The third week of January 2026 brings together a focused and practice-shaping selection of discussions in GI oncology, spanning colorectal, pancreatic, hepatocellular, biliary. This week’s 10 must-read posts integrate clinical trial data, real-world evidence, and translational research, highlighting how progress in GI oncology increasingly depends on precision, context, and patient selection rather than treatment intensification alone.
Across these contributions, a common theme emerges: meaningful advances come from better stratification, biologically informed decisions, and durable benefit, reinforcing a shift toward personalized and rational treatment strategies in contemporary GI oncology.
Nicholas Hornstein – Gastrointestinal Medical Oncologist
“Final analysis of MOUNTAINEER and it’s worth pausing on how big this really was for colorectal cancer.
Before this study, HER2 in CRC was interesting biology with very little clinical payoff. MOUNTAINEER changed that.
This was a chemo-refractory, HER2-positive, RAS wild-type metastatic colorectal cancer population, patients who historically had very few effective options left. A chemotherapy-free, dual HER2 approach with tucatinib plus trastuzumab showed that HER2 is not just present in colorectal cancer, it is actionable.
What stood out
Roughly 4 in 10 patients had meaningful tumor shrinkage
When responses happened, they were durable, often lasting more than a year
Disease control was measured in months, not weeks
Median survival approached two years, something we simply did not see in this setting beforeToxicity pearls and management
Diarrhea was common, usually early, and very manageable with proactive loperamide and dose adjustments
Rash was frequent but typically low grade, acneiform in nature, and manageable with topical steroids, doxycycline, and early dermatology involvement when needed
Fatigue and mild liver function test elevations occurred, but serious toxicity was uncommon
Very few patients discontinued therapy due to side effects and there were no treatment-related deathsTwo other things matter here. First, benefit was seen regardless of how HER2 was identified, tissue or blood, which has real-world implications for testing. Second, the author list is a true who’s who of colorectal cancer, reflecting how much collective effort went into proving this concept.
MOUNTAINEER was the proof-of-principle moment. It showed that HER2 targeting belongs in colorectal cancer and laid the foundation for what comes next, including earlier lines of therapy and smarter sequencing.”
Moawia Mohammed Ali Elhassan – Clinical and Radiation Oncologist
“Less is More: Long-Term SCOT Trial Data Confirms 3 Months of Adjuvant CAPOX as a Standard of Care in Colorectal Cancer (CRC)
The debate on adjuvant chemotherapy duration in patients with high-risk stage II and stage III colorectal cancer takes a definitive step forward with the latest long-term survival results from the SCOT trial, recently published in the Journal of Clinical Oncology.
After a median follow-up of 113 months in over 6,000 patients, the findings reinforce a crucial shift in clinical practice.
Non-inferiority confirmed: 5-year overall survival was identical at 82.4% for both 3-month and 6-month cohorts (HR 0.96; 95% CI 0.8–1.07).
Regimen matters: non-inferiority was robustly demonstrated for CAPOX, whereas data for FOLFOX remained less certain. Even in stage III patients treated with FOLFOX, the group with the largest variance, the absolute overall survival benefit for 6 months was only 2.2%. This yields a number needed to treat of 50 to prevent one death. Conversely, 6 months of therapy more than doubles grade ≥2 peripheral neuropathy (25% to 58%). Effectively, for every death prevented, 15 patients suffer long-lasting, clinically significant impairment.
Quality of life: reducing treatment to 3 months significantly mitigates cumulative peripheral neuropathy and enhances patient quality of life without compromising survival.
Rectal cancer: notably, non-inferiority was also established in the rectal cancer subgroup.
The bottom line:
For most patients with high-risk stage II and stage III colorectal cancer, 3 months of CAPOX should now be considered the standard of care. This ‘less is more’ approach prioritizes patient safety and long-term neurological health while maintaining oncological efficacy.”
Oliver Waidmann – Professor and Partner, Bethanien Center for Hematology and Oncology; Attending Physician, Agaplesion Bethanien Hospital; Head of the FDK Oncology Center, Bethanien Hospital Site
“I am happy to share our data on iRGD which improves PD-L1 treatment in murine HCC models. A potential new treatment concept for human HCC.
Thank you Albrecht Piiper and all collaborators on your ongoing commitment to the project we have started already several years ago.”
Cristina Smolenschi – Medical Oncologist, Comprehensive Cancer Center (CLCC), Gustave Roussy Institute
“The rise in early-onset colorectal cancer is well recognized, but BTC and PDAC are also an important and growing concern. Genetics, obesity, alcohol, smoking, environmental exposures do probably play a role, but the the puzzle remains unsolved, reinforcing the need to continue research to better understand these diseases and find more effective treatment as well as preventive measures.”
Nelson Dusetti – Research Director, INSERM; Pancreatic Cancer and Translational Oncology; Co-founder of Predicting Med, developing transcriptomic tools for precision oncology
“An important topic in pancreatic cancer research. Personalising treatment can no longer rely on a one-size-fits-all approach; it requires a precise understanding of tumour heterogeneity and the development of biological tools that are truly actionable in the clinic.
This SFC webinar will take place on Thursday, February 12, 2026 (6:00–7:00 pm CET). The presentation will be in French and is intended for both scientists and clinicians, bridging biology and clinical practice. CRCM – Centre de Recherche en Cancérologie de Marseille. Institut Paoli-Calmettes.”
