What is Hemangioblastoma?
Hemangioblastomas are rare, benign (non-cancerous) tumors that arise from the cells lining blood vessels in the central nervous system (CNS), including the brain, spinal cord, and retina (back of the eye). These tumors are highly vascular, meaning they are richly supplied with blood vessels and can cause various symptoms depending on their location and size. While these tumors are typically slow-growing, they can still cause significant problems if left untreated, making early diagnosis and appropriate management crucial.
Prevalence and Epidemiology
Hemangioblastomas are relatively uncommon, accounting for approximately 1-2.5% of all intracranial tumors and 2-3% of all intramedullary spinal cord tumors. The overall incidence rate of CNS hemangioblastomas is estimated to be around 0.141 per 100,000 person-years. These tumors can occur at any age, but they are most commonly diagnosed in young to middle-aged adults, with a peak incidence between 30 and 60 years of age.
These tumors can occur sporadically (without a known genetic cause) or in association with an inherited genetic condition called von Hippel-Lindau (VHL) disease. Approximately 70-80% of cases are sporadic, while the remaining 20-30% are associated with VHL disease. Patients with VHL disease have a higher risk of developing multiple hemangioblastomas, as well as other types of tumors and cysts in various organs.
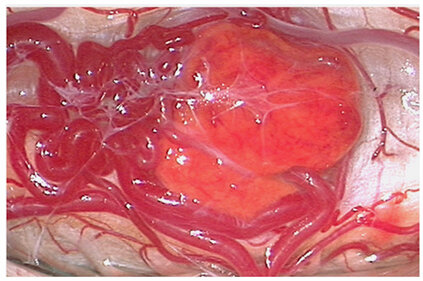
Spinal cord hemangioblastoma. The image is taken from a paper by Dornbos et al. (2018).
Types
Hemangioblastomas can be classified into two main types: sporadic and familial (associated with VHL disease).
- Sporadic Hemangioblastomas: These tumors occur spontaneously and account for approximately 70-80% of all hemangioblastoma cases. Sporadic hemangioblastomas are typically solitary and are most commonly found in the cerebellum (45-50%), followed by the spinal cord (40-45%) and brainstem (5-10%).
- Familial Hemangioblastomas (von Hippel-Lindau Disease): Approximately 20-30% of these tumors are associated with VHL disease, an inherited autosomal dominant disorder caused by mutations in the VHL tumor suppressor gene. Patients with VHL disease are predisposed to developing multiple hemangioblastomas, as well as other types of tumors and cysts in various organs, including the kidneys, pancreas, and adrenal glands.
Causes and Risk Factors
The exact cause of sporadic hemangioblastomas is unknown, but they are believed to arise from genetic mutations or alterations in the VHL tumor suppressor gene or related pathways. These mutations can lead to abnormal cellular growth and the formation of highly vascular tumors.
The primary risk factor for developing hemangioblastomas is having VHL disease, an inherited genetic condition caused by mutations in the VHL gene. Individuals with VHL disease have a significantly increased risk of developing multiple hemangioblastomas, as well as other types of tumors and cysts throughout their lifetime. There is currently no strong evidence linking environmental or lifestyle factors to the development of these tumors.
Symptoms
The symptoms can vary depending on the tumor’s location, size, and the extent of compression on surrounding structures. Some common symptoms include:
Cerebellar Hemangioblastomas
- Headaches
- Nausea and vomiting
- Gait imbalance and ataxia (lack of coordinated movement)
- Dizziness
- Abnormal head positioning
Brainstem Hemangioblastomas
- Headaches
- Nausea and vomiting
- Difficulty swallowing (dysphagia)
- Hiccups
- Weakness or numbness in the arms or legs
- Impaired bladder or bowel function
Spinal Cord Hemangioblastomas
- Back pain
- Weakness or numbness in the arms or legs
- Impaired bladder or bowel function
- Gait disturbances
Retinal Hemangioblastomas
- Blurred vision
- Floaters
- Partial or complete vision loss
In some cases, hemangioblastomas may also cause polycythemia (increased red blood cell production) due to the production of erythropoietin-like substances by the tumor.
