Top 5 AI Tools for Radiation Oncologists: What Clinicians Need to Know
Artificial intelligence (AI) has emerged as a transformative force in modern oncology, particularly within the field of radiation oncology. As treatment planning grows more complex, image-guided modalities become more precise, and the demand for personalized care increases, AI tools for radiation oncologists offer a promising solution to reduce clinician burden and enhance treatment quality. From auto-segmentation of tumors and organs-at-risk (OARs) to adaptive radiotherapy and predictive analytics, these technologies are no longer future ambitions—they are active components of contemporary cancer care.
The integration of AI tools for radiation oncologists into clinical workflows is enabling practitioners to reduce variability, improve efficiency, and deliver more individualized treatment plans. Automation in contouring and planning reduces interobserver differences and saves valuable time. Adaptive radiotherapy platforms allow for treatment modification in real time based on changing patient anatomy, while radiomics and machine learning models can identify responders to specific therapies and inform prognosis. Even large language models trained on oncology-specific datasets are beginning to support clinical decision-making, documentation, and patient triage.
Among the most impactful AI tools for radiation oncologists currently advancing the field are MVision AI, a leading auto-contouring solution; Varian Ethos, an adaptive radiotherapy system; RayStation, which integrates AI-based planning optimization; TheraPanacea ART-Plan, a vendor-neutral adaptive radiotherapy platform; and Imbio Lung Suite, which supports AI-powered radiomics and image-based prognostics. These tools represent the cutting edge of intelligence-driven oncology care and reflect a broader shift toward precision, automation, and data integration in cancer treatment.
As radiation oncologists are increasingly called upon to integrate high-dimensional data into their therapeutic decisions, the ability to interpret and apply artificial intelligence will become essential. This article explores five of the most impactful AI tools for radiation oncologists, examining their clinical utility, scientific foundations, and potential to improve patient outcomes.

Read About AI in Oncology on OncoDaily
MVision AI: Automating Contours Without Compromising Quality
One of the most time-intensive tasks in radiation oncology is the manual contouring of organs-at-risk (OARs) and tumor volumes. MVision AI, a CE-certified deep learning-based software, addresses this challenge by offering fully automated contouring capabilities tailored for clinical radiotherapy workflows. It provides auto-segmentation of over 50 anatomical structures and has been shown to significantly reduce contouring time while maintaining high clinical accuracy.
MVision operates as a cloud-based platform that integrates directly with treatment planning systems. Using large-scale training datasets derived from diverse patient populations, the software rapidly generates contours for critical structures such as the spinal cord, bladder, heart, lungs, parotid glands, and nodal regions. These contours are delivered within minutes and can be manually reviewed and adjusted, allowing radiation oncologists to maintain full control over the planning process.
In a prospective evaluation by Heijkoop and colleagues (2023), the quality of MVision’s contours was analyzed in a multicenter setting. The study found that in over 90% of cases, the auto-generated contours were clinically acceptable and required only minor edits. Notably, significant time savings were reported across several cancer types, including head and neck, prostate, and thoracic malignancies—regions where contouring complexity is high. The study concluded that MVision AI not only improves efficiency but also enhances reproducibility by minimizing interobserver variability (Heijkoop et al., 2023).
Another key advantage of MVision is its transparent and modifiable output. Unlike “black box” AI models, MVision allows users to view, verify, and override any contour. This transparency fosters clinical trust and ensures that patient safety remains the top priority.
As radiation oncology departments face increasing patient volumes and pressure to streamline treatment workflows, MVision AI is proving to be an indispensable tool. It exemplifies how artificial intelligence can reduce clinician workload while upholding the precision and individualization required for effective cancer care.

Photo: Depositphotos
Varian Ethos: Personalized Radiotherapy in Real Time
Adaptive radiotherapy (ART) has long been recognized as a promising advancement in precision oncology, offering the ability to modify treatment based on daily changes in tumor or patient anatomy. However, its widespread implementation was historically limited by time, complexity, and workflow challenges. Varian’s Ethos system addresses these obstacles through the integration of artificial intelligence, automation, and real-time image guidance, enabling online adaptive radiotherapy (oART) that is both efficient and clinically practical.
