What is renal cell carcinoma?
Renal cell carcinoma (RCC), also known as renal cell cancer or renal cell adenocarcinoma, is the most common type of kidney cancer. About 9 out of 10 kidney cancers are renal cell carcinomas. Although RCC usually grows as a single tumor within a kidney, sometimes there are 2 or more tumors in one kidney or even tumors in both kidneys at the same time. As a complex and potentially aggressive disease, patients need to have a thorough understanding of its causes and risk factors, symptoms, diagnosis, treatment approaches, and other aspects related to this cancer.
Prevalence and Epidemiology
Renal cell carcinoma is the most common type of kidney cancer in adults, accounting for over 90% of all kidney malignancies. It is a relatively uncommon cancer, making up about 3-4% of all adult cancers. In the United States, it is estimated that there will be around 79,000 new cases of kidney and renal pelvis cancer diagnosed in 2023, resulting in over 13,000 deaths. Globally, the incidence of RCC has been steadily increasing, with an estimated 403,000 new cases and 175,000 deaths worldwide in 2020. RCC is slightly more common in men than women, with a male-to-female ratio of approximately 1.5:1.
A short video from Osmosis.org explaining Renal cell carcinoma
Causes and Risk Factors
The exact causes of RCC are not entirely clear, but several well-established risk factors have been identified through epidemiological studies.
- Smoking: Tobacco smoking is considered the most significant modifiable risk factor for renal cell carcinoma. Smokers have a 1.5- to 2-fold increased risk of developing renal cell carcinoma compared to non-smokers, and the risk appears to be dose-dependent, with heavier smokers at greater risk. The carcinogenic compounds in tobacco smoke are believed to contribute to the development of renal cell carcinoma through various mechanisms, including DNA damage, oxidative stress, and inflammation.
- Sex: Men are 2 to 3 times more likely to develop kidney cancer than women.
- Race: Black people have higher rates of kidney cancer4.
- Obesity: Excess body weight, as measured by a high body mass index (BMI), is another major risk factor for RCC. Numerous studies have consistently shown that individuals with obesity have a 1.5- to 2-fold higher risk of developing RCC compared to those with a normal BMI. The underlying mechanisms may involve obesity-related metabolic alterations, such as insulin resistance, chronic inflammation, and hormonal imbalances, which can promote tumor growth and progression4.
- Hypertension: High blood pressure, or hypertension, has been associated with an increased risk of RCC. Individuals with hypertension have a 1.5- to 2-fold higher risk of developing renal cell carcinoma compared to those with normal blood pressure. The exact pathways linking hypertension to RCC are not fully understood but may involve factors such as oxidative stress, endothelial dysfunction, and alterations in the renin-angiotensin system.
- Chronic Kidney Disease: Patients with chronic kidney disease (CKD), particularly those on dialysis, have an elevated risk of developing RCC. The incidence of RCC is estimated to be 2- to 4-fold higher in individuals with CKD compared to the general population. The chronic inflammation, oxidative stress, and altered immune function associated with CKD may contribute to the increased risk of RCC in this population.
- Occupational Exposures: Certain occupational exposures have been linked to an increased risk of RCC, including exposure to trichloroethylene (a common industrial solvent), asbestos, and cadmium. These exposures may lead to cellular damage and genetic alterations that can promote the development of RCC.
- Overuse of certain medications: Painkillers containing phenacetin have been banned in the United States since 1983 because of their link to transitional cell carcinoma.
- Genetic Factors: Inherited genetic conditions, such as von Hippel-Lindau (VHL) disease, hereditary papillary renal cell carcinoma, and Birt-Hogg-Dubé syndrome, are associated with an increased risk of developing RCC. These genetic syndromes are relatively rare, accounting for only 2-3% of all RCC cases, but they provide valuable insights into the molecular pathways involved in the development of the disease.
Symptoms
In the early stages, RCC is often asymptomatic, and many tumors are discovered incidentally during imaging studies performed for other medical conditions. However, as the disease progresses, patients may develop a variety of symptoms, including:
- Hematuria (blood in the urine): This is one of the most common symptoms of RCC, occurring in up to 60% of patients. The presence of blood in the urine can be either visible (gross hematuria) or detected only through laboratory testing (microscopic hematuria).
- Flank or abdominal pain: Dull, aching pain in the flank or abdominal region may be experienced by some patients, particularly those with larger or more advanced tumors.
