The first week of February opens with a particularly rich set of updates across GI Oncology, highlighting how the field continues to advance at the intersection of translational science, biomarker-driven decision-making, and evolving therapeutic strategies.
This week’s must-read posts span the full continuum of gastrointestinal cancer research and care—from adjuvant treatment optimization in rare GI tumors and later-line strategies in metastatic colorectal cancer, to regulatory progress in cholangiocarcinoma, emerging radiotherapy paradigms in hepatocellular carcinoma, and advances in liquid biopsy technologies. Several contributions emphasize the growing role of ctDNA, transcriptomic and methylome-based frameworks, and machine learning models in refining patient selection, monitoring treatment response, and guiding clinical trial design.
Together, these studies and expert insights illustrate how early February is shaping a more precise, data-driven, and biology-informed era in GI Oncology—where clinical decisions are increasingly supported by integrative molecular profiling, innovative computational tools, and collaborative translational research.
Nelson Dusetti – Research Director, INSERM | Pancreatic Cancer & Translational Oncology | Co-founder of Predicting Med, developing transcriptomic tools for precision oncology
“Pleased to share the publication of the design of the phase III PRODIGE 98 – AMPIRINOX trial in resected ampullary adenocarcinoma, a rare epithelial digestive cancer where the optimal adjuvant strategy remains debated.
Beyond clinical outcomes, this study integrates an extensive translational program combining pathology, genomics and transcriptomics to better understand tumor subtypes and treatment response.
Our contribution is articulated through OncoSignView, a cross-tumor transcriptomic framework dedicated to transferring and refining chemotherapy-response signatures across epithelial cancers.
Starting from PancreasView, originally developed for PDAC treatment-response prediction, we aim to evaluate how predictive transcriptomic patterns can be extended beyond pancreatic cancer to other epithelial gastrointestinal tumors treated with FOLFIRINOX or gemcitabine-based regimens, while explicitly accounting for both epithelial and stromal composition.
This is not a fixed model but an ongoing scientific exploration, moving predictive signatures from one tumor context to another to approach a more organ-agnostic precision oncology grounded in biology and data.
A truly collective effort bridging clinical oncology, molecular pathology and machine-learning-driven translational research.”
Vincenzo De Falco – MD, Medical Oncologist, PhD
“I am pleased to share the publication of our latest study reporting the clinical and translational results of the phase II ABACO trial, evaluating cabozantinib in pretreated patients with metastatic colorectal cancer.
In a heavily pretreated mCRC population, we combined clinical outcomes with translational analyses to better characterize the activity of multi-target tyrosine kinase inhibition and explore potential biological correlates of response.
These findings add to the growing body of evidence supporting novel therapeutic strategies for patients with limited treatment options and highlight the value of integrating clinical and molecular data in advanced colorectal cancer.”
Juan W. Valle, MB ChB MSc FRCP – Chief Medical Officer at Cholangiocarcinoma Foundation
“Great news for the end of the week! Partner Therapeutics, Inc. announced that the FDA and has granted Orphan Drug Designation to zenocutuzumab-zbco for the treatment of adults with advanced unresectable or metastatic cholangiocarcinoma.
Patients with cholangiocarcinoma face a particularly aggressive cancer with a poor prognosis and limited treatment options. Receiving Orphan Drug Designation for zenocutuzumab in patients with CCA harboring the NRG1 gene fusion is a significant regulatory milestone for Partner Therapeutics and highlights the urgent need for new and effective treatment options for patients with this disease.”
Read about Zenocutuzumab‑zbco Secures FDA Orphan Drug Designation in NRG1 Fusion–Positive Cholangiocarcinoma on OncoDaily.
Davide Ciardiello – Oncologo presso Divisione Oncologia Medica Tumori Gastrointestinali e Neuroendocrini, IEO, Istituto Europeo di Oncologia
“How does anti-EGFR rechallenge strategy compares with SoC as later line therapy in mCRC?
Ti answer to this question we conducted a systematic review and meta-analysis.
-anti-EGFR rechallenge led to higher ORR, DCR and PFS compares with SoC (mainly regorafenib or trifluridine/tipiracil) in patients with ctDNA RAS/BRAF wt tumors.
-No difference in OS was observed due to crossover.
The ROMANCE trial will compare cetuximab+irinotecan rechallenge vs trifluridine/tipiracil+bevacizumab as third-line therapy in patients with ctDNA “negative hyperselected”mCRC (NCT07381764).”
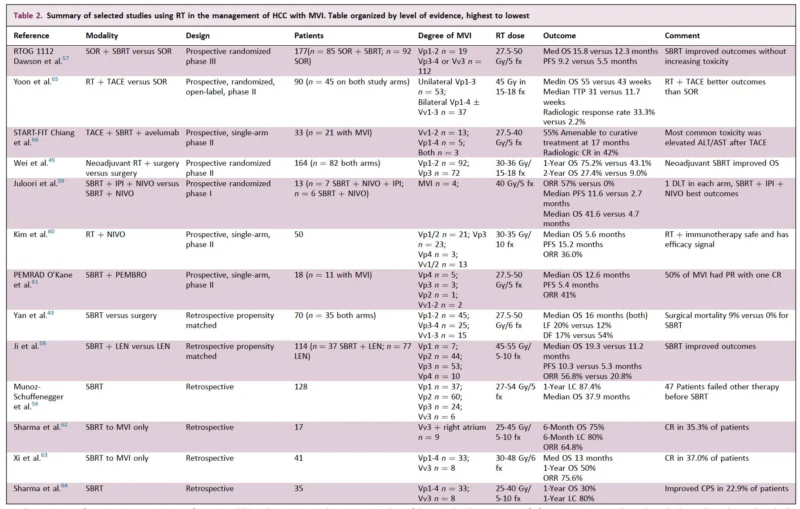
Arndt Vogel – Clinician-Scientist, ESMO Ambassador, focussed on Liver Cancer & Precision Oncology, Toronto General Hospital/Princess Margaret Cancer Center
“The role of stereotactic body radiotherapy in the management of HCC with macroscopic vascular invasion: a narrative review.
