Langerhans Cell Histiocytosis: What patients should know about
What is Langerhans Cell Histiocytosis?
Langerhans cell histiocytosis (LCH) is a rare disorder characterized by the abnormal accumulation and proliferation of Langerhans cells, a type of white blood cell that helps regulate the immune system. These cells can build up in various parts of the body, causing damage to tissues and forming lesions or tumors. LCH can affect people of all ages but is most common in children, particularly those between the ages of 1 and 3.
There is ongoing debate among researchers about whether LCH should be classified as a type of cancer. Some consider it a neoplastic disease (a disease involving abnormal cell growth), while others view it as an inflammatory condition. Regardless of its classification, LCH can range from a mild, self-resolving condition to a severe, life-threatening disease requiring intensive treatment.
Causes and Risk Factors
The exact cause of LCH is unknown. Researchers have identified several genetic mutations, particularly in the BRAF and MAP2K1 genes, that are present in many cases of LCH. These mutations lead to the uncontrolled growth and accumulation of Langerhans cells. However, it is not clear what triggers these genetic changes.
Several risk factors have been associated with LCH, including:
- Family History: A family history of cancer or LCH may increase the risk.
- Environmental Exposures: Exposure to certain chemicals, metals, or dust, particularly in the workplace, may be linked to LCH.
- Infections: Some studies suggest that infections, particularly in newborns, might play a role in the development of LCH.
- Smoking: Smoking is a significant risk factor, especially for pulmonary LCH, which affects the lungs.
Symptoms
Langerhans cell histiocytosis (LCH) is a rare disorder that can affect various parts of the body, leading to a wide range of symptoms. The symptoms depend on which organs or tissues are involved and can vary significantly from one patient to another. Below is a detailed overview of the common symptoms associated with LCH, organized by the affected body systems.
Skin
LCH can manifest in the skin, often presenting as rashes, blisters, or scaly patches. These skin changes can be mistaken for other conditions like eczema or cradle cap. Specific symptoms include:
- Rashes: Red, scaly bumps that may appear in skin folds, such as the groin, armpits, or neck.
- Blisters: Fluid-filled blisters that can be painful or itchy.
- Scaly Patches: Areas of the skin that become dry and flaky, resembling dandruff.
- Cradle Cap: In infants, a scalp rash that looks like a cradle cap, which is a common skin condition.
Bones
Bone involvement is common in LCH, occurring in about 80% of cases. Symptoms related to bone involvement include:
- Pain and Swelling: Painful swelling or lumps over bones, particularly in the skull, arms, legs, ribs, or spine.
- Fractures: Bone lesions can weaken bones, leading to fractures, even with minor injuries.
- Headaches: Persistent headaches, especially if the skull is affected.
- Limp or Trouble Walking: Pain in the legs or spine can cause a limp or difficulty walking.
- Neck or Back Pain: Pain in the neck or back, which may be due to collapsed vertebrae (vertebra plana).
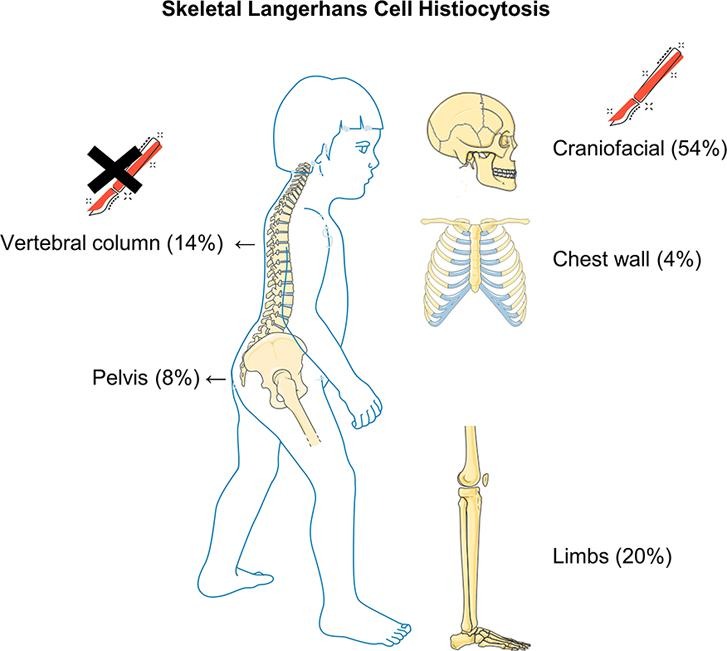
This image is taken from sciencedirect.com
Mouth
LCH can affect the mouth, leading to various dental and oral symptoms:
- Loose Teeth: Teeth that become loose without any apparent reason.
