
New Series by Nico Gagelmann: Rarity in Hematology – BPDCN
Nico Gagelmann, Hematologist at University Hospital Hamburg-Eppendorf, Young National Society Ambassador at European Hematology Association (EHA), and Chair of the CAR-T for plasma cell disorder committee at The EBMT, shared a post on X:
“Welcome to a new series.
Rarity in hematology.
Starting with BPCDN.
Share hematological conditions you never really understood or heard of, but would like to know more about.
I guarantee I will cover all suggestions in future threads!
Rarity in hematology.
Blastic Plasmacytoid Dendritic Cell Neoplasm (BPDCN)
Rare but aggressive blood cancer with a name as complex as its behavior.
Let’s break it down in an educational.
Definition:
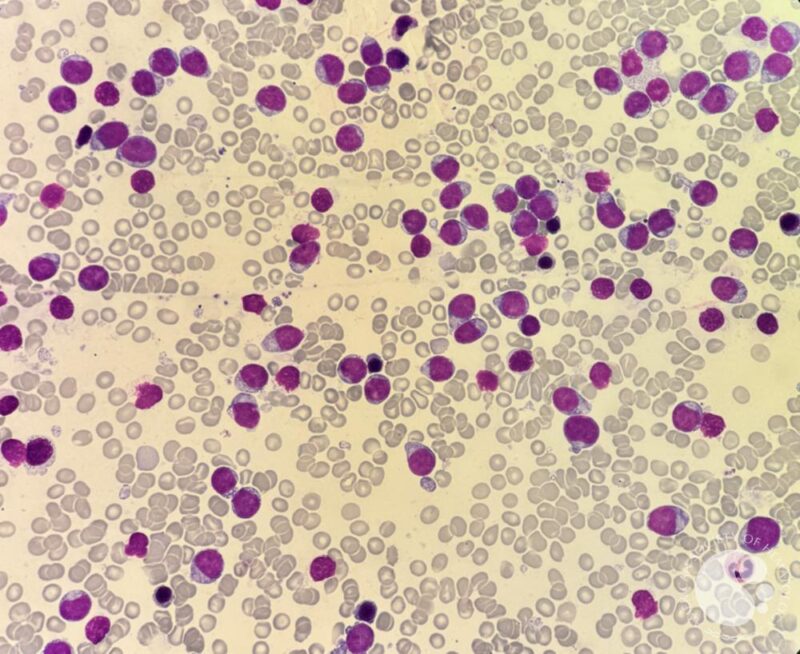
- a rare hematologic malignancy arising from precursors of plasmacytoid dendritic cells (pDCs)
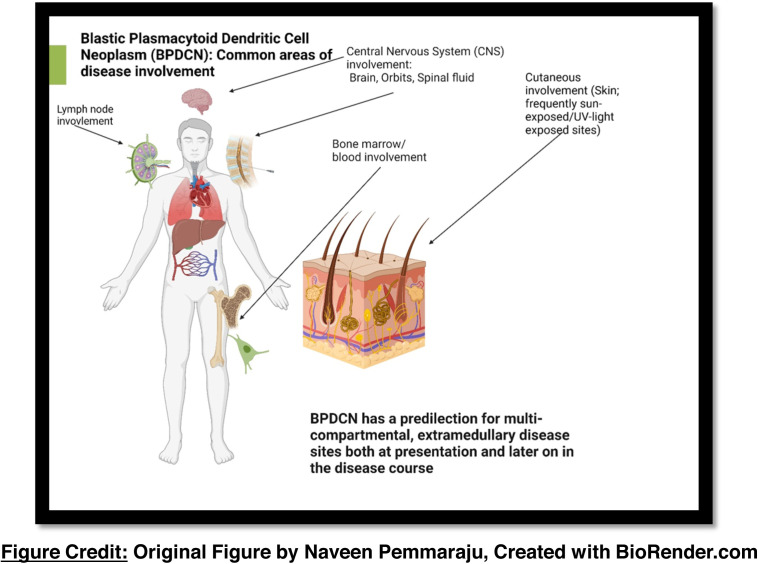
- can involve skin, bone marrow, blood, lymph nodes, central nervous system
- more common in adults (60-70 years) and males (~3:1)
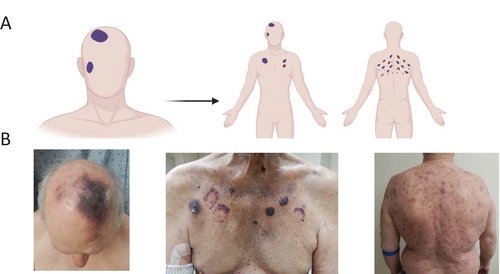
First signs? often purple skin lesions.