- Palpable abdominal mass: In some cases, a solid mass or lump can be felt in the abdomen during a physical examination.
- Weight loss: Unexplained weight loss, often accompanied by a loss of appetite, can be a symptom of RCC, especially in more advanced cases.
- Fatigue and malaise: Patients may experience general feelings of tiredness, weakness, and lack of energy, which can be related to cancer or associated paraneoplastic syndromes.
- Fever: Some patients with RCC may experience intermittent or persistent fever, which can be a sign of an underlying inflammatory response or paraneoplastic syndrome.
- Edema: Swelling, particularly in the legs or abdomen, can occur in some RCC patients, often due to the obstruction of blood vessels or lymphatic drainage.
- Anemia: In some cases, iron deficiency anemia can be the presenting feature of RCC, even in the absence of other typical symptoms like hematuria, flank pain, or abdominal mass.
It is important to note that these symptoms do not necessarily indicate the presence of RCC, as they can also be associated with other medical conditions. Therefore, a comprehensive medical evaluation, including diagnostic imaging and, in some cases, biopsy, is essential for the accurate diagnosis of RCC.
Diagnosis
The diagnosis of RCC typically involves a combination of imaging studies and, in some cases, biopsy.
Imaging Studies
Imaging plays a crucial role in the diagnosis and staging of RCC. The primary imaging modalities used include:
- Computed Tomography (CT) Scan:
- CT scan is the most commonly used imaging technique for the evaluation of suspected RCC.
- It provides detailed information about the size, location, and characteristics of the tumor, as well as the presence of any metastatic disease.
- CT scans can help differentiate RCC from other types of kidney masses, such as benign cysts or other renal tumors.
- Intravenous contrast is typically used to enhance the visualization of the tumor and surrounding structures.
- Magnetic Resonance Imaging (MRI):
- MRI can be useful in cases where CT imaging is inconclusive or when there is a concern about the involvement of surrounding structures, such as the renal vein or inferior vena cava.
- MRI can provide additional information about the tumor’s relationship to nearby blood vessels and organs, which can be important for surgical planning.
- MRI is particularly helpful in evaluating the extent of venous involvement, which is a critical factor in determining the appropriate treatment approach.
- Ultrasound:
- Abdominal ultrasound can be a useful initial screening tool for the detection of kidney masses.
- It is a non-invasive and relatively inexpensive imaging modality that can help identify the presence of a kidney tumor.
- However, ultrasound is generally less accurate than CT or MRI in characterizing the tumor and determining its extent.
Biopsy
In some cases, a percutaneous needle biopsy may be performed to obtain a tissue sample for histological analysis and confirm the diagnosis of RCC. Biopsy is typically reserved for situations where the imaging findings are inconclusive or when the information is needed to guide treatment decisions. The biopsy procedure involves the insertion of a thin needle through the skin and into the kidney tumor under the guidance of imaging, such as CT or ultrasound. A pathologist then examines the tissue sample obtained to determine the histological subtype of the RCC. Biopsy may be considered in the following scenarios:
- When the imaging findings are atypical or inconclusive, additional information is needed to confirm the diagnosis.
- When the patient is not a candidate for immediate surgical treatment, the biopsy results can help guide the selection of appropriate systemic therapy.
- When there is a concern about the possibility of a non-RCC tumor, such as lymphoma or metastatic disease, a biopsy is needed to establish the diagnosis.
It is important to note that biopsy is not routinely performed for all patients with suspected RCC, as the risks, such as bleeding or infection, may outweigh the benefits in some cases. The decision to perform a biopsy is made on an individual basis, taking into account the patient’s clinical presentation, imaging findings, and the potential impact on the treatment plan. Once the diagnosis of RCC is established through imaging and, if necessary, biopsy, further evaluation and staging are required to determine the appropriate treatment approach.

Renal cell carcinoma (gross pathology). This image is taken from radiopaedia.org.
