Mark Lewis shared on Twitter/X:
“WHY I (ALMOST) NEVER BOLUS 5-FLUOROURACIL
I’ve been pondering this thread for a while but it’s become more urgent in light of another looming chemo shortage <deep sigh>, this time with an imminent dearth of THE foundational drug of GI oncology: 5-fluorouracil, or 5-FU.
An attending of mine from fellowship said “every patient with GI cancer deserves to receive FOLFOX” and, while that may have been a statement of its time (I trained 2009-2012, pre-KEYNOTE 177!) it still has the ring of truth today.
So, while we should ALWAYS be thoughtful prescribers of chemotherapy (primum non nocere, anyone?), if we have a finite supply of 5-FU, and some other cytotoxic drugs are likely only active with a fluoropyrimidine backbone, we should be particularly parsimonious with its use.
In mFOLFOX6 the ambulatory infusion of 5-FU is 2400mg/m2 and the bolus is 400mg/m2 so the bolus comprises ~14% of the entire drug usage (put another way, we can enable 1 extra pump fill for every 6 boluses held).
And while FOLFOX (whether FOLFOX4 or 6) has been the workhorse regimen in mCRC for decades, we have data from the pre-oxaliplatin era (EORTC 40952 and even Moertel in 1972!) that slow(er) infusion had similar activity in the metastatic setting (but could not deduce additive effect).
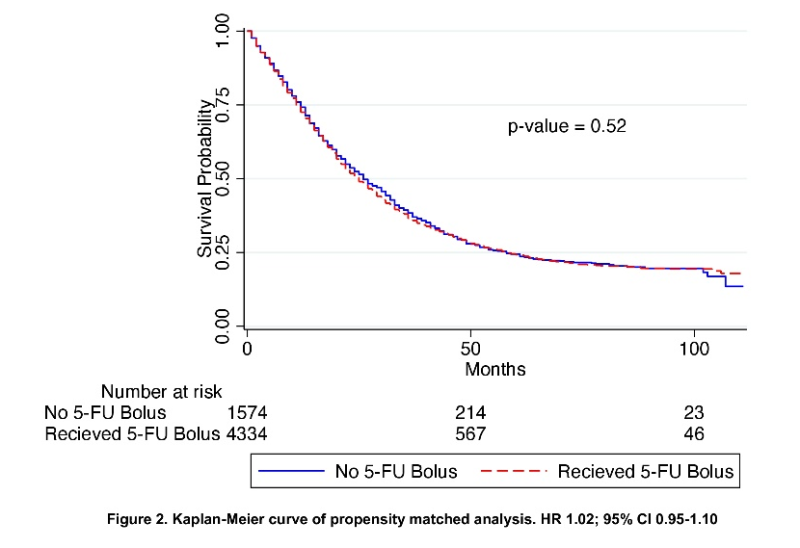
Much more recently, the abstract below caught my eye at ASCO GI earlier this year (GI23) “The use of a 5-FU bolus was not associated with OS (HR 0.98; 95% CI 0.91-1.06; p = 0.64).” You can’t fit a laser pointer between these survival curves. See more here:
And while it didn’t demonstrate any benefit for concurrent infusion of calcium/magnesium salts with oxaliplatin to mitigate CIPN CONcePT (corroborated by CRAFT) showed that mFOLFOX7 could reduce the incidence and severity of neutropenia (grade 3/4 ≤ 20%). See more here:
I’m no oncologic pharmacist but have always wondered how to correlate serum concentration of 5-FU with cytotoxic effect given the need for intracellular incorporation –> inhibition of thymidylate synthase –> FdUMP –> DNA damage (the bolus is thought to act on RNA synthesis).
Stated more simply, why bolus a drug over 15 minutes that is then going to be in circulation for at least 46+ hours? (You also, in theory, don’t need leucovorin to lengthen the half-life of bolus 5-FU if infusion alone is being used). Read more here:
OK, if that’s the metastatic setting (where, without succumbing to therapeutic nihilism, we are seldom treating with curative intent), what about the adjuvant context? Here I need to get on a soapbox about the IDEA trial and our sloth in implementing it in practice.