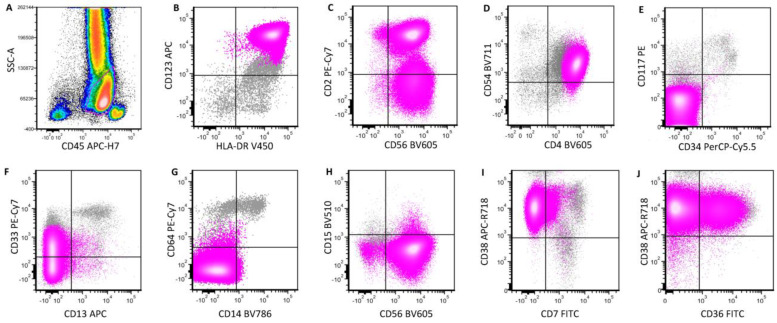
Diagnosis hinges on immunophenotyping:
- Remember the signature: ‘123, 4, 56’
- CD123+, CD4+, CD56+
- additional pDC markers: TCF4, TCL1, CD303, CD304
- negative for CD3, CD14, CD34, MPO
Classic clinical presentation:
- deep violaceous plaques or nodules (esp. on scalp, face, chest)
- often misdiagnosed as bruises or benign skin lesions
- 80-90% have skin involvement at diagnosis
BE AWARE
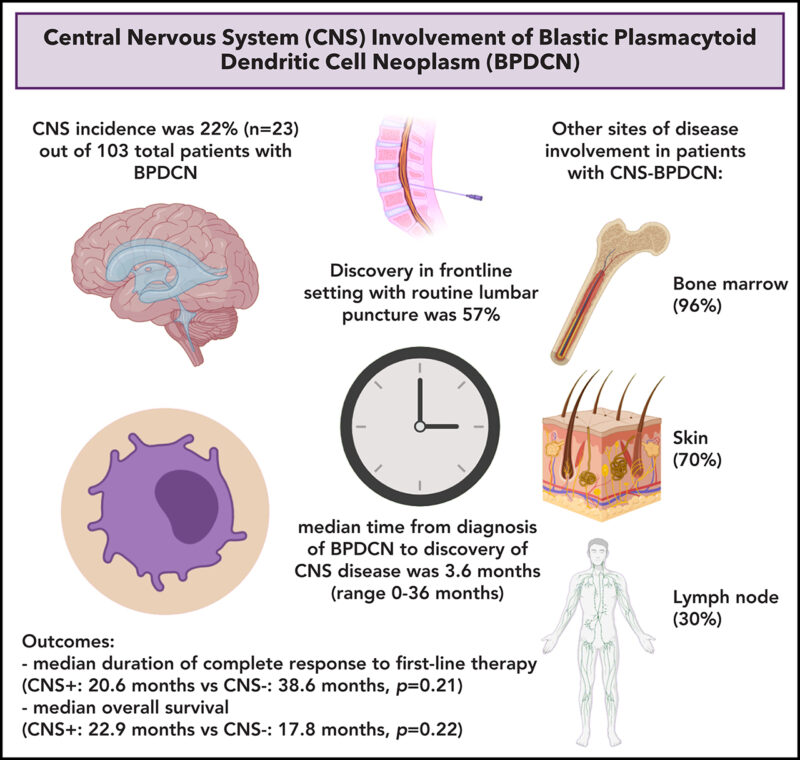
CNS and systemic disease:
- CNS involvement common, often asymptomatic
- ‘systemic-only’ disease less common but under-recognized
- always evaluate CSF + perform CNS prophylaxis
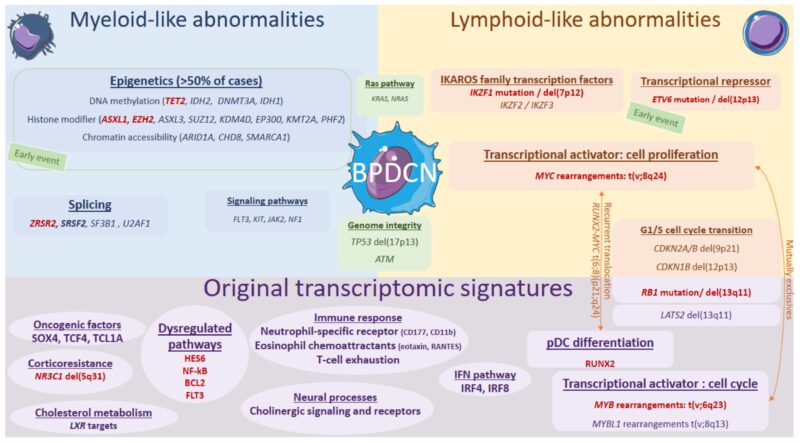
Pathophysiology:
- BPDCN harbors mutations commonly found in myeloid malignancies
- -TET2 (most frequent)
- -ASXL1, TP53, ZRSR2 (X-linked, linked to male predominance)
- -MYC or MYB fusions (esp. in children)
ALSO, think of associated conditions
- Up to 30-50% of adult BPDCN cases have concurrent or preceding CMML, MDS, or AML
- This dual pathology can influence treatment decisions