Staging and Histological Subtypes
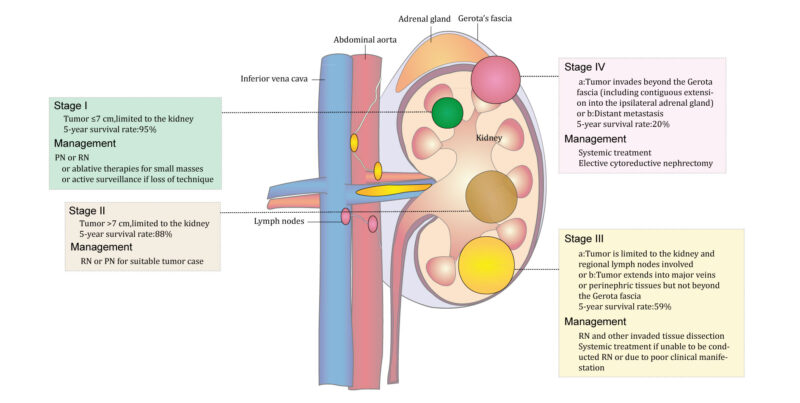
The staging of renal cell carcinoma is based on the TNM (Tumor, Node, Metastasis) classification system, which considers the size and extent of the primary tumor (T), the involvement of nearby lymph nodes (N), and the presence of distant metastases (M). The stage of the disease is a critical factor in determining the prognosis and guiding treatment decisions. The stages of RCC are as follows:
- Stage I: The tumor is 7 cm or smaller and is confined to the kidney.
- Stage II: The tumor is larger than 7 cm but is still confined to the kidney.
- Stage III: The tumor has grown into the major veins or surrounding tissues, and/or has spread to nearby lymph nodes.
- Stage IV: The tumor has spread to other organs, such as the lungs, liver, or bones, or has grown into the adrenal gland.
In addition to staging, the histological subtype of RCC is also an important factor in determining prognosis and treatment. The most common subtypes of RCC include:
- Clear cell RCC: This is the most common subtype, accounting for 70-80% of all RCC cases. Clear cell RCC is characterized by the presence of clear, glycogen-rich cells and is generally associated with a more aggressive clinical course.
- Papillary RCC: Papillary RCC accounts for 10-15% of RCC cases and is further divided into type 1 and type 2 subtypes, which have different genetic and clinical characteristics.
- Chromophobe RCC: Chromophobe RCC makes up 5-10% of RCC cases and is typically less aggressive than clear cell RCC.
- Collecting duct RCC: This is a rare and highly aggressive subtype, accounting for less than 1% of RCC cases.
- Unclassified RCC: A small percentage of renal cell carcinoma cases (5-10%) do not fit into the above-mentioned subtypes and are classified as unclassified RCC.
The histological subtype, along with the stage of the disease, plays a crucial role in determining the prognosis and guiding the most appropriate treatment approach for each patient.
This image is taken from auo.asmepress.com.
Treatment
The treatment of renal cell carcinoma depends on the stage and histological subtype of the disease, as well as the patient’s overall health and preferences. The main treatment modalities for renal cell carcinoma include:
- Surgery:
- Partial nephrectomy: This procedure involves the removal of the tumor and a small portion of the surrounding healthy kidney tissue. It is the preferred treatment for small, localized tumors (stage I or II) and is associated with a lower risk of chronic kidney disease compared to radical nephrectomy.
- Radical nephrectomy: This involves the removal of the entire kidney, along with the adrenal gland and surrounding lymph nodes. Radical nephrectomy is typically recommended for larger tumors or those that have grown into surrounding tissues or blood vessels (stage III or IV).
- Targeted Therapies:
- Tyrosine kinase inhibitors (TKIs): These targeted drugs, such as sunitinib, pazopanib, and cabozantinib, are commonly used to treat advanced or metastatic renal cell carcinoma. TKIs work by inhibiting the activity of specific proteins involved in tumor growth and angiogenesis.
- mTOR inhibitors: Drugs like everolimus and temsirolimus that target the mammalian target of rapamycin (mTOR) pathway are also used to treat advanced or metastatic RCC.
- Immunotherapies:
- Checkpoint inhibitors: These immunotherapeutic agents, such as nivolumab and pembrolizumab, work by blocking the interaction between specific proteins (e.g., PD-1, PD-L1) that can suppress the immune system’s ability to recognize and attack cancer cells.
- Cytokine therapies: Interleukin-2 (IL-2) and interferon-alpha (IFN-α) are cytokines that can stimulate the immune system to attack renal cell carcinoma cells, although their use has declined with the advent of more targeted and effective immunotherapies.
- Radiation Therapy:
- External beam radiation therapy: This may be used in certain cases, such as to alleviate symptoms from metastatic lesions or to treat inoperable primary tumors.
