The last week of January brings a particularly rich and multidimensional set of updates across GI Oncology, reflecting how the field continues to evolve at the intersection of biomarker-driven decision-making, therapeutic innovation, and care optimization.
This week’s must-read posts span the full GI spectrum—from ctDNA-guided risk stratification in resected colon cancer to practice-changing data in HER2-positive gastric and BRAFV600E-mutated colorectal cancer—alongside advances in pancreatic cancer biology, medicinal chemistry, and perioperative and supportive care frameworks. Several contributions underscore how molecular context increasingly determines benefit, whether in immunotherapy selection, targeted combinations, or perioperative strategies.
Across these studies and expert insights, a unifying theme emerges: precision in GI Oncology is no longer confined to drug choice alone, but now extends to patient selection, biological enrichment, survivorship interventions, and system-level implementation. Together, these posts capture how late January 2026 is shaping a more nuanced, biology-aware, and execution-focused era of GI cancer care.
Frank Sinicrope, MD – Gastrointestinal Oncologist
“Tissue-Free Circulating Tumor DNA Assay and Patient Outcome in a Phase III Trial of FOLFOX-Based Adjuvant Chemotherapy (Alliance N0147) | Journal of Clinical Oncology
Hot off the press! Largest study of tissue-free ctDNA assay in colon cancer.”
Erman Akkus – Medical Oncologist – GI Oncology
“Anbenitamab + ChT vs ChT in previously trastuzumab-treated HER2+ gastric/GEJ adenocarcinoma (KC-WISE)
mPFS: 7.1 vs 2.7 months
HR: 0.25 (0.17–0.39); p<0.0001mOS: 19.6 vs 11.5 months
HR: 0.29 (0.17–0.50); p<0.0001”
Nelson Dusetti – Research Director, INSERM | Pancreatic Cancer & Translational Oncology | Co-founder of Predicting Med
“Honored to have been invited to the International Biotherapy Days in Toulouse.
I had the pleasure to present PANCProfiler, an integrative framework combining single-cell transcriptomics and patient-derived preclinical models to decipher therapeutic resistance programs in pancreatic cancer.What makes this meeting particularly valuable is the way it brings together academic research, clinical perspectives, and innovation ecosystems, creating a space where mechanistic insights can naturally resonate beyond the laboratory.
Many thanks to the organizing committee for this invitation and the quality of the discussions, and special thanks to my friend Pierre Cordelier for making this possible.”
Giovanni Ferrandi – Postdoctoral Researcher, Universitat Politècnica de Catalunya
“Publication alert!
Check out my first first-author paper in ACS Medicinal Chemistry Letters with my colleagues Greta Bagnolini and Laura Poppi and the various project collaborators. It was a pleasure working with them on this paper. Thank you to everyone involved!”
Daniel Acosta Eyzaguirre – Medical Oncologist and Clinical Researcher, Drug Development; Digestive and Endocrine Tumors Unit (Gastric Cancer), Vall d’Hebron University Hospital; Vall d’Hebron Institute of Oncology (VHIO)
“New insights on CLDN18.2 in gastroesophageal adenocarcinoma!
Just out!Proud to share our multicenter European study (563 patients, 17 institutions) on CLDN18.2 expression in gastroesophageal cancer, now published in ESMO Open.
Key findings worth considering:
We found high CLDN18.2 expression in nearly half of tumors (48%), with substantial overlap across multiple biomarkers (HER2+, PD-L1+, dMMR, EBV+).
Patients with CLDN18.2-high tumors treated with immunotherapy showed a trend toward poorer outcomes, even in the context of PD-L1 positivity.We should ask:
Should we evaluate multiple biomarkers simultaneously before deciding first-line strategy?
Should we reconsider the use of immunotherapy in CLDN18.2-high patients until we have more prospective evidence?
For me it is clear that we should integrate CLDN18.2 into our clinical decision-making algorithms.
As a retrospective study, these findings require prospective validation, but they highlight the need for more tailored therapeutic strategies in GEA.”
Rishabh Jain – Senior Resident, Medical Oncology, AIIMS Delhi
“Exercise is now part of adjuvant colon cancer care. Yes, officially.
ESMO colon cancer guidelines now recommend structured exercise programmes alongside chemotherapy in Stage II (high-risk) and Stage III colon cancer.
This is not lifestyle advice.
This is evidence-based oncology care.Where does exercise fit?
Stage III colon cancer
High-risk Stage II colon cancer
During adjuvant chemotherapy and follow-upStrength of evidence
Level II evidence
Grade B recommendation
MCBS A scoreWhy this matters clinically
Improved disease-free survival
Better treatment tolerance
Reduced fatigue and QoL decline
Lower recurrence signalsKey takeaway
Exercise is no longer optional advice.