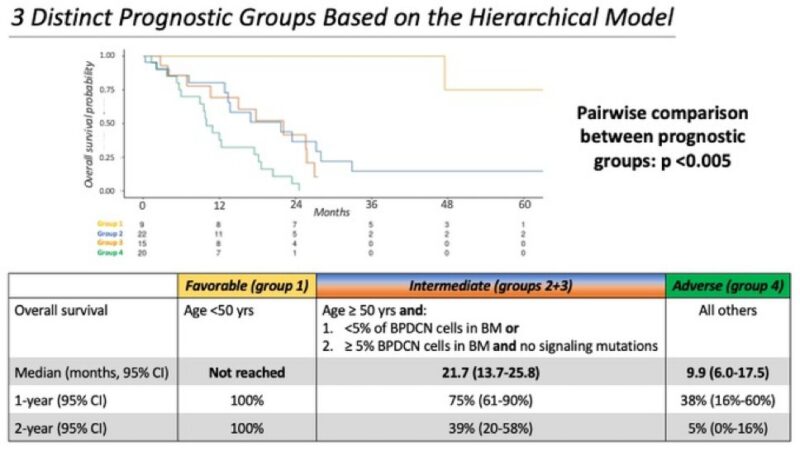
Prognosis:
- median overall survival: 18–24 months
- 3 key variables for worse outcomes:
- -age ≥ 50
- -bone marrow involvement of ≥5%
- -activating signaling mutations (e.g., NRAS, KRAS)
- stratifies patients into favorable, intermediate and adverse risk
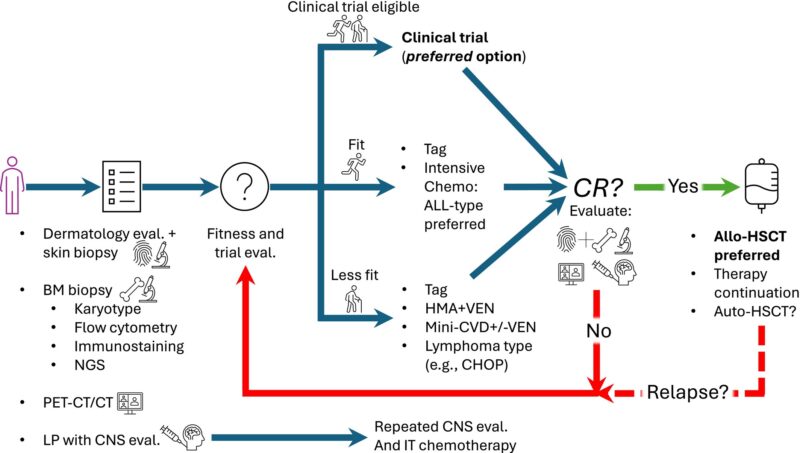
Treatment options in a nutshell (1st line):
- hyper-CVAD (ALL-based chemo) for young, fit patients
- Tagraxofusp (CD123-targeted therapy), FDA-approved
- hypomethylating agents + venetoclax for older or less fit patients
Tagraxofusp (SL-401):
- IL-3 + diphtheria toxin fusion
- targets CD123
- response rate ~72%
- risk: Capillary Leak Syndrome (CLS)
- only agent FDA and EMA-approved specifically for BPDCN
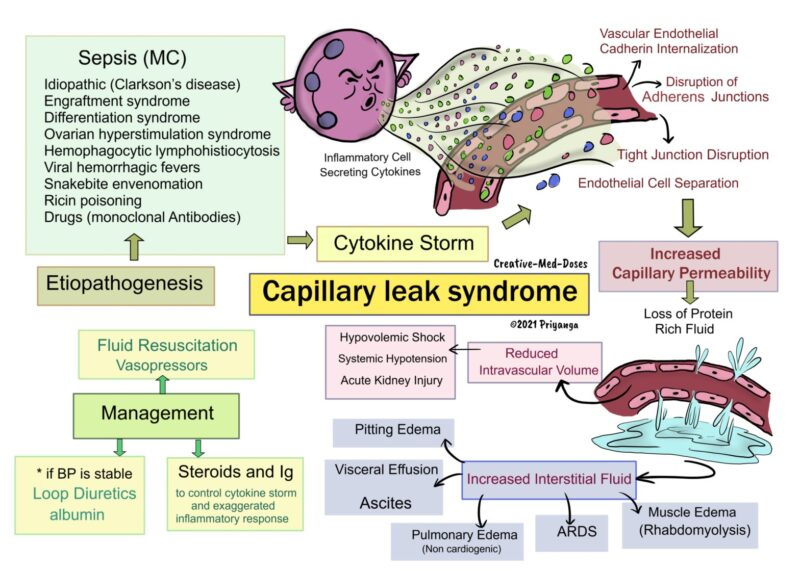
CLS, the Achilles’ heel of Tagraxofusp:
- life-threatening capillary leak risk
- careful patient selection, premedication and inpatient monitoring in Cycle 1 is essential
- CLS is mostly a Cycle 1 toxicity
Venetoclax-based regimens:
- effective in older adults
- often combined with azacitidine (HMA)
- responses often seen but typically short-lived