- Ablative Therapies:
- Cryoablation: This procedure uses extreme cold to destroy the tumor, and it may be an option for small, localized tumors in patients who are not candidates for surgery.
- Radiofrequency ablation: This technique uses heat generated by radiofrequency energy to destroy the tumor.
The choice of treatment approach depends on various factors, including the stage and histological subtype of the RCC, the patient’s overall health and preferences, and the availability of specific therapies. In many cases, a multidisciplinary team of healthcare providers, including urologists, medical oncologists, and radiation oncologists, collaborates to develop the most appropriate treatment plan for each patient.
In this video, the results of a clinical trial elucidating the outcomes of patients with advanced renal-cell carcinoma who were randomized to receive either nivolumab plus ipilimumab or sunitinib were presented. Video from NEJM.com
Prognosis and Survival
The prognosis for patients with RCC can vary significantly depending on the stage of the disease at the time of diagnosis. The anatomic extent of the disease, as determined by the TNM staging system, is the most consistent factor that influences prognosis in RCC patients.
The 5-year relative survival rates for RCC in the United States are as follows:
- Stage I: 93%
- Stage II: 88%
- Stage III: 72%
- Stage IV: 12%
These survival rates highlight the importance of early detection and treatment of RCC. Patients with localized, early-stage disease (stages I and II) have a much better prognosis compared to those with advanced, metastatic disease (stage IV).
In addition to stage, other factors that can influence the prognosis of RCC include:
- Histological Subtype:
- Clear cell RCC, the most common subtype, is generally associated with a more aggressive clinical course compared to other subtypes like papillary and chromophobe RCC.
- Genetic Alterations:
- Certain genetic mutations, such as those in the BAP1 and PBRM1 genes, are independent prognostic factors for tumor recurrence and survival.
- Degree of Anemia:
- More severe anemia (hemoglobin <10 g/dL) has been associated with worse overall survival in RCC patients compared to those with mild or no anemia.
- Other Prognostic Factors:
- Factors like tumor size, Fuhrman nuclear grade, presence of sarcomatoid differentiation, and various laboratory parameters (e.g., neutrophil-to-lymphocyte ratio, and platelet count) have also been identified as prognostic indicators in renal cell carcinoma.
Patient’s Survivorship
The treatment for RCC has improved dramatically over the past half-century, leading to high survival rates. However, patients may face a range of problems or side effects during and after treatment, which require careful management and follow-up. These side effects can include cardiac toxicity, neurotoxicity, bone toxicity, hepatic dysfunction, visual changes, obesity, impact on fertility, and neurocognitive effects. It is essential to monitor and manage these side effects to ensure the best possible outcome for the patient.
Problems During Treatment
- Anemia and its Impact on Prognosis:
- Severe anemia (hemoglobin <10 g/dL) has been associated with worse overall survival in RCC patients compared to those with mild or no anemia.
- The degree of anemia can be an important prognostic factor that can impact a patient’s survivorship during their treatment.
- Resistance to Targeted Therapies:
- One of the major challenges in the treatment of metastatic renal cell carcinoma is overcoming drug resistance to targeted therapies, such as tyrosine kinase inhibitors.
- Patients may initially respond to these targeted agents but can develop resistance over time, leading to disease progression.
- Toxicity and Side Effects of Treatments:
- While targeted therapies have improved outcomes for patients with metastatic RCC, these treatments can also be associated with substantial toxicity.
- Patients may need to navigate the management of treatment-related side effects, which can impact their quality of life and ability to continue therapy.
- Access to Emerging Therapies:
- Patients may face challenges in accessing emerging RCC treatments, such as novel combinations of targeted therapies and immunotherapies, depending on factors like insurance coverage, clinical trial availability, and geographic location.
Strategies to Manage Challenges
- Proactive Management of Anemia:
- Closely monitoring and managing anemia, potentially through the use of erythropoiesis-stimulating agents or iron supplementation, may help mitigate its negative impact on prognosis.
- Combination Therapy Approaches:
- Exploring the use of combination therapies, such as the integration of targeted agents and immunotherapies, may help overcome resistance and improve outcomes for patients with advanced RCC.
- Proactive Management of Treatment-Related Toxicity:
- Implementing strategies to actively manage and mitigate the side effects of RCC treatments, such as dose modifications, supportive care interventions, and close monitoring, can help patients better tolerate and adhere to their prescribed therapies.
