What is Immunotherapy?
Immunotherapy is a groundbreaking cancer treatment that helps the body’s own immune system recognize and attack cancer cells. Unlike chemotherapy, which directly kills cancer cells, immunotherapy boosts the body’s natural defenses to fight the disease more effectively. The immune system is constantly on the lookout for threats like bacteria and viruses, but cancer cells are tricky. They disguise themselves to hide from immune cells, allowing them to grow unchecked. Immunotherapy removes these disguises or activates the immune system, making it stronger in recognizing and destroying cancer cells.
This treatment has changed cancer care, offering longer-lasting effects than some traditional therapies. While it doesn’t work for everyone, for some patients, it has led to remission or prolonged survival, even in advanced cancers. However, like any treatment, it comes with side effects, which we’ll explore in this article—helping you understand what to expect and how to manage them.
How Does Immunotherapy Work?
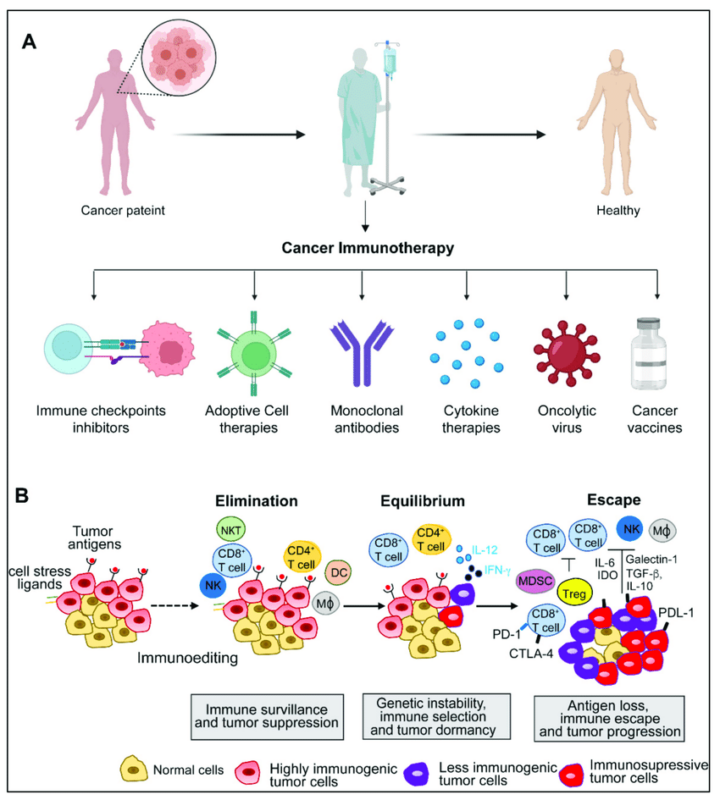
Imagine your immune system as a powerful security team that constantly scans your body for threats like viruses, bacteria, and even cancer cells. Normally, it does a great job protecting you, but cancer is tricky—it can hide from the immune system or even turn off its defenses. That’s where immunotherapy steps in. Immunotherapy acts like a special training program for your immune system, helping it recognize and attack cancer cells more effectively. Here’s how it works:
- Checkpoint Inhibitors – Think of your immune system as a car with brakes. Cancer can keep the brakes on, preventing an attack. Checkpoint inhibitors release the brakes, allowing immune cells to go full speed and fight the cancer.
- Monoclonal Antibodies – These lab-made proteins work like special forces, marking cancer cells so the immune system can easily spot and destroy them.
- CAR-T Cell Therapy – Doctors take your own immune cells, reprogram them in a lab to hunt cancer, and then put them back into your body to do their job.
- Cancer Vaccines – Just like vaccines train your immune system to fight viruses, cancer vaccines help your body recognize and target cancer cells.
By boosting the immune response, immunotherapy can help shrink tumors, stop cancer from spreading, and even lead to long-term remission in some cases. However, because it supercharges the immune system, it can sometimes cause side effects, which we’ll explore next.