- useful when intensive chemo or tagraxofusp is contraindicated
CNS prophylaxis is a must
- 60% of patients may have occult CNS involvement at diagnosis
- all patients should receive intrathecal chemo
- pediatric ALL regimens naturally cover CNS
Novel therapies in the pipeline:
- Tagraxofusp-azacitidine-venectoclax triplet
- IMGN632 (anti-CD123 ADC)
- CD123 CAR-T and CAR-NK cells
- bispecifics (e.g., flotetuzumab)
Trials are expanding rapidly.
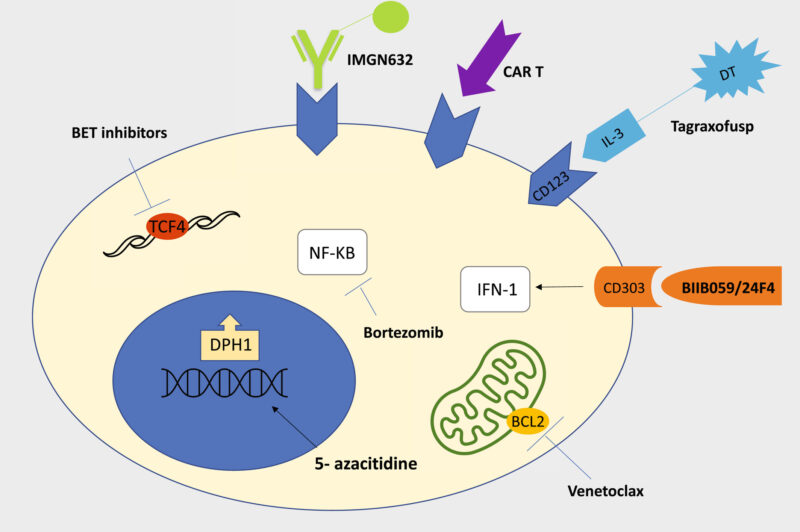
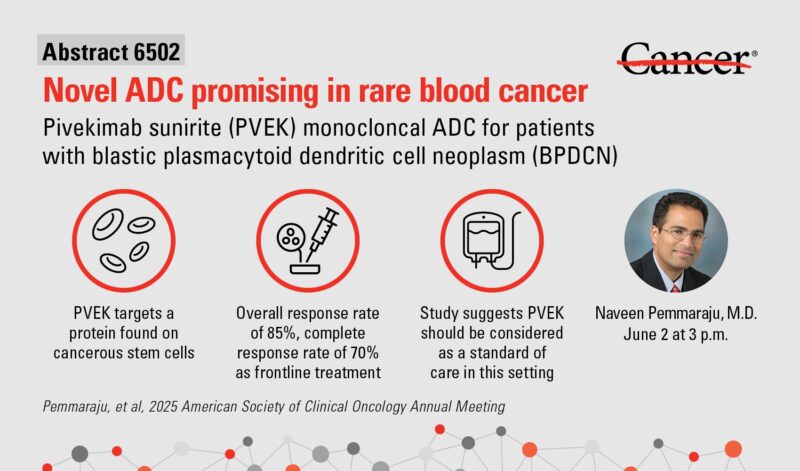
Drug spotlight: IMGN632 (pivekimab sunirine)
- CD123-targeted antibody-drug conjugate in trials for both newly diagnosed and relapsed/refractory BPDCN
- doesn’t cause CLS, although though peripheral edema has been reported
- active even in some patients who failed tagraxofusp
Pediatric BPDCN is different:
- more favorable biology (e.g., MYB rearrangements)
- better response to pediatric ALL protocols
- transplant may not always be necessary
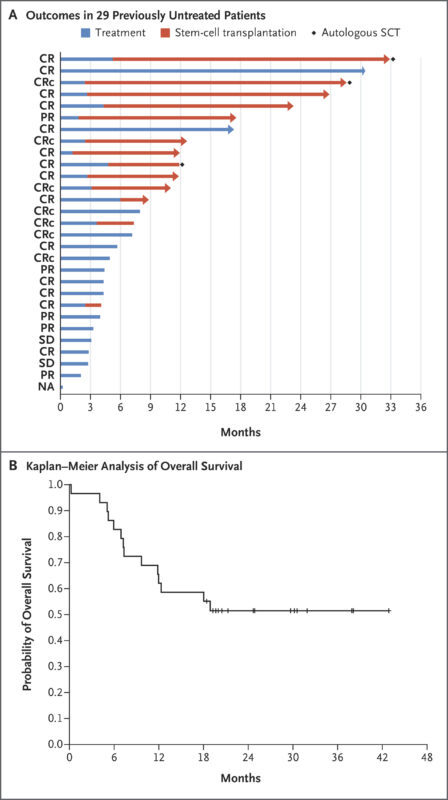
Post-remission consolidation:
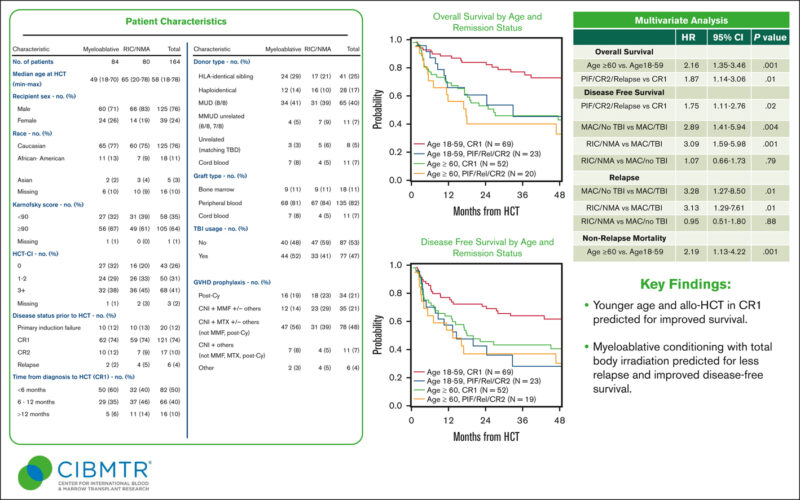
- allogeneic hematopoietic stem cell transplantation is standard for eligible adults in first complete remission
- 5-year OS ~50%
- potential for tagraxofusp maintenance after transplant
- consider auto-HSCT only in select low-risk cases
Relapse management:
- repeat profiling
- switch treatment class
- clinical trial enrollment strongly encouraged
- second transplants, donor lymphocyte infusion or newer targeted therapies
Take-home message:
- BPDCN is rare but deadly
- Increased awareness, early diagnosis, and evolving therapies like tagraxofusp, venetoclax and transplant are changing the game
- Still, relapse is common
Follow and read Naveen Pemmaraju, Shai Shimony, and others to learn more.
References and resources on BPDCN.”
Flow Cytometry Profiling of Plasmacytoid Dendritic Cell Neoplasms
Tagraxofusp in Blastic Plasmacytoid Dendritic-Cell Neoplasm
Central nervous system involvement in blastic plasmacytoid dendritic cell neoplasm
Blastic Plasmacytoid Dendritic Cell Neoplasm 1
More posts featuring Nico Gagelmann.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
