Pancreatic ductal adenocarcinoma (PDAC) remains one of the most lethal malignancies in oncology. Despite decades of therapeutic advances, overall survival across all stages remains dismal, with a median survival of approximately four months and more than 467,000 deaths worldwide annually (Bray et al., 2024; Stoop et al., 2025). The reason is painfully consistent: pancreatic cancer is usually diagnosed too late.