Ismail Gögenur – Professor and Senior Consultant, Department of Surgery, Zealand University Hospital; University of Copenhagen
“Proud to share our new paper on identifying colorectal cancer recurrence using Danish national health data registries.
A key message: the best recurrence algorithm is not only the most accurate—it is the most representative.
In many registries (including Denmark), recurrence is not routinely recorded. Existing approaches can unintentionally select ‘healthier’ cohorts by applying pre- or postoperative exclusion criteria—creating selection bias and limiting generalizability.
In this work, we refined an established registry-based algorithm with a clear priority: maximize patient representation in the recurrence cohort while maintaining high performance.
What we changed to improve representativeness and generalizability:
Removed preoperative exclusion criteria
Included patients who died within 180 days after surgery (often excluded, but essential for real-world validity)
Expanded treatment signals (e.g., targeted therapy and radiotherapy codes)
Revised pathology code logic and strengthened recurrence signals across registriesResults (reference: an expanded chart-validated recurrence from electronic health records):
More inclusive cohort: 4,388 vs 3,684 patientsHigh performance retained (and slightly improved):
Sensitivity 0.92 (vs 0.90)
Specificity 0.97 (vs 0.96)Improved alignment in stage-specific recurrence patterns, including UICC stage I, where the refined algorithm reduced discrepant recurrence estimates versus reference.
Why this matters: if we want registry-based studies to inform clinical decisions, health policy, and quality improvement, we must ensure that our recurrence cohorts reflect the full spectrum of patients—not just those who survive long enough or fit narrow criteria.
We are looking forward to demonstrating even improved performance through the use of machine learning algorithms later this year, improving these metrics while preparing to utilize these algorithms to individualize perioperative interventions in the future.”
Giovanni Marchegiani, MD, PhD – Academic Pancreatic Surgeon, Hepato-Pancreato-Biliary (HPB) and Liver Transplant Surgery, Padova University Hospital
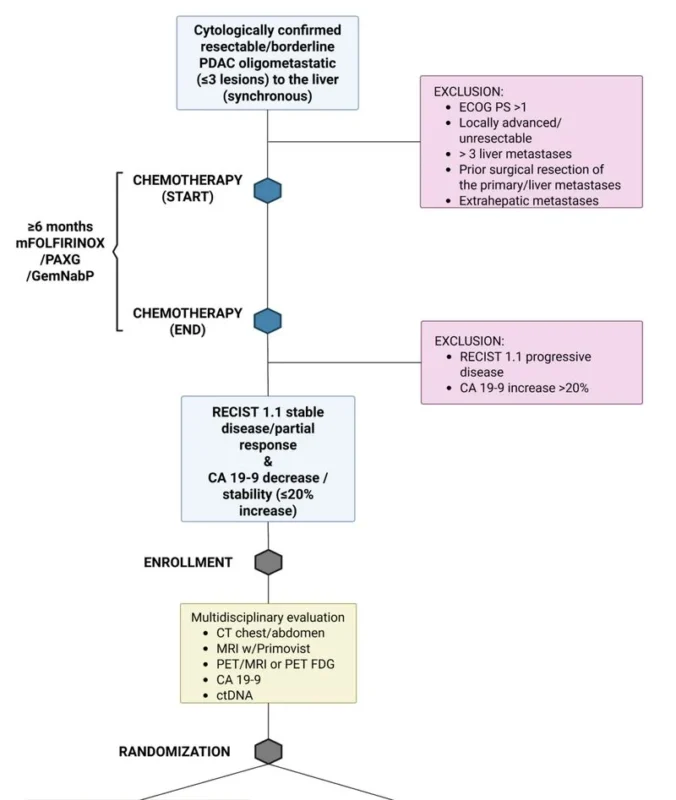
“Oligometastatic pancreas cancer: what’s the best treatment?
The randomized controlled SONAR multicenter study is up and running.
Patients are randomized 1:1 after chemotherapy selection into surgery versus observation or continued chemotherapy.
The protocol is freely available via BMC.”
Akshaya Srikanth, PhD – Cancer Researcher
“I’m pleased to share my second-author publication in the British Journal of Cancer.
Our study, ‘CD44 upregulation in chronic liver disease marks the transition to hepatocellular carcinoma and portends poor prognosis,’ identifies CD44 as a marker associated with disease progression and poor outcomes in liver cancer, providing insights into mechanisms underlying hepatocellular carcinoma development.
Grateful to my co-authors for the excellent collaboration.
Here’s a link to the publication, if you’re interested:”
Erman Akkus – Medical Oncologist, Gastrointestinal Oncology
“SLOG versus Modified FOLFIRINOX as First-Line Treatment for Advanced Pancreatic Cancer: A Randomized Phase II Trial (TCOG T5217) – European Journal of Cancer”
Stefan Salcher – Assistant Professor in Precision Oncology, Department of Internal Medicine V (Hematology and Oncology), Medical University of Innsbruck
“We’re thrilled to announce that our second major paper in Cancer Cell is now out!
In this work, we present a large-scale single-cell atlas of colorectal cancer, provide a precise definition of CRC-associated neutrophils, and map their spatial organization across the tumor microenvironment.”

Find out 10 Must-Read Posts in GI Oncology from the second week of January on OncoDaily.


