The “Morning with the Masters – How Do I Manage Common Cardiovascular Toxicities in Cancer Patients” session at the Global Cardio-Oncology Summit (GCOS) 2025 brought together leading experts to discuss practical management of common cardiovascular toxicities in oncology.
The session featured Dr. Ninian Lang (Scotland) on arterial hypertension and Dr. Chris Plummer (UK) on QTc prolongation – two critical yet often under-recognized challenges in cancer care.
Arterial Hypertension in Cancer Patients – Dr. Ninian Lang
Dr. Lang opened with a central question:
“At what level does blood pressure become harmful in cancer patients?”
While robust randomized data in oncology populations are limited, evidence clearly links elevated blood pressure at diagnosis with worse long-term outcomes.
Systolic blood pressure above 140 mmHg have a twofold increased risk of late heart failure, while even modest elevations between 130–140 mmHg increase risk by about 25%.
Hypertension is a common yet often under-recognized cardiovascular risk factor in oncology. Early detection and proactive management – before, during, and after cancer therapy – are critical to optimizing both cardiac and cancer outcomes.
Practical recommendations:
- Aim for <140/90 mmHg in most patients. Consider <130/80 mmHg in younger or fit individuals who tolerate lower pressures.
- For BP >160/100 mmHg, initiate treatment with an ACE inhibitor (ACEi) or angiotensin receptor blocker (ARB) combined with a calcium channel blocker (CCB).
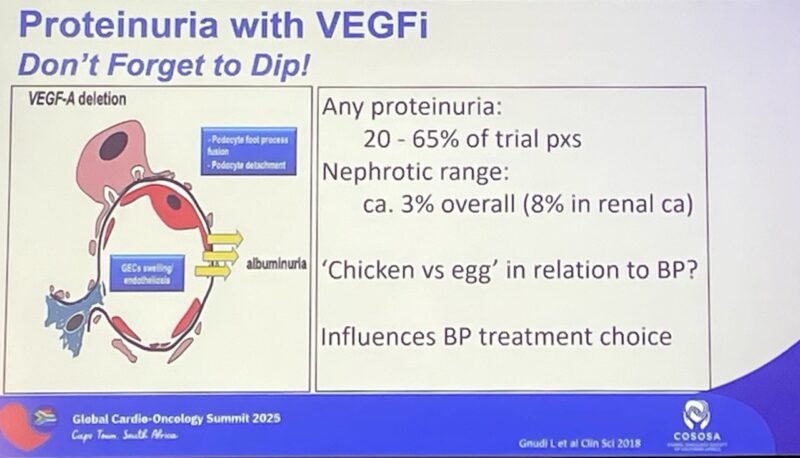
- Recognize that VEGF inhibitors (e.g., sunitinib) can cause rapid and severe hypertension; close home monitoring during treatment initiation is essential.
- Avoid verapamil and diltiazem in patients on VEGF inhibitors due to drug–drug interactions.
- If proteinuria is present, prefer ACEi or ARB over CCBs.
Dr. Lang emphasized a personalized, context-driven approach: treatment decisions should consider cancer stage, prognosis, and therapy type. Ultimately, hypertension management aims to ensure uninterrupted optimal cancer therapy while minimizing cardiovascular risk.
QTc Prolongation – Dr. Chris Plummer
Dr. Plummer tackled the complex topic of QT interval prolongation, which can predispose patients to potentially fatal arrhythmias such as torsades de pointes. He highlighted that despite widespread awareness, uncertainty remains around accurate measurement, risk interpretation, and real-world management.
The QT interval represents the time for ventricular depolarization and repolarization. When prolonged, it creates electrical instability that can trigger arrhythmias. Accurate measurement remains a challenge. Automated ECG readings often over- or underestimate QTc, so manual verification is essential.
Clinicians should measure across visible leads, use the longest QT, and apply the Fridericia correction formula, which is less dependent on heart rate than Bazett’s. Leads with U-waves should be avoided where possible, or analyzed using the tangent method if unavoidable.
Typical QTc values are considered <450 ms in men and <470 ms in women, but up to 10% of healthy individuals fall outside these limits, emphasizing the need for individualized interpretation rather than rigid cutoffs.
Dr. Plummer stressed the importance of balancing competing risks:
“The risk of untreated stage IV cancer approaches 100%. The risk of ventricular arrhythmia from QT prolongation is far lower—but must still be managed wisely.”
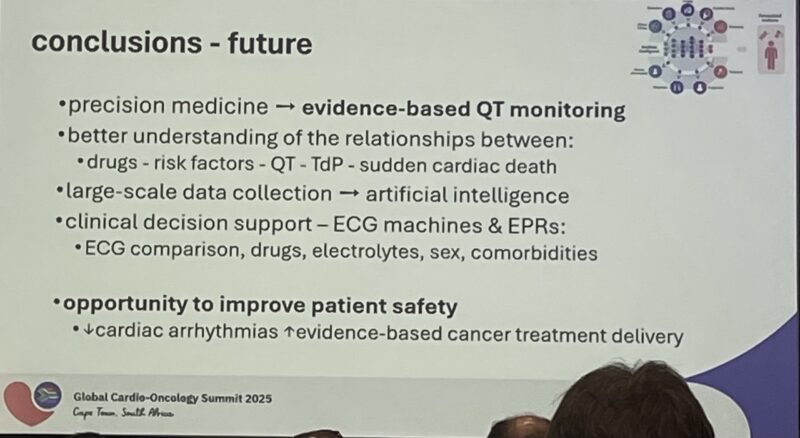
He concluded that improving consistency in QTc assessment and embracing collaborative management between oncologists and cardio-oncologists will help patients achieve “permissive toxicity safely” – maximizing treatment efficacy while minimizing cardiac risk.
Key Takeaways
- Hypertension and QTc prolongation are among the most frequent and clinically relevant cardiovascular toxicities in oncology.
- Proactive monitoring, personalized thresholds, and multidisciplinary collaboration are fundamental to safe cancer therapy.
- Empowering patients through home monitoring and clear follow-up pathways greatly enhances safety.
- Both experts underscored a shared philosophy: cardiovascular management in oncology must support – not interrupt – the optimal cancer treatment plan.
This article is developed by the OncoDaily editorial team,sponsored by Internation Cardio-Oncology Society (IC-OS).
For more information click here.
More content from GCOS 2025 by OncoDaily.