Ethos is a next-generation radiotherapy platform equipped with an integrated linear accelerator and cone-beam CT (CBCT) system. The defining feature of Ethos is its AI-driven adaptive planning engine, which automates key steps such as contour propagation, dose recalculation, plan evaluation, and approval—all in real time, during the treatment session. This innovation allows clinicians to account for daily anatomical variations, such as tumor shrinkage, organ motion, or changes in bladder and rectal filling, which can otherwise compromise dose delivery and increase toxicity.
Clinical validation of Ethos is growing. In a study published by Barragán Montero et al. (2023), the authors assessed the feasibility and dosimetric impact of Ethos-guided oART across multiple tumor sites. The study demonstrated that Ethos enables daily adaptation with minimal workflow disruption, and that adaptive plans significantly improved target coverage and sparing of organs-at-risk in pelvic and abdominal cancers. Importantly, the adaptation process—powered by machine learning algorithms—took under 15 minutes per session in most cases, making it viable even in high-volume centers (Barragán Montero et al., 2023).
Ethos is especially valuable in treating cancers such as non-small cell lung cancer, rectal cancer, cervical cancer, and prostate cancer, where intra- and interfraction anatomical variability can be significant. By adapting plans based on patient-specific anatomy on each treatment day, clinicians can reduce margins, escalate dose safely, and potentially improve both local control and toxicity profiles.
The incorporation of artificial intelligence in Ethos streamlines contouring, planning, and QA steps, enabling radiation oncologists to focus more on clinical decision-making and less on technical execution. Its “adaptive-first” philosophy signals a paradigm shift in radiotherapy, transforming it from a static plan to a dynamic, learning-based process.
As the use of Ethos expands across academic and community centers, it exemplifies how AI can not only accelerate workflows but also enhance the personalization of treatment in a way that was not previously feasible.
Photo: Depositphotos
RayStation: Intelligent Planning for Complex Cases
Radiotherapy planning is a meticulous and iterative process that traditionally demands hours of expert time to achieve optimal tumor coverage while sparing organs at risk. RayStation, an advanced treatment planning system developed by RaySearch Laboratories, has incorporated artificial intelligence into this workflow, offering a transformative approach to dose optimization and beam arrangement. AI-powered planning in RayStation enables rapid generation of clinically robust plans, particularly in anatomically complex regions such as the head and neck, prostate, and spine.
One of the key innovations in RayStation is its integration of machine learning-based dose prediction models. These models are trained on large datasets of high-quality clinical plans and can predict the achievable dose distribution for a given anatomy. Based on this prediction, the AI engine automatically generates optimization objectives and beam configurations that match the patient’s clinical requirements. This process significantly reduces inter-planner variability and enables institutions to maintain consistent quality standards across staff and shifts.
In a notable study, Babier et al. (2020) evaluated the performance of AI-assisted radiotherapy planning using deep learning models trained on previously delivered plans. They found that the AI-generated plans were comparable—or even superior—to those created manually by experienced dosimetrists, particularly for prostate and oropharyngeal cancers. The plans achieved target coverage and organ-at-risk sparing in line with clinical guidelines, but in a fraction of the time required by traditional workflows (Babier et al., 2020).
RayStation’s AI module does not aim to replace planners, but rather to augment their capabilities. By front-loading the planning process with intelligent suggestions, clinicians can explore multiple plan options quickly and make well-informed decisions based on comparative data. This capability is particularly useful in institutions conducting adaptive planning, stereotactic body radiotherapy (SBRT), or proton therapy, where precision is critical and time is limited.
Another advantage of RayStation is its compatibility with multiple modalities, including photons, electrons, protons, and even carbon ion therapy. This makes it a versatile platform suitable for hybrid institutions or those involved in clinical trials where cross-modality planning is required. The AI engine learns continuously and can be refined over time using institutional data, further enhancing its adaptability to local practice patterns.
Ultimately, RayStation exemplifies the practical integration of AI into a core clinical task. It does not disrupt existing workflows but elevates them—accelerating turnaround times, improving plan quality, and allowing radiation oncologists to focus more on patient care and less on manual iteration.