Why Does Immunotherapy Cause Side Effects?
Immunotherapy works by supercharging the immune system to recognize and attack cancer cells. But sometimes, in its effort to fight cancer, the immune system becomes overactive and mistakenly attacks healthy cells and tissues, leading to side effects. Think of it like a security alarm system. Normally, it’s supposed to go off only when an intruder (cancer cells) enters. But with immunotherapy, the alarm can become extra sensitive, sometimes triggering even when there’s no real danger—leading to inflammation in different parts of the body.
Understanding why these side effects happen can help patients feel more prepared and in control of their treatment journey. And the good news? Doctors have ways to manage these effects so that immunotherapy remains both safe and effective!
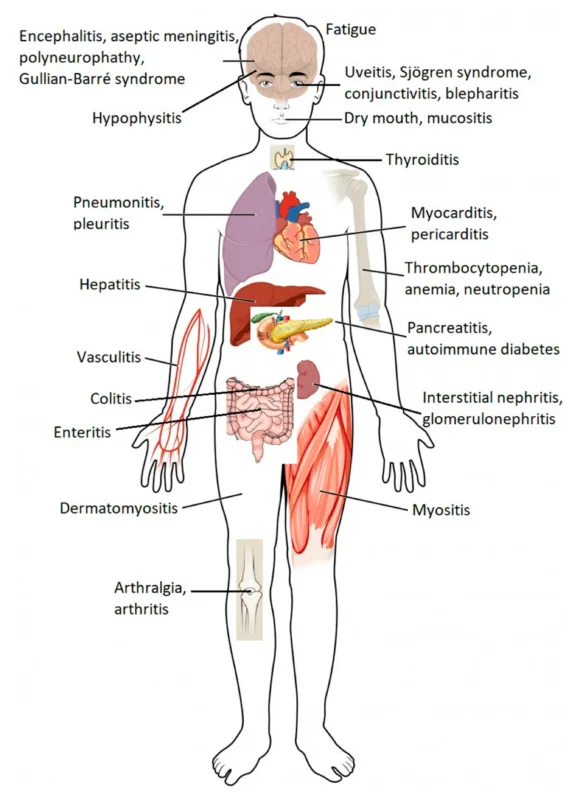
What Are the Side Effects of Cancer Immunotherapy?
Immunotherapy can lead to side effects, which can range from mild to more serious. Some of the most common side effects include:
- Fatigue – Feeling more tired than usual, even after a full night’s sleep.
- Skin changes – Rashes, dryness, or itchiness, like an unexpected sunburn.
- Flu-like symptoms – Fever, chills, muscle aches, and a general “under-the-weather” feeling.
- Digestive issues – Nausea, diarrhea, or stomach pain, making food less enjoyable.
In some cases, the immune system may attack major organs, leading to inflammation in the lungs (pneumonitis), liver (hepatitis), or intestines (colitis). While this sounds scary, doctors monitor patients closely and have ways to control these side effects early with medications like steroids. Not everyone experiences side effects, and many are mild and manageable. The key is to listen to your body, report any changes to your doctor, and stay proactive in managing symptoms. Immunotherapy is changing cancer treatment, and with the right care, many patients are able to continue treatment while maintaining a good quality of life.
When to Expect Side Effects
One of the biggest questions patients have about immunotherapy is: “When will I start feeling side effects?”. Unlike chemotherapy, which often causes immediate side effects, immunotherapy works differently. It takes time for the immune system to wake up and start attacking cancer cells—and sometimes, healthy cells too. For some patients, side effects show up within days or weeks after starting treatment. Others may not notice anything until months later. And here’s the tricky part: side effects can appear even after treatment has ended, since the immune system may stay active for a long time.
- First few weeks – Fatigue, mild skin rashes, or flu-like symptoms may appear.
- First few months – More noticeable effects, like digestive issues or joint pain, can develop.