It is part of standard adjuvant management in colon cancer.”
Maj-Britt Paulsohn – PhD Candidate, Molecular Oncology
“I am incredibly happy to share our latest publication on combined KRAS and CDK4 inhibition in pancreatic cancer, published at Cell Death & Disease.
Simultaneous targeting of KRAS and CDK4 synergistically induces durable growth arrest in pancreatic cancer cells
I am extremely grateful for all our collaboration partners, who contributed to this project, particularly all KFO5002 members. Thank you to the Hessmann and Schneider labs! And thank you to my supervisor Matthias Dobbelstein.”
Dimitrios Chatziisaak – Doctorat en Médecine (Dr.med.), MSc, MBA (cand.), Junior Member, Swiss College of Surgeons (SCS)
“Honored to share that our abstract and poster on simultaneous pancreas–kidney (SPK) transplantation in recipients with HIV infection were accepted for EPITA 2026 (ESOT – European Society for Organ Transplantation).
Grateful to my co-authors and the transplant team at Guy’s & St. Thomas’ NHS Foundation Trust for the collaboration.
Looking forward to the discussions on how we can continue expanding equitable access to transplantation for complex patient populations.”
Davide Ciardiello – Medical Oncologist, Division of Gastrointestinal and Neuroendocrine Tumors, IEO, Istituto Europeo di Oncologia
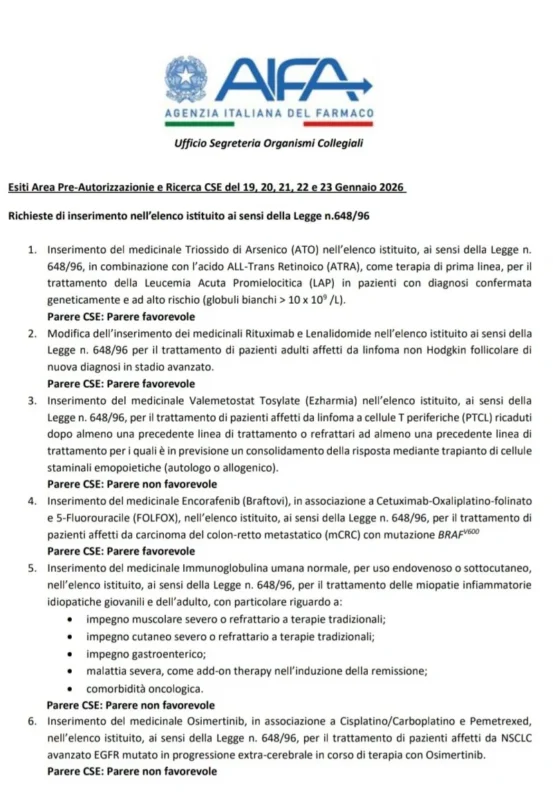
“January 30 will be a date to remember for oncologists who deal with neoplasms of the gastrointestinal tract.
AIFA has just expressed a favourable opinion on the inclusion of the combination encorafenib + cetuximab and FOLFOX in the list established by Law no. 648/96.
The BREAKWATER study (Kopetz et al, NEJM 2025) had shown that this combination is able to double the survival of patients with colorectal BRAFV600E-mutated cancers compared to a standard therapy.
These are incredible results that demonstrate how a molecularly targeted therapy is able to transform the natural history of an extremely aggressive disease.If this was also possible, it was thanks to the request to AIFA carried out by the president of the Oncology Group of Southern Italy (GOIM) Roberto Bordonaro, by the past president Prof. Ferdinando De Vita, and by the president-elect Prof. Fortunato Ciardiello.”
Sarbajit Mukherjee, MD, MS – Chief of GI Medical Oncology
“Who truly benefits from perioperative immunotherapy in gastric and GEJ cancer?
Our latest data suggest the answer is clear: tumor biology matters.I’m excited to share that our team’s meta-analysis has just been published in JNCI Cancer Spectrum, synthesizing evidence from 7 randomized trials and 2,510 patients evaluating perioperative chemo-immunotherapy in resectable gastric/GEJ adenocarcinoma.
Key findings:
• Adding immunotherapy to perioperative chemotherapy improves outcomes overall:
• pCR: 17.6% vs 6.1%
• EFS: HR 0.76
• OS: HR 0.82
However, benefit is biologically enriched:
• PD-L1–positive tumors show consistent improvement in pCR, EFS, and OS
• PD-L1–negative disease demonstrates no statistically significant survival signal at the meta-analysis levelImportantly, these findings align closely with the National Comprehensive Cancer Network (NCCN) guidelines.”

Find out 10 Must-Read Posts in GI Oncology from the fourth week of January on OncoDaily.