Unlike standard chemotherapy, which targets rapidly dividing cells, targeted drugs focus on specific gene and protein changes within cancer cells, making them more precise and often more effective.
Papillary and Follicular Thyroid Cancer: Multikinase inhibitors like Lenvatinib, Sorafenib, and Cabozantinib target several kinases. These drugs can block the formation of new blood vessels and inhibit proteins that cancer cells rely on for growth. They are often used when radioactive iodine treatment is no longer effective.
Common side effects include fatigue, nausea, skin rashes, and high blood pressure. In some cases, more serious effects like severe bleeding or intestinal issues may occur.
Medullary Thyroid Cancer (MTC): For MTC, where radioactive iodine therapy is ineffective, Vandetanib and Cabozantinib are used. These multikinase inhibitors block tumor growth and blood vessel formation. Common side effects include diarrhea, nausea, and high blood pressure, while rare but serious effects may involve heart rhythm problems or infections.
RET inhibitors like Selpercatinib are another option for advanced MTC, especially when cancer cells have specific RET gene changes. These drugs can also cause side effects like dry mouth, diarrhea, and high blood pressure.
Read more about Selpercatinib (Retevmo): Uses in Cancer, Side Effects, Dosage, Expectations on OncoDaily.
Anaplastic Thyroid Cancer: Targeted drugs like BRAF and MEK inhibitors (e.g., Dabrafenib and Trametinib) can be effective for cancers with BRAF gene mutations. These drugs target proteins that help cancer cells grow. Side effects include skin issues, muscle pain, and fatigue, with a risk of skin cancers.
RET inhibitors (e.g., Selpercatinib and Pralsetinib) and TRK inhibitors (e.g., Larotrectinib) are also used for anaplastic thyroid cancers with specific gene mutations. These medications can cause side effects like dizziness, nausea, and liver damage, but they may offer new hope for advanced cases.
Targeted drugs are taken orally, usually once or twice daily, and offer a more targeted approach to treating thyroid cancer compared to traditional chemotherapy. However, like all treatments, they come with the potential for side effects. Patients should work closely with their healthcare team to monitor any adverse reactions and adjust the treatment plan as needed.
By targeting specific molecular changes in thyroid cancer cells, targeted drugs represent an important advancement in cancer therapy, providing new options for patients with advanced or refractory thyroid cancers.
Read about Targeted Therapy vs Immunotherapy on OncoDaily.
Stages of Thyroid Cancer
Thyroid cancer staging helps doctors understand how far the disease has progressed, which guides treatment planning. According to the NCCN, the staging of thyroid cancer depends on the type of thyroid cancer, and it will be discussed separately for each type (medullary, differentiated and anaplastic) below. (National Comprehensive Cancer Network, version 1.2025)
Staging for Medullary Thyroid Cancer
Stage I: The tumor is 2 cm or smaller and limited to the thyroid, with no spread to lymph nodes or distant sites.
Stage II: The tumor is larger than 2 cm or has grown into nearby neck muscles, but it hasn’t spread to lymph nodes or other parts of the body.
Stage III: The cancer has spread to nearby central neck lymph nodes but not to distant sites.
Stage IVA: The tumor has either spread to more distant neck lymph nodes or invaded nearby neck structures like the trachea or esophagus, but hasn’t spread beyond the neck.
Stage IV B: The tumor has grown into major neck structures such as the spine or large blood vessels, without distant spread.
Stage IVC: The cancer has spread to distant organs like the lungs, liver, bones, or brain, regardless of tumor size or lymph node involvement.
Staging for Differentiated Thyroid Cancer
For people under 55, differentiated thyroid cancer is staged simply:
Stage I:if it hasn’t spread beyond the neck
Stage II: if it has spread to distant parts of the body
For people 55 Years and Older, differentiated thyroid cancer is staged:
Stage I: The tumor is still confined to the thyroid. It may be small (under 2 cm) or up to 4 cm in size. There’s no spread to lymph nodes or other parts of the body.
Stage II: Cancer is still limited to the thyroid or nearby neck muscles but may have spread to nearby lymph nodes. There’s still no distant spread.
Stage III: The tumor has grown beyond the thyroid into nearby neck structures like the windpipe, voice box, or esophagus, but hasn’t spread to distant organs.
Stage IVA: The cancer has extended further into critical areas like large blood vessels or near the spine, though it still hasn’t spread beyond the neck.
Stage IV : The cancer has spread to distant parts of the body, such as the lungs, bones, or brain. This is considered advanced-stage thyroid cancer.