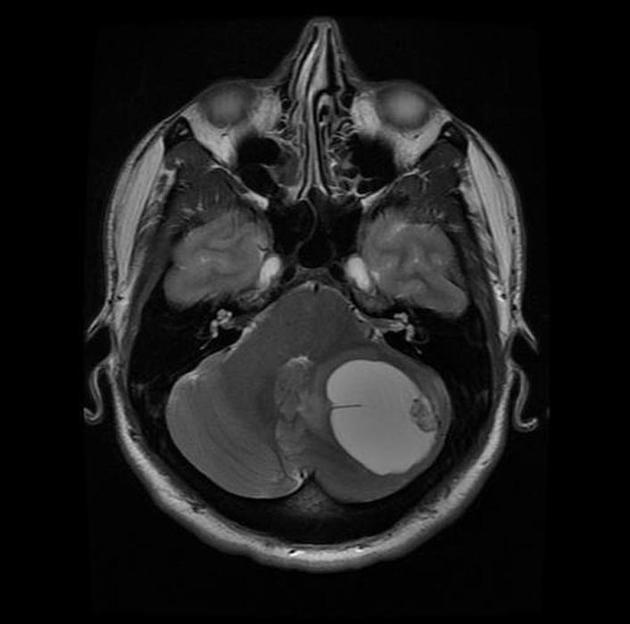
Cerebellar hemangioblastoma. This image is taken from radiopaedia.org.
Diagnosis
The diagnosis of hemangioblastomas typically involves a combination of clinical evaluation, imaging studies, and, in some cases, biopsy or surgical resection.
Imaging Studies
- Magnetic Resonance Imaging (MRI): MRI is the preferred imaging modality for detecting and characterizing hemangioblastomas. These tumors typically appear as well-defined, enhancing masses with a cystic component and surrounding edema.
- Computed Tomography (CT) Scan: CT scans can also be useful in identifying these tumors, particularly in cases where MRI is contraindicated or unavailable.
- Angiography: Cerebral or spinal angiography may be performed to evaluate the tumor’s blood supply and plan for surgical resection.
Treatment Options
The primary treatment for these tumors is surgical resection, aimed at removing as much of the tumor as possible while preserving surrounding healthy tissue and neurological function.
Surgical Resection
- Microsurgical resection is the standard treatment for symptomatic hemangioblastomas, particularly those causing mass effect or compression on surrounding structures.
- The surgical approach depends on the tumor’s location and may involve a craniotomy for brain tumors or a laminectomy for spinal cord tumors.
- Complete resection is often possible for well-circumscribed tumors, but partial resection may be necessary in cases where the tumor is adherent to critical structures or poses a high risk of neurological deficits.
Stereotactic Radiosurgery (SRS)
- SRS, such as Gamma Knife or CyberKnife, may be an option for small, residual, or recurrent hemangioblastomas, particularly in patients with VHL disease or those who are not candidates for open surgery.
- SRS delivers a highly focused dose of radiation to the tumor while minimizing exposure to surrounding healthy tissue.
Radiation Therapy
- Conventional external beam radiation therapy may be considered for inoperable or partially resected hemangioblastomas, particularly in cases where SRS is not feasible or appropriate.
Antiangiogenic Therapy
- Antiangiogenic agents have shown promise in the treatment of hemangioblastomas by targeting the tumor’s vascular supply and inhibiting angiogenesis (the formation of new blood vessels).
- These therapies may be used as neoadjuvant (before surgery) or adjuvant (after surgery) treatments in combination with surgery or radiation therapy.
Patient Survivorship
The long-term prognosis for patients with hemangioblastomas largely depends on the tumor’s location, the extent of surgical resection, and the presence of associated conditions such as VHL disease.
For sporadic hemangioblastomas that are completely resected, the long-term prognosis is generally favorable, with a low risk of recurrence. However, patients with VHL disease may develop new or recurrent hemangioblastomas over time, requiring ongoing surveillance and treatment.
Regular follow-up with imaging studies (e.g., MRI) is typically recommended to monitor for tumor recurrence or the development of new lesions, particularly in patients with VHL disease or those who have undergone partial resection.
Problems During and After Treatment and How to Manage Them
While surgical resection and other treatments for hemangioblastomas can be effective, patients may experience various problems or complications during and after treatment. It is essential to be aware of these potential issues and to work closely with the healthcare team to manage them effectively.
Intraoperative Complications
- Bleeding: Due to the highly vascular nature of these tumors, significant bleeding can occur during surgical resection. Meticulous surgical technique and proper hemostatic measures are crucial to minimize blood loss and potential complications.
- Neurological deficits: Depending on the tumor’s location and proximity to critical structures, there is a risk of neurological deficits, such as weakness, sensory disturbances, or cranial nerve palsies, following surgery.
Postoperative Complications
- Cerebrospinal fluid (CSF) leak: In cases where the tumor involves the dura or spinal cord, there is a risk of CSF leakage, which can lead to headaches, nausea, and an increased risk of infection.
- Hydrocephalus: Hemangioblastomas, particularly those located in the posterior fossa, can cause obstructive hydrocephalus (accumulation of CSF in the brain), which may require temporary or permanent CSF diversion procedures.
- Edema and swelling: Postoperative edema and swelling around the surgical site can cause temporary neurological deficits or increased intracranial pressure, which may require medical management with steroids or other medications.