- Months to a year later – Delayed side effects, such as inflammation in the lungs or liver, may occur.
Since side effects can be unpredictable, regular check-ups and early reporting of symptoms are key. Even mild changes—like a cough that won’t go away or unusual fatigue—shouldn’t be ignored. The earlier side effects are managed, the easier they are to control, ensuring a smoother treatment journey with fewer interruptions.
How Long Do Side Effects of Immunotherapy Last?
The duration of immunotherapy side effects can vary widely. Some are short-lived and disappear quickly, while others may linger for months or even become permanent. Understanding how long side effects last is essential for managing them effectively and ensuring the best quality of life during and after treatment.
- Short-Term Side Effects: Many patients feel side effects within days or weeks of starting immunotherapy, but the good news is that these often improve quickly after stopping treatment or with proper care. Flu-like symptoms such as fever, chills, muscle aches, and fatigue are common in the beginning but usually fade within a few weeks. Skin rashes and itching can also appear early but often respond well to moisturizers, topical creams, or mild corticosteroids. Gastrointestinal issues, like diarrhea or colitis, may require anti-inflammatory medication, while thyroid problems (either hypothyroidism or hyperthyroidism) can develop in the first few months, sometimes needing short-term hormone therapy.
- Long-Term Side Effects: Some side effects don’t go away right away and may last for months or even years. Endocrine disorders, like thyroid dysfunction or adrenal insufficiency, may require long-term hormone replacement therapy to keep the body balanced. Chronic inflammation in the lungs (pneumonitis), joints (arthritis), or nerves (neuropathy) can cause lasting discomfort and may need ongoing treatment with immunosuppressive medications.
- Permanent Side Effects: In rare cases, immunotherapy can cause irreversible damage to certain organs. Some patients develop type 1 diabetes due to immune system attacks on the pancreas, leading to lifelong insulin dependency. Inflammation in the heart (myocarditis), lungs (severe pneumonitis), or kidneys (nephritis) can cause permanent impairment if not detected early.
Do Side Effects Mean That Treatment is Working?
Many patients wonder, “If I have side effects, does that mean my immunotherapy is working?” The answer isn’t always simple, but here’s what you need to know. Side effects happen because immunotherapy boosts your immune system, making it more aggressive in attacking cancer. But sometimes, it also attacks healthy cells, leading to inflammation and side effects. So while side effects can be a sign that your immune system is active, they don’t necessarily mean the treatment is working against the cancer.
On the other hand, not having side effects doesn’t mean the treatment isn’t working. Every patient’s immune system responds differently. Some people see great results with few or no side effects, while others experience strong reactions even if the treatment isn’t fully effective. What really matters is regular monitoring through scans and blood tests. These tests show whether the cancer is shrinking or staying under control—not the presence or absence of side effects.
Managing Side Effects: What Can You Do?
Dealing with side effects from immunotherapy can feel overwhelming, but the good news is there are ways to manage them and feel better! The key is to stay proactive—recognizing symptoms early and taking steps to control them before they get worse.
- Listen to Your Body: Side effects can range from mild fatigue to more serious inflammation in the lungs, liver, or intestines. If something feels off—don’t ignore it! Even a small cough, skin rash, or stomach issue can be a sign that your immune system is overactive. Report any new or worsening symptoms to your doctor right away. The sooner they’re addressed, the easier they are to treat.
- Stay Hydrated and Eat Well: Your body is working hard, so fuel it with the right nutrition! Drinking plenty of water helps with fatigue and keeps your system running smoothly. If you’re dealing with nausea or diarrhea, stick to bland, easy-to-digest foods like rice, bananas, or toast. If you’re losing your appetite, try eating small, frequent meals instead of three big ones.
- Protect Your Skin:Many immunotherapy treatments cause rashes, itching, or dryness. To soothe irritated skin, use gentle, fragrance-free moisturizers and avoid hot showers that strip natural oils. Sunscreen is a must! Some treatments make your skin extra sensitive to sunlight, so wear SPF 30+ even on cloudy days.