- Swollen Gums: Gums that are swollen, red, and may bleed easily.
- Mouth Sores: Painful sores on the tongue, lips, or inside the cheeks.
Ears
Ear involvement in LCH can lead to recurrent infections and other ear-related symptoms:
- Ear Infections: Frequent ear infections that may not respond well to standard treatments.
- Discharge: Fluid or pus draining from the ear.
- Hearing Loss: Progressive hearing loss due to damage to the ear structures.
Eyes
LCH can affect the eyes, leading to various visual and ocular symptoms:
- Swelling of the Eyelids: Puffy or swollen eyelids.
- Vision Problems: Blurred vision or other visual disturbances.
- Bulging Eyes: Protrusion of one or both eyes, known as exophthalmos.
Lymph Nodes
LCH can cause the lymph nodes to swell, particularly in the neck:
- Swollen Lymph Nodes: Enlarged lymph nodes that may be tender to the touch.
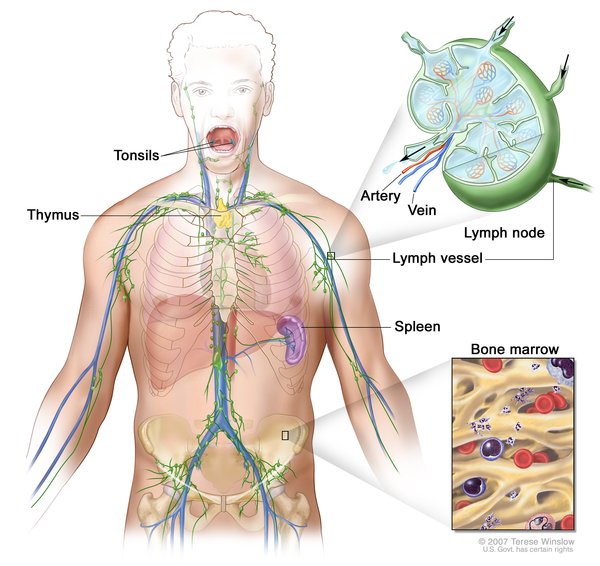
This image is taken from medlineplus.gov
Liver and Spleen
Involvement of the liver and spleen can lead to significant symptoms and complications:
- Enlarged Liver or Spleen: Swelling of the liver (hepatomegaly) or spleen (splenomegaly).
- Jaundice: Yellowing of the skin and eyes due to liver dysfunction.
- Abdominal Swelling: Swelling or distension of the abdomen.
Lungs
Lung involvement is more common in adults, particularly those who smoke. Symptoms include:
- Cough: Persistent cough that may be dry or productive.
- Chest Pain: Pain in the chest, which may worsen with deep breathing or coughing.
- Difficulty Breathing: Shortness of breath or difficulty breathing, especially during physical activity.
Endocrine System
LCH can affect the endocrine system, leading to hormonal imbalances and related symptoms:
- Excessive Thirst and Urination: A condition known as diabetes insipidus, where the body produces large amounts of urine and the patient feels very thirsty.
- Fatigue: Persistent tiredness and lack of energy.
- Hormonal Imbalances: Issues affecting growth and puberty, such as delayed or early puberty.
Central Nervous System
When LCH affects the central nervous system (CNS), it can lead to neurological symptoms:
- Headaches: Severe and persistent headaches.
- Dizziness: Feeling lightheaded or unsteady.
- Seizures: Episodes of uncontrolled electrical activity in the brain.
- Balance Problems: Difficulty maintaining balance or coordination.
Gastrointestinal Tract
LCH can also affect the gastrointestinal tract, leading to digestive symptoms:
- Abdominal Pain: Pain in the stomach or intestines.
- Vomiting and Diarrhea: Frequent vomiting or diarrhea, which can lead to dehydration.
- Blood in Stool: Presence of blood in the stool, indicating gastrointestinal bleeding.
- Poor Growth: In children, poor growth due to malnutrition and digestive issues.
