In the world of oncology, the roles of radiation oncologists, radiologists, and medical oncologists, clinical oncologists often spark confusion even for professionals. While these specialists work closely together to provide comprehensive care for patients, each has distinct training, responsibilities, and expertise. By understanding the unique functions and training paths of these professionals, we can appreciate the critical contributions each makes to the multidisciplinary approach to cancer treatment.
What is the difference between a Radiation Oncologist vs Radiologist vs Medical Oncologist
Let’s Understand in Simple Terms First who is who. When it comes to cancer treatment, different specialists play different roles. Think of a radiologist as the expert who takes pictures of the inside of your body, a radiation oncologist as the doctor who uses radiation to target and destroy cancer, and a medical oncologist as the one who uses drugs to treat cancer throughout the body. Each specialist is crucial, but they focus on different parts of the treatment process. Let’s break it down with a simple example using Mark, a cancer patient.
What is the difference between a radiologist and a radiation oncologist?
Imagine a patient named Mark, who was recently diagnosed with cancer. He needs radiation therapy to treat his tumor. A radiation oncologist will create a treatment plan, determining the amount of radiation, the precise area to target, and the number of treatment sessions. Meanwhile, a radiologist will interpret Mark’s imaging scans—like CT or MRI scans—to assess the tumor’s size, shape, and location. While both play essential roles, the radiologist focuses on diagnosis through imaging, whereas the radiation oncologist uses this information to guide radiation therapy.
What is the difference between an oncologist and a radiation oncologist?
After diagnosis, Mark also consults a medical oncologist. While the radiation oncologist focuses on localized treatment using radiation, the medical oncologist looks at the bigger picture, using systemic therapies like chemotherapy, immunotherapy, or targeted drugs to attack cancer cells throughout Mark’s body. The radiation oncologist’s role is more specific—delivering focused radiation to shrink the tumor or destroy cancer cells in targeted areas—while the medical oncologist manages systemic treatments affecting the whole body.
What exactly does a radiologist do?
A radiologist is a medical doctor who specializes in diagnosing diseases and injuries using medical imaging techniques. Their expertise includes a variety of imaging modalities, such as:
- X-rays: Now mainly used for examining bones and detecting fractures or infections in various organs.
- Computed Tomography (CT): Provides cross-sectional images of the body to assess conditions in various organs.
- Magnetic Resonance Imaging (MRI): Uses magnetic fields to produce detailed images of soft tissues, including the brain and muscles.
- Ultrasound: Employs sound waves to visualize internal organs, joints,muscles,skin etc.
- Nuclear Medicine: Involves the use of small amounts of radioactive material to diagnose diseases.
Radiologists interpret these images to identify abnormalities, and recommend further testing. They play an important role in the multidisciplinary team approach to patient care, often collaborating with other specialists to provide comprehensive diagnosis and management.
What exactly does a medical oncologist do?
A medical oncologist is a physician who specializes in treating cancer using non-surgical approaches. Their primary focus is on the use of systemic therapies, which include:
- Chemotherapy: The use of drugs to kill cancer cells or stop their growth.
- Immunotherapy: Treatments that help the immune system recognize and attack cancer cells.
- Targeted Therapy: Drugs designed to target specific characteristics of cancer cells, such as genetic mutations.
- Hormone Therapy: Treatments that block hormones that fuel certain cancers, such as breast and prostate cancer.
Medical oncologists are involved in the overall management of cancer patients, from initial diagnosis through treatment and into survivorship. They work closely with other specialists, such as surgeons and radiation oncologists, to create a comprehensive treatment plan. Additionally, they monitor patients for side effects, manage symptoms, and provide supportive care throughout the treatment process. Their role is important in ensuring that patients receive personalized and effective cancer care.
What exactly does a clinical oncologist do?
A clinical oncologist is a medical professional who specializes in the diagnosis, treatment, and management of cancer, particularly focusing on non-surgical approaches.
Clinical oncologists often work as part of a multidisciplinary team, collaborating with surgeons, medical oncologists, radiologists, and other specialists to create comprehensive treatment plans for cancer patients. Their training involves a background in medicine followed by specialized training in oncology and the various cancer treatment modalities.
Countries where Clinical Oncology is a Specialty
- United Kingdom (UK): In the UK, clinical oncologists are trained in both radiotherapy and chemotherapy. They typically lead cancer treatment teams and play a central role in cancer care.
- Australia and New Zealand: Clinical oncologists in these countries also focus on both radiotherapy and chemotherapy, managing the overall treatment of cancer patients.