Staging for Anaplastic Cancer
Anaplastic thyroid cancer is considered advanced from the start and is always staged as stage IV, with subcategories IVA, IVB, and IVC.
Stage IVA means the tumor is still confined to the thyroid and hasn’t spread to lymph nodes or distant sites.
Stage IVB includes tumors that have grown into nearby neck muscles or tissues, or have spread to lymph nodes, but not to distant organs.
Stage IVC is the most advanced stage, where the cancer has spread to distant parts of the body, such as the lungs, bones, or brain, regardless of the tumor size or lymph node involvement.
Thyroid cancer Prognosis and Outcomes
A 5-year relative survival rate compares people with a specific type and stage of thyroid cancer to those without it, showing the likelihood of living at least five years after diagnosis. These rates come from the SEER database, which groups thyroid cancer into localized (still in the thyroid), regional (spread nearby), and distant (spread to distant organs).
According to the American Cancer Society, for papillary and follicular thyroid cancers, survival is excellent, over 99% if localized. Medullary cancer also has high survival when caught early, but drops to 43% with distant spread. Anaplastic thyroid cancer has the lowest rates, with just 4% surviving five years if it has spread.
These stats don’t account for individual factors like age or treatment advances, and many people diagnosed today may have better outcomes.
Thyroid Cancer Latest Research in 2025
Poster Abstract 48P, presented at the ESMO Sarcoma and Rare Cancers Congress 2025, examines survival outcomes in patients with Hürthle cell carcinoma (HCC), a rare thyroid cancer. Data from 5,119 patients (2000-2021) showed 5-, 10-, and 20-year survival rates of 87.95%, 77.64%, and 58.49%, respectively. Males had worse survival (mOS 232 months), and survival varied by race, with Hispanics having better long-term outcomes. Lower income and non-metropolitan residency were associated with poorer survival. These findings highlight disparities that require further study.
Poster 55P, presented at the ESMO Sarcoma and Rare Cancers Congress 2025, explored the correlation between serum calcitonin levels and clinical characteristics of medullary thyroid carcinoma (MTC). The study included 43 patients and found that pre-operative calcitonin levels were positively correlated with tumor size and regional lymph node metastases (p<0.01). Patients with calcitonin levels above 1000 pg/ml had remote metastases. Post-surgery, those with calcitonin levels under 1000 pg/ml showed biochemical recovery, with levels dropping below 10 pg/ml. These findings suggest that calcitonin can be used as a prognostic marker in MTC.
Ongoing Trials Associated with Thyroid Cancer
The clinical trial NCT06898437 is investigating 177Lu-LNC1004, a FAP-targeting radiopharmaceutical, in patients with radioiodine-refractory differentiated thyroid cancer (RAIR-DTC) who have failed TKIs or declined standard treatment. Participants receive 80 mCi (±10%) of the drug every six weeks for two cycles, with the possibility of continuing up to six cycles based on response and side effects. The study aims to assess the treatment’s efficacy and safety.
Written by Mariam Khachatryan, MD
FAQ
What are the common types of thyroid cancer?
The most common types of thyroid cancer are papillary thyroid cancer, follicular thyroid cancer, medullary thyroid cancer, and anaplastic thyroid cancer. Each type behaves differently and requires different treatment approaches
What are the risk factors for thyroid cancer?
Risk factors include a family history of thyroid cancer, exposure to radiation, certain genetic conditions (like familial medullary thyroid cancer), and being female, as thyroid cancer is more common in women.
How is thyroid cancer diagnosed?
Diagnosis typically involves a physical exam, imaging tests (such as ultrasound), a biopsy (fine needle aspiration), and blood tests to check for thyroid function or cancer markers like calcitonin.
What treatments are available for thyroid cancer?
Treatment depends on the type and stage of the disease. Common treatments include surgery (thyroidectomy or lobectomy), radioactive iodine therapy, external radiation therapy, and targeted therapy for advanced cases.
Is surgery the main treatment for thyroid cancer?
Yes, surgery is the primary treatment for most types of this cancer. It may involve removing part or all of the thyroid gland. In more advanced cases, surgery may also include removing nearby lymph nodes.
What is radioactive iodine therapy (RAI)?
RAI is a targeted therapy used after thyroid surgery to destroy any remaining thyroid tissue or cancer cells. It involves swallowing a radioactive iodine pill, which is absorbed by thyroid cells, sparing other parts of the body from radiation.