Bone Marrow
Involvement of the bone marrow can lead to hematological symptoms:
- Anemia: Low red blood cell count, causing pale skin, fatigue, and decreased appetite.
- Frequent Infections: Low white blood cell count, leading to frequent infections and fevers.
- Easy Bruising or Bleeding: Low platelet count, resulting in easy bruising or bleeding.
Diagnosis
Diagnosing LCH involves a combination of medical history, physical examination, and various tests to identify the presence and extent of the disease. Common diagnostic tests include:
- X-rays: To detect bone lesions.
- MRI (Magnetic Resonance Imaging): To provide detailed images of organs and tissues.
- PET-CT Scan (Positron Emission Tomography-Computed Tomography): To assess both the structure and function of cells and tissues.
- Biopsy: A sample of affected tissue is examined under a microscope to confirm the presence of Langerhans cells.
Langerhans Cell Histiocytosis Prognosis
The prognosis for LCH varies widely depending on the extent and location of the disease. In many cases, particularly those involving only the skin or a single bone, the disease may resolve on its own or with minimal treatment. However, when LCH affects multiple organs or high-risk organs like the liver, spleen, or bone marrow, the prognosis can be more serious and may require intensive therapy.
Children with low-risk LCH generally have a very good prognosis, with survival rates close to 99%. For high-risk LCH, the survival rate is around 80%. Long-term outcomes can include chronic health issues such as bone defects, hearing loss, or hormonal imbalances.
This informative video is taken from Demystifying Medicine McMaster.
Treatment
Treatment for Langerhans cell histiocytosis (LCH) varies widely depending on the severity and location of the disease. The goal of treatment is to control symptoms, prevent complications, and improve the quality of life. Here is a detailed overview of the treatment options available for LCH, along with their potential side effects.
Observation
In mild cases, particularly those involving only the skin, no treatment may be necessary. The disease may resolve on its own without intervention. This approach is often referred to as “watchful waiting” or “active surveillance.” During this period, regular follow-ups are essential to monitor the disease’s progression and ensure that it does not worsen.
Surgery
Surgery is often used for isolated bone lesions. The surgical procedure typically involves the removal of the affected tissue, which can help alleviate pain and prevent further damage to the bone. Surgery may also be required initially to obtain a biopsy for diagnostic purposes. In some cases, all of the LCH cells may be removed during the biopsy, eliminating the need for further treatment.
Side Effects of Surgery:
- Pain and swelling at the surgical site
- Risk of infection
- Scarring
- Potential for damage to surrounding tissues
Chemotherapy
Chemotherapy is a common treatment for more extensive LCH. It involves the use of drugs to kill or inhibit the growth of abnormal Langerhans cells. Chemotherapy can be administered orally (as a pill), subcutaneously (under the skin), or intravenously (directly into the bloodstream). Common chemotherapy drugs used for LCH include vinblastine, prednisone, methotrexate, and mercaptopurine.
Side Effects of Chemotherapy:
- Nausea and vomiting
- Hair loss
- Fatigue
- Increased risk of infections due to lowered white blood cell counts
- Anemia (low red blood cell count)
- Thrombocytopenia (low platelet count), leading to easy bruising or bleeding
- Mouth sores
- Loss of appetite
Radiation Therapy
Radiation therapy uses high-energy rays to damage or kill abnormal cells and shrink tumors. It is sometimes used for localized lesions that do not respond to other treatments. Radiation therapy can be particularly effective for bone lesions and lesions in critical areas where surgery is not feasible.
Side Effects of Radiation Therapy:
- Skin irritation or burns at the treatment site
- Fatigue
- Hair loss in the treated area
- Risk of secondary cancers
- Potential damage to surrounding healthy tissues
- Growth abnormalities in children
Targeted Therapy
Targeted therapy involves the use of drugs that specifically target genetic mutations associated with LCH, such as BRAF and MAP2K1 mutations. BRAF inhibitors like vemurafenib and dabrafenib, and MEK inhibitors like trametinib, have shown promise, particularly for relapsed or refractory LCH. These drugs work by blocking the pathways that allow Langerhans cells to grow and proliferate.