Photo: Depositphotos
TheraPanacea ART-Plan: AI-Powered Automation for Adaptive Radiotherapy
Adaptive radiotherapy (ART) requires rapid recontouring, dose recalculation, and treatment plan generation—all within a narrow time window during a patient’s treatment session. TheraPanacea’s ART-Plan platform is one of the most advanced AI-driven systems addressing this need, offering a fully automated and vendor-neutral solution that streamlines ART workflows without compromising precision.
ART-Plan leverages deep learning models trained on high-quality, multi-center datasets to perform auto-segmentation of organs-at-risk (OARs), deformable image registration, and re-optimization of plans in near real time. The software is CE-certified and integrates easily with both linear accelerator systems and treatment planning software across vendors, making it accessible even in diverse clinical ecosystems.
One of ART-Plan’s distinguishing features is its ability to create synthetic CTs (sCTs) from cone-beam CT images using AI-based image synthesis algorithms. This is a crucial capability in MRI- or CBCT-guided adaptive therapy where direct dose calculation from on-board images is not feasible due to poor soft tissue contrast or inaccurate Hounsfield units. By generating sCTs with dosimetric accuracy equivalent to simulation CTs, ART-Plan enables rapid and reliable plan recalculation that is suitable for daily adaptation.
A multicenter study by Isambert et al. (2022) evaluated the clinical feasibility and accuracy of ART-Plan in head and neck cancers, where anatomical changes over treatment are frequent and impactful. The authors found that ART-Plan significantly reduced the time required for adaptation—from over 90 minutes manually to under 20 minutes using automation—without compromising target coverage or normal tissue sparing. The AI-generated contours were deemed clinically acceptable in over 95% of cases (Isambert et al., 2022).
Importantly, TheraPanacea’s ART-Plan platform is designed with explainability in mind. Clinicians can view the AI-generated outputs alongside confidence scores, uncertainty maps, and editable structures, allowing for quick verification and manual adjustment when needed. This transparent and human-in-the-loop approach fosters trust, which is essential in high-stakes oncologic care.
As adaptive therapy moves from academic centers into broader clinical practice, tools like ART-Plan will be essential to make daily adaptation feasible for routine patients—not just those enrolled in prospective trials. The system not only accelerates ART workflows but also expands access to this precision technology by removing vendor lock-in and enabling implementation across different radiotherapy infrastructures.
Photo: Depositphotos
Imbio Lung Suite and Radiomics Platforms: Bridging Imaging and Prognostics
As the field of radiation oncology continues to evolve, radiomics—an advanced imaging biomarker approach—has emerged as a powerful tool to personalize treatment beyond traditional anatomical and pathological variables. Platforms like Imbio Lung Suite and other AI-driven radiomics solutions are helping radiation oncologists extract quantitative, prognostically relevant data from standard imaging to guide therapy decisions, especially in thoracic malignancies.
Imbio Lung Suite is a clinically deployed AI platform that transforms high-resolution CT scans into automated reports highlighting lung density, emphysema patterns, airway metrics, and interstitial abnormalities. While initially developed for pulmonary fibrosis and COPD, the software has gained increasing attention in lung cancer radiotherapy. By evaluating background lung function and regional parenchymal quality, Imbio Lung Suite aids in optimizing radiation field design to reduce normal tissue toxicity.
In radiation planning for non-small cell lung cancer (NSCLC), accurate assessment of underlying lung condition is essential, particularly when high-dose treatments like stereotactic body radiotherapy (SBRT) are employed. A study by Maldonado et al. (2022) found that integrating AI-based lung texture analysis from Imbio significantly altered dose constraints and planning in a cohort of patients with borderline pulmonary reserve. The ability to visualize emphysema and fibrotic zones in 3D helped clinicians spare vulnerable regions and individualize treatment margins (Maldonado et al., 2022).
On a parallel track, radiomics platforms such as RadiomiX, TexRad, and AI-integrated research pipelines in tools like 3D Slicer or PyRadiomics enable the extraction of hundreds of quantitative features from medical imaging—texture, shape, heterogeneity, and more. These features can be correlated with genomic markers, treatment response, or survival outcomes, enabling the construction of predictive models that inform decision-making.