It’s taking longer than you might expect/hope (at least in the US, our Dutch colleagues have been faster) for prescribing patterns to change (the dashed lines below are ASCO plenary in 2017 and the manuscript publication in 2018). Read more here:
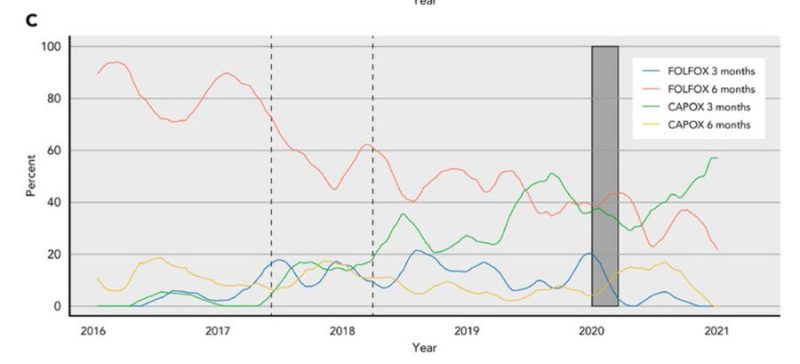
Even with COVID-19 potentially hastening more CAPOX use (conjecturing the relative attractiveness of fewer oxali infusions) I still don’t think we are using enough CAPOX in the low-risk (i.e. T3N1) risk stratum.
And, back to the crux of this thread, using more cape saves 5-FU!
This graph blew my mind at ASCO17. If the litmus test of a meaningful conference is that it changes your practice then this was a resounding YES. I became much more likely to truncate adjuvant courses for low-risk stage III colon cancer cases to 3 months, and also to use CAPOX.
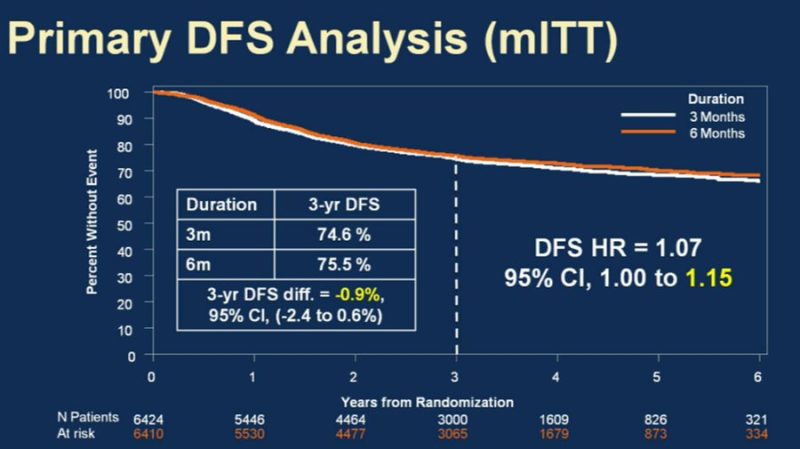
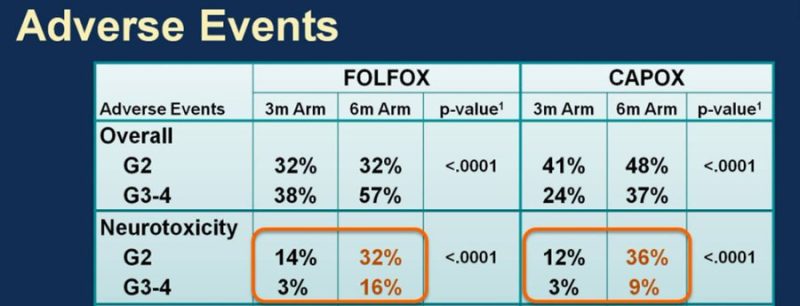
And re: the CIPN risk, this is how I distill it down, hopefully not too reductively or condescendingly for patients: “for a 1% greater chance of being alive without cancer in 3 years, would you be willing to incur triple the risk of severe nerve damage?” (sum G2+: 15% –> 45%).
Finally, when DO I bolus 5-FU then? If I’m legitimately concerned about coronary vasospasm then I deploy the Roswell Park regimen, as the phenomenon appears schedule-dependent (also shoutout cardio-onc, vital partners in such multidisciplinary calculus!). Read more here:
In summary:
1) ask what the 5FU bolus is adding (or not) to your GI onc regimens and if you can possibly omit it
2) ask, relatedly, if leucovorin is needed
3) consider capecitabine when appropriate and don’t forget IDEA’s risk strata/durations
4) talk to your pharmacists”
Source: Mark Lewis/Twitter
Mark A. Lewis is the Director of Gastrointestinal Oncology at Intermountain Healthcare in Utah, the Co-Chair of adolescent and young adult (AYA) oncology in the SWOG cooperative group, and the Vice President of American Multiple Endocrine Neoplasia Support. Dr. Lewis is also a well-known patient advocate and social media influencer.