SBRT emerges as a crucial tool in the multidisciplinary management of HCC and has the potential to enhance systemic therapy efficacy”
Matteo Benelli – Associate Professor, University of Florence
“I’m very happy to share our recent publications on METER (DNA-METhylome AnalysER), a unified computational framework that enables:
– ctDNA detection (METER-detect)
– Tumor fraction quantification (METER-quant)
– Molecular subtyping (METER-subtype)from low-pass (0.5–1x) whole-methylome sequencing of plasma cell-free DNA, within a single integrated pipeline.
This work is the result of years of development and validation, led by the brilliant marta paoli, and developed in collaboration with Francesca Demichelis.
In the study published in Genome Medicine (Springer Nature), we introduced METER and, together with laura biganzoli (Medical Oncology) and Luca Malorni (Translational Research Unit, thanks to the super Francesca Galardi and Agostina Nardone) at the Hospital of Prato, applied it to longitudinal plasma samples from two independent cohorts of patients with metastatic breast cancer. We show that METER:
– Enhances sensitivity for ctDNA detection, enabling disease monitoring in challenging low–tumor fraction settings
– METER-detect, the module for classifying samples as ctDNA pos vs neg, shows a strong association with clinical outcomes, outperforming state-of-the-art approaches and matched CTC counts
– Enables non-invasive ER status subtyping with 94% accuracy, supporting monitoring of tumor phenotypeFurthermore, in collaboration with Filippo Pietrantonio, we demonstrated METER’s generalizability to colorectal cancer. In the study co-led by Paolo Manca and published in Clinical Cancer Research (AACR Journals), we leveraged METER to evaluate baseline and on-treatment ctDNA dynamics in patients with metastatic colorectal cancer from the VALENTINO trial, showing that METER can effectively complement radiologic assessment of treatment response.
METER is open-source and coupled with low-pass methylome is designed to be a practical, robust, and cost-effective tool for ctDNA analysis and longitudinal monitoring.”
Signe Bülow Therkildsen – PhD student, UNICCA University Clinic for Cancer Screening
“The qualitative study from my PhD project OPTIMZED-FIT is now published
Study Title: “Attitudes and information-needs towards a risk-based optimization of colorectal cancer screening among Danish citizens: a qualitative study”
In collaboration with my supervisors, Berit Andersen and Camilla Rahr Tatari
we explored Danish citizens’ attitudes towards a risk-based optimization of the national colorectal cancer screening program. Overall, attitudes were positive when changes were clinically justified. Shorter screening intervals for higher-risk individuals were perceived as both concerning and reassuring, while longer intervals for lower-risk individuals were generally seen as reassuring.
Most participants reported limited information needs, although some preferred access to personal contact. Our findings suggest that risk-based screening is acceptable to citizens and may be implemented without major changes to existing information materials.”
Erman Akkus – MD, medical oncology, internal medicine, Ankara University; sharing and discussing on cancer, GI oncology
“Do we need a germline genetic testing in HCC?
I presented our study in 2nd International Hereditary Cancers Congress
We analyzed somatic driver mutations of hereditary cancer genes in HCC
- 372 patients, 25% diagnosed <50y
- 438 driver mutations in 77 genes
- 70% of mutations VAF > 30%
- 34% had VAF>50%
Do we neglect a possible germline predisposition in HCC?
More germline data and target population definitions are required”
Noelia Tarazona, MD, PhD – Research Fellow at Mass General Brigham Cancer Center
“Happy to share our latest work from Mass General Brigham, led by Aparna Parikh.
In MSS metastatic colorectal cancer, liver metastases really matter: patients without liver involvement had markedly better outcomes with ICIs, both in PFS and OS.
Important implications for patient selection and trial design. ”
Rami Rhaiem – Surgeon, HPB and digestive surgery department
“We are pleased to share the results of our new multicenter French collaborative study, recently published in Liver Cancer, focusing on machine learning–based prediction of disease-free survival (DFS) after liver resection for hepatocellular carcinoma (HCC).
Rationale
Liver resection remains a cornerstone of the curative treatment of HCC, yet postoperative recurrence rates remain high. Accurate and individualized postoperative prognostication remains a key clinical challengeResults
In this study (663 patients from 4 French HPB centers), machine learning–based survival models were developed and externally validated to estimate DFS after liver resection for HCC.
Random Survival Forest (RSF) achieved the highest performance, especially in predicting DFS for up to 36-40 months following LR, effectively capturing complex non-linear relationships.Clinical impact
ML-based survival models can help:
• Identify patients at high risk of early recurrence
• Support MDT discussions
• Refine patient selection for clinical trials evaluating adjuvant treatment versus standard surveillance”

Find out 10 Must-Read Posts in GI Oncology from the last week of January on OncoDaily.