For example, in NSCLC patients undergoing chemoradiation, radiomic signatures extracted from baseline CT scans have been shown to predict local recurrence and overall survival independently of tumor stage (Aerts et al., 2014). These signatures may soon be integrated into clinical trials or adaptive protocols, allowing radiation dose to be escalated or de-escalated based on the tumor’s imaging phenotype.
While not yet fully integrated into all commercial radiotherapy systems, radiomics-driven models are being increasingly explored for:
- Differentiating pseudo-progression from true progression post-immunotherapy.
- Predicting toxicities such as radiation pneumonitis.
- Selecting patients for dose painting or hypofractionation.
One of the most promising aspects of radiomics is its potential synergy with other omics platforms—genomics, transcriptomics, and pathomics—to enable true precision oncology.
As Imbio Lung Suite becomes more broadly used and radiomics algorithms are validated in larger cohorts, these AI-based imaging tools will play an increasingly important role in personalizing treatment, predicting outcomes, and selecting patients for advanced radiation techniques.
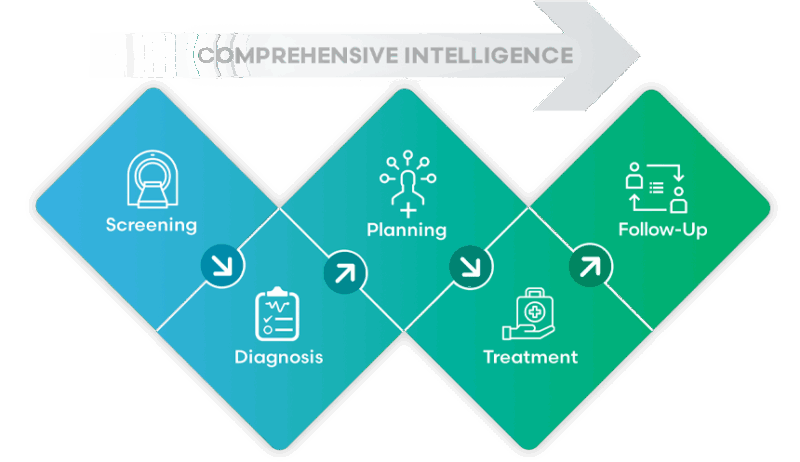
Photo: Depositphotos
The Era of Intelligence-Driven Radiation Oncology
Artificial intelligence is no longer a future promise in radiation oncology—it is a present reality, reshaping clinical workflows, improving treatment precision, and expanding the possibilities of personalized care. From MVision AI’s auto-contouring capabilities that streamline time-intensive tasks to Varian’s Ethos system, which brings real-time adaptive therapy into routine clinical practice, AI is addressing some of the field’s most pressing limitations.
RayStation’s AI-driven planning solutions demonstrate that consistent, high-quality plans can be achieved more rapidly and with reduced inter-operator variability, while TheraPanacea’s ART-Plan offers a vendor-neutral, fully automated adaptive platform that exemplifies the future of efficient and accurate daily adaptation. Meanwhile, imaging-based tools like Imbio Lung Suite and radiomics platforms are expanding the role of diagnostic imaging from anatomy to actionable prognostic insights, supporting a more intelligent form of treatment personalization.
Across all five platforms, the unifying theme is the ability of AI to assist—not replace—the clinician. These systems augment clinical judgment by accelerating routine steps, highlighting high-risk anatomical features, and surfacing treatment-relevant insights that might otherwise remain buried in imaging or dosimetric data. Importantly, their clinical validation is grounded in peer-reviewed studies, not theoretical models, ensuring safe integration into real-world practice.
As the technology continues to evolve, ongoing collaboration between engineers, clinicians, and researchers will be essential to ensure that AI tools remain interpretable, reproducible, and adaptable to the diverse needs of global oncology centers. Ethical deployment, data governance, and transparency in algorithm design must continue to be prioritized to maintain trust in these systems.
Ultimately, AI is enabling radiation oncologists to spend less time on technical minutiae and more time making strategic, patient-centered decisions. As institutions adopt these technologies, they are not only improving efficiency but also positioning themselves at the forefront of a new era—one where intelligent automation meets human expertise to deliver safer, more effective cancer care.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