- Canada and Ireland: Like in the UK, clinical oncologists are key specialists in cancer care, particularly in radiotherapy and systemic therapies.
- United States: In the U.S., the field is typically divided into medical oncologists (who primarily focus on chemotherapy and systemic therapies) and radiation oncologists (who specialize in radiotherapy). The combination of these roles is less common, but some practitioners may cross-train in both areas.
- India: In India, clinical oncologists can be found managing cancer treatments across a range of methods, often in conjunction with medical oncologists and surgeons.
- Germany and other European countries: In much of Europe, oncology is similarly divided into clinical, medical, and surgical specialties, with clinical oncologists focusing on non-surgical treatments, particularly radiotherapy.
What exactly does a radiation oncologist do?
A radiation oncologist is a medical doctor who specializes in the use of radiation therapy to treat cancer. Radiation therapy involves the precise delivery of high-energy radiation, often in the form of X-rays or particles such as electrons, protons to kill cancer cells or inhibit their ability to grow and divide. Radiation oncologists play a huge role in the multidisciplinary approach to cancer treatment, working alongside other specialists such as medical oncologists, surgical oncologists, and radiologists.
The primary responsibility of a radiation oncologist is to manage the planning and administration of radiation therapy. This process involves several steps:
Consultation and Diagnosis
The radiation oncologist meets with the patient to evaluate their medical history, review imaging studies (like CT scans, MRIs, or PET scans), and conduct a physical examination. The radiation oncologist also works with pathologists to understand the specific type of cancer and its stage. Based on this information, the radiation oncologist determines if radiation therapy is appropriate and beneficial.
Treatment Planning
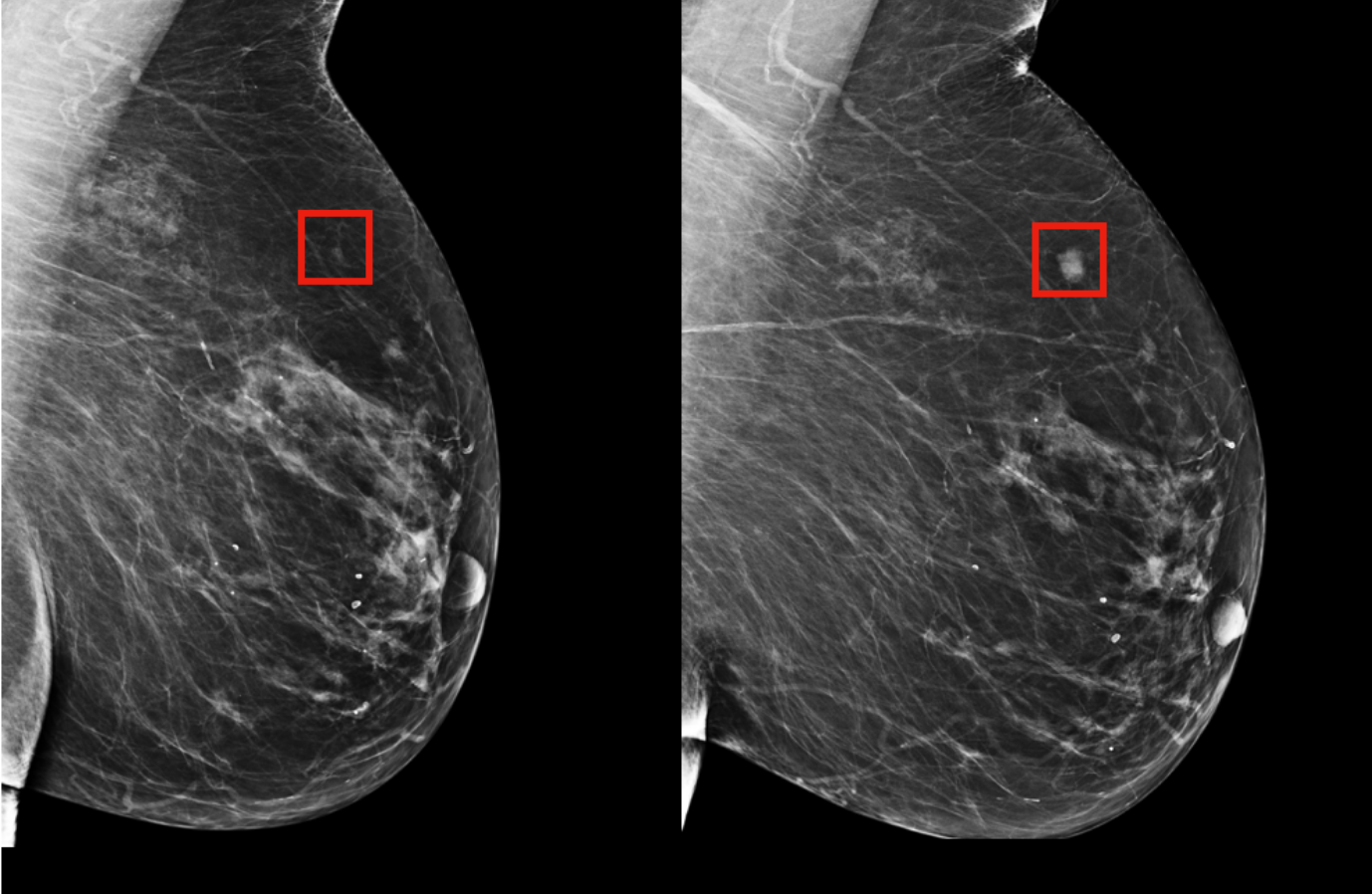
- CT simulation is a critical step in radiation therapy planning, used to precisely map out the area to be treated. During this procedure, the patient undergoes a CT scan in the same position they will be in for treatment. The images generated provide a detailed, 3D view of the tumor and surrounding anatomy.