- Infection: As with any surgical procedure, there is a risk of infection, which can be minimized through proper surgical technique, antibiotic prophylaxis, and wound care.
Long-term Complications
- Recurrence or new tumor development: Patients with VHL disease are at risk for developing new or recurrent hemangioblastomas over time, requiring ongoing surveillance and potential additional treatments.
- Neurological deficits: Depending on the extent of surgical resection and the tumor’s location, some patients may experience long-term neurological deficits, such as weakness, sensory disturbances, or cognitive impairments.
- Vision problems: In cases of retinal hemangioblastomas, vision loss or other visual disturbances may persist, even after treatment.
- Endocrine and metabolic disturbances: Patients with VHL disease may develop endocrine and metabolic disturbances, such as pheochromocytomas (tumors of the adrenal gland) or pancreatic neuroendocrine tumors, which require additional management and treatment.
Recommendations for Patients with Hemangioblastoma
If you or a loved one has been diagnosed with hemangioblastoma, it is essential to understand the condition, its implications, and the steps you can take to manage it effectively. Here are some recommendations to help navigate this journey:
1. Understand Diagnosis
- Educate Yourself: Learn about hemangioblastomas, their nature, and how they affect the body. Understanding the condition aids in making informed care decisions.
- Know the Types: Hemangioblastomas can be sporadic or associated with VHL disease. Identifying the type influences treatment and follow-up care.
2. Seek Specialized Care
- Find a Specialist: Consult with a neurosurgeon or a neuro-oncologist who has experience in treating hemangioblastomas. Specialists can provide the most up-to-date and effective treatment options.
- Multidisciplinary Approach: Consider a healthcare team that includes neurosurgeons, radiation oncologists, genetic counselors, and other specialists to address all aspects of your condition.
3. Regular Monitoring and Follow-Up
- Imaging Studies: Regular MRI or CT scans are crucial for monitoring the tumor’s status and detecting new growths, especially with VHL disease.
- Routine Check-Ups: Schedule regular follow-up appointments to track the condition and manage symptoms or complications promptly.
4. Manage Symptoms and Complications
- Symptom Management: Work with the healthcare team to manage symptoms such as headaches, nausea, and neurological deficits. Medications and supportive therapies can help improve the quality of life.
- Address Complications: Be aware of potential complications such as CSF leaks, hydrocephalus, and infections. Prompt treatment of these issues is essential.
5. Genetic Counseling and Testing
- VHL Disease: For hemangioblastomas associated with VHL disease, genetic counseling and testing for family members may be recommended. Early detection and management of VHL-related tumors can improve outcomes.
6. Lifestyle and Support
- Healthy Lifestyle: Maintain a balanced diet, regular exercise, and adequate rest to support overall well-being.
- Support Networks: Join support groups or connect with others who have hemangioblastomas or VHL disease. Sharing experiences and advice can provide emotional support and practical tips.
7. Stay Informed
- Research and Advances: Stay informed about new research and advances in the treatment of hemangioblastomas. Clinical trials may offer access to new therapies.
- Patient Advocacy: Advocate for yourself by asking questions, seeking second opinions, and being an active participant in your care.
8. Emergency Preparedness
- Recognize Symptoms: Be aware of symptoms that may indicate complications, such as severe headaches, sudden neurological changes, or signs of infection. Seek medical attention promptly if these occur.
- Emergency Plan: Have an emergency plan in place, including contact information for healthcare providers and instructions for seeking urgent care.
Prognosis
The prognosis for these tumors largely depends on the tumor’s location, size, and the extent of surgical resection. With complete surgical removal, the long-term prognosis for sporadic hemangioblastomas is generally favorable, with a low risk of recurrence. However, patients with VHL disease may develop new or recurrent hemangioblastomas over time, requiring ongoing surveillance and treatment.
Conclusion
Hemangioblastomas are rare, benign tumors primarily affecting the central nervous system, including the brain, spinal cord, and retina. They can occur sporadically or in association with VHL disease, an inherited genetic disorder.
Understanding the causes, risk factors, and symptoms of these tumors is crucial for early diagnosis and effective management. Regular monitoring and a multidisciplinary approach are essential for managing potential complications and improving patient outcomes. With appropriate care, many patients with hemangioblastomas can achieve favorable long-term prognoses and maintain a good quality of life.
In this video, Bridget shares her experience as a hemangioblastoma patient. The video is produced by Johns Hopkins Medicine.
Sources
-
- American Cancer Society – Cancer. org
- National Cancer Institute – Cancer.gov
- Radiopaedia – Radiopedia.org
- American Society of Clinical Oncology – Asco.org
- Assessment of care pattern and outcome in hemangioblastoma – Scientific Reports
- Hemangioblastoma and von Hippel-Lindau disease: genetic background, spectrum of disease, and neurosurgical treatment – Child’s Nervous System