Side Effects of Targeted Therapy:
- Skin rash
- Diarrhea
- Fatigue
- Joint pain
- Increased risk of infections
- Liver toxicity
- Potential for developing resistance to the drugs over time
Immunotherapy
Immunotherapy aims to boost the body’s immune system to fight the disease. Monoclonal antibodies targeting specific proteins on Langerhans cells, such as CD1a or CD52, are being explored as potential treatments. These therapies can help the immune system recognize and destroy abnormal cells.
Side Effects of Immunotherapy:
- Flu-like symptoms (fever, chills, fatigue)
- Skin reactions at the injection site
- Autoimmune reactions, where the immune system attacks healthy tissues
- Risk of severe allergic reactions
Photodynamic Therapy
Photodynamic therapy involves the use of light-sensitive drugs and a light source to destroy abnormal cells. This treatment is sometimes used for skin lesions in LCH.
Side Effects of Photodynamic Therapy:
- Skin redness and swelling
- Sensitivity to light
- Pain at the treatment site
Stem Cell Transplant
In severe cases, particularly those involving multiple organ systems or high-risk organs, a stem cell transplant may be considered. This procedure involves replacing the patient’s diseased bone marrow with healthy stem cells from a donor. Stem cell transplants can help restore normal blood cell production and immune function.
Side Effects of Stem Cell Transplant:
- Risk of infections due to immunosuppression
- Graft-versus-host disease (GVHD), where the donor cells attack the recipient’s tissues
- Organ damage
- Infertility
- Secondary cancers
Hormone Replacement Therapy
For patients with endocrine involvement, such as diabetes insipidus, hormone replacement therapy may be necessary to manage symptoms. This can include medications to replace deficient hormones and maintain normal bodily functions.
Side Effects of Hormone Replacement Therapy:
- Weight gain
- Mood changes
- Increased risk of osteoporosis
- Potential for hormone imbalances
Experimental Treatments and Clinical Trials
New treatments for LCH are continually being explored through clinical trials. These may include novel targeted therapies, immunotherapies, and other experimental approaches. Participation in clinical trials can provide access to cutting-edge treatments that are not yet widely available.
Side Effects of Experimental Treatments:
- Vary depending on the specific treatment being tested
- Potential for unknown or unexpected side effects
- Close monitoring is required to manage adverse reactions
Newest Options and Ongoing Trials
Recent advances in understanding the genetic basis of LCH have led to the development of targeted therapies. These treatments focus on inhibiting the specific pathways involved in the disease, such as the MAPK pathway. Clinical trials are ongoing to evaluate the effectiveness of these new treatments, including:
- BRAF Inhibitors: Drugs like vemurafenib target the BRAF* V600E mutation found in many LCH cases.
- MEK Inhibitors: These drugs target the MAP2K1* gene and are being tested for their ability to control LCH.
- Immunotherapy: Approaches like CAR-T cell therapy are being explored for their potential to treat LCH by harnessing the body’s immune system.
*Mutations of these genes may result in uncontrollable cell division and cancer.
More information about ongoing clinical trials can be found on clinicaltrials.gov
Prevention
There are no known ways to prevent LCH, as the exact cause of the disease is still unclear. However, reducing exposure to known risk factors, such as smoking and certain environmental chemicals, may help lower the risk. Regular medical check-ups and early detection can improve outcomes for those at risk.
Conclusion
Langerhans cell histiocytosis is a complex and rare disorder with a wide range of symptoms and outcomes. While the exact cause remains unknown, advances in genetic research have improved our understanding of the disease and led to new treatment options. Early diagnosis and appropriate treatment are crucial for managing LCH and improving the quality of life for affected individuals. Patients and their families should work closely with healthcare providers to develop a personalized treatment plan and stay informed about the latest research and clinical trials.
Resources
- National Cancer Institute – cancer.gov
- Langerhans cell histiocytosis – medlineplus.gov
- Clinical trials for Langerhans cell histiocytosis – Clinicaltrials.gov
- SEER Hematopoietic and Lymphoid Neoplasm Database, SEER Cancer- seer.cancer.gov
- American Society of Clinical Oncology – cancer.net
- American Cancer Society – cancer.org
- Histiocytosis syndromes in children: II. Approach to the clinical and laboratory evaluation – PubMed
- Genetic landscape of adult Langerhans cell histiocytosis with lung involvement – European Respiratory Journal
- Clinical characteristics, genomic profiling and outcomes of single system multifocal Langerhans cell histiocytosis in adults with bone involvement – Nature.com
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