- Using these images, radiation oncologists and medical physicists create a customized treatment plan, determining the exact location, size, and shape of the tumor. They also identify critical structures, or organs at risk, that need to be protected from excessive radiation. The CT simulation ensures accurate targeting during radiation therapy, enhancing treatment effectiveness and minimizing side effects.
- In addition to their broader responsibilities, an important part of a radiation oncologist’s work involves contouring during the treatment planning process. Contouring refers to the precise delineation of areas within the patient’s body that will receive radiation, as well as the identification of areas that need to be protected from radiation exposure (known as organs at risk, or OARs). This is a vital step in the planning process because it directly affects the success of the treatment and the reduction of potential side effects.
Can AI Replace Radiation Oncologists?
While Artificial Intelligence (AI) is making significant strides in healthcare, the idea of AI completely replacing radiation oncologists is far from reality. AI is indeed a powerful tool, but it functions best as an assistant—not a replacement—for human expertise. Here’s why AI, despite its advancements, cannot fully take over the critical role that radiation oncologists play in cancer care.
source: MIT News
AI is transforming key aspects of radiation oncology, such as treatment planning and tumor contouring. For example, AI-based platforms like Mirada Medical’s ContourAI are already assisting radiation oncologists by automating the delineation of tumor boundaries in imaging scans. This can save hours of manual work, allowing oncologists to focus on refining the treatment plan. However, AI lacks the ability to make the critical clinical decisions that are necessary for each individual patient.
Consider a case where a patient has multiple comorbidities or an unusual tumor location. AI can analyze scans and suggest treatment pathways based on historical data, but it cannot interpret complex medical histories or adapt to unpredictable patient responses. For instance, in cases of head and neck cancers, where tumors are often located near critical structures like the brain and spinal cord, the radiation oncologist must carefully weigh the risks and benefits of various treatment options. AI lacks the ability to make these nuanced, real-time decisions that often require collaboration with other specialists, such as surgeons or medical oncologists.
During radiation therapy, complications can arise, such as unexpected tumor shrinkage or organ movement that affects the treatment area. Technologies like Varian’s Ethos™ adaptive radiation therapy system utilize AI to adjust treatments in real-time based on daily imaging, but these adjustments still require the expertise of a radiation oncologist to ensure accuracy and safety. AI can provide options, but it’s the oncologist who decides the best course of action for the patient.

Beyond technical skills, radiation oncologists provide compassionate care that AI simply cannot replicate. Imagine a patient who is undergoing radiation therapy for the first time and is anxious about potential side effects. A radiation oncologist can explain the process, reassure the patient, and adjust treatment to manage side effects like fatigue or skin irritation. AI may help predict outcomes or recommend treatment protocols, but it cannot communicate empathetically or offer personalized advice in response to a patient’s fears and concerns.
In recent years, AI-driven tools like DeepMind’s AlphaFold have contributed significantly to understanding protein structures that could aid cancer treatments, but these tools enhance the oncologist’s ability to target cancer, not replace it. Similarly, IBM Watson for Oncology has shown potential in suggesting treatment options by analyzing massive datasets, but it still requires oncologists to interpret those suggestions in the context of a patient’s unique situation.
Written by Aren Karapetyan, MD