- Advocacy and Access to Emerging Therapies:
- Patients and their healthcare providers can explore options to access emerging RCC treatments, such as participating in clinical trials or advocating for insurance coverage of novel therapies.
Problems After Treatment
- Recurrence and Metastatic Disease:
- Despite initial treatment, a significant proportion of RCC patients will experience disease recurrence or develop metastatic disease.
- The stage and grade of renal cell carcinoma were independent predictors of recurrence at earlier time points (up to 4 years).
- However, at 5 years post-surgery, the stage and grade were no longer significant predictors of recurrence.
- Other factors like renal vein invasion, tumor size >7 cm, and urinary collecting system invasion were also associated with higher recurrence rates.
- Long-Term Toxicity and Side Effects:
- While targeted therapies have improved outcomes for patients with metastatic RCC, these treatments can also be associated with substantial long-term toxicity.
- Patients may need to manage persistent side effects, such as fatigue, hypertension, and hand-foot syndrome, which can impact their quality of life.
- Psychological and Emotional Challenges:
- The fear of recurrence, the burden of ongoing monitoring and follow-up, and the emotional toll of managing a chronic, potentially life-threatening condition can be significant challenges for RCC survivors.
- Patients may struggle with anxiety, depression, and the impact of the disease on their personal and professional lives.
- Rehabilitation and Functional Impairment:
- Depending on the treatment received, some RCC patients may experience functional impairments, such as reduced kidney function or physical limitations, which can affect their daily activities and quality of life.
- Patients may need to navigate rehabilitation and adaptive strategies to regain or maintain their physical and cognitive abilities.
- Financial and Practical Challenges:
- The ongoing costs of medical care, including follow-up visits, diagnostic tests, and potentially long-term therapies, can be a significant burden for RCC survivors.
- Patients may face challenges with insurance coverage, employment, and managing the practical aspects of their care.
Strategies to Manage Challenges
- Close Monitoring and Early Intervention:
- Regular follow-up with the healthcare team, including frequent imaging and laboratory tests, can help detect disease recurrence or progression early, allowing for timely intervention and management.
- Proactive Management of Long-Term Toxicity:
- Implementing strategies to actively manage and mitigate the long-term side effects of renal cell carcinoma treatments, such as dose modifications, supportive care interventions, and lifestyle changes, can help patients better maintain their quality of life.
- Psychological and Emotional Support:
- Accessing resources like counseling, support groups, and mental health professionals can help RCC survivors cope with the psychological and emotional challenges of their disease and treatment.
- Rehabilitation and Adaptive Strategies:
- Engaging in rehabilitation programs, such as physical therapy or occupational therapy, can help RCC patients regain or maintain their functional abilities and independence.
- Financial and Practical Assistance:
- Exploring resources like patient assistance programs, financial counseling, and community-based support services can help renal cell carcinoma survivors manage the practical and financial challenges of their care.
In this video, Annamarya shared her experience with renal cell carcinoma.
Conclusion
Despite the challenges of managing RCC, there are reasons for optimism. Advancements in treatment and care have significantly improved outcomes and quality of life. Surgical techniques now allow many patients to preserve kidney function. Targeted therapies and immunotherapies have transformed the management of advanced disease. And healthcare teams are taking a more personalized, patient-centered approach. While challenges remain, the future for those diagnosed with renal cell carcinoma is bright. With continued innovation and a steadfast commitment to addressing the unique needs of each individual, there is every reason for patients to be encouraged.
In this video prepared by the National Kidney Foundation, surgical approaches for kidney cancer were presented.
Resources
- National Cancer Institute – cancer.gov
- American Cancer Society – cancer.org
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Memorial Sloan Kettering Cancer Center – mskcc.org
- Clinicaltrials.gov
- National Kidney Foundation – Kidney.org
- Oncodaily.com
- American Family Physician – aafp.org
- How to Treat Renal Cell Carcinoma – PubMed
- Nebraska Hematology Oncology – yourcancercare.com
- Emerging Therapies for Advanced Clear Cell Renal Cell Carcinoma – PubMed
- Renal toxicity of targeted therapies for renal cell carcinoma in patients with normal and impaired kidney function – PubMed
- The Lancet Oncology – thelancet.com
- Scientific reports – nature.com
- Immunotherapy in Renal Cell Carcinoma: The Future Is Now – PubMed
- ASCO Publications – ascopubs.org