- Balance Rest and Activity: Fatigue is common, but staying in bed all day can make it worse. Try light activities like short walks or stretching to keep your energy up. But also, listen to your body—rest when you need to!
- Ask About Medications: Doctors can prescribe medications to help manage side effects. Steroids can calm inflammation, while other drugs help with nausea, diarrhea, or pain. Never wait for side effects to get unbearable—early treatment makes a big difference!
- Stay Connected: You don’t have to go through this alone. Talk to your doctor, join a support group, or lean on friends and family. Many patients find comfort in sharing their experiences with others who understand.
Immunotherapy vs. Chemotherapy Side Effects
Both immunotherapy and chemotherapy are used to fight cancer, but they work in very different ways—which means the side effects are different, too. Understanding these differences can help patients feel more prepared and know what to expect.
Chemotherapy kills fast-growing cells, including cancer cells—but also healthy ones like those in the hair, digestive system, and bone marrow. This is why chemo can cause hair loss, nausea, and low blood cell counts. Immunotherapy doesn’t attack cancer directly. Instead, it activates the immune system to find and destroy cancer cells. But sometimes, the immune system also attacks healthy tissues, leading to inflammation-related side effects in different organs.
Chemotherapy Side Effects tend to happen quickly, often within days of starting treatment. Patients may experience hair loss, nausea, vomiting, mouth sores, and a weakened immune system due to lower blood cell counts. Immunotherapy Side Effects can appear later—sometimes weeks or even months after starting treatment. The immune system may cause fatigue, skin rashes, flu-like symptoms, and inflammation in the lungs, liver, or intestines. Chemo side effects usually stop once treatment ends, and the body begins to recover. Immunotherapy side effects can linger for months or even years because the immune system remains active for a long time. Some effects may even be permanent if they cause long-term damage to organs.
| Aspect | Immunotherapy | Chemotherapy |
| Mechanism of Action | Stimulates the immune system to recognize and attack cancer cells. | Targets rapidly dividing cells, including cancer cells and some healthy cells. |
| Common Side Effects | Fatigue, skin reactions, gastrointestinal issues, endocrine disorders, flu-like symptoms. | Fatigue, nausea, vomiting, hair loss, bone marrow suppression, gastrointestinal issues. |
| Onset of Side Effects | Can appear weeks to months after starting treatment; some may appear even after treatment has ended. | Typically occurs shortly after treatment begins and subside once treatment ends. |
| Duration of Side Effects | Can be long-lasting or even permanent; some side effects may persist long after treatment has concluded. | Generally short-term and resolve after treatment ends, though some long-term effects can occur. |
| Severity of Side Effects | Can range from mild to severe; severe side effects may require immunosuppressive treatment. | Can range from mild to severe; severe side effects often require supportive care and management. |
| Management of Side Effects | Requires monitoring for irAEs; may need steroids or other immunosuppressants. | Often managed with medications to control nausea, pain, and other symptoms; supportive care is crucial. |
| Long-Term Effects | Potential for long-term immune system changes and autoimmune conditions. | Potential for long-term damage to organs such as the heart, lungs, and nerves. |
| Impact on Quality of Life | Can significantly impact the quality of life due to chronic or severe autoimmune reactions. | Can significantly impact the quality of life due to immediate and intense side effects, but these often improve after treatment. |
| Predictability | Less predictable; side effects can vary widely among patients and may appear long after treatment. | More predictable; side effects typically follow a known pattern based on the specific drugs used. |
When to See a Doctor
Patients undergoing immunotherapy should contact their healthcare provider if they experience any new or worsening symptoms, even if they seem minor. Immediate medical attention is required for severe symptoms such as difficulty breathing, chest pain, severe abdominal pain, high fever, or signs of an allergic reaction. Regular follow-up appointments are essential to monitor for late-onset side effects and adjust treatment plans as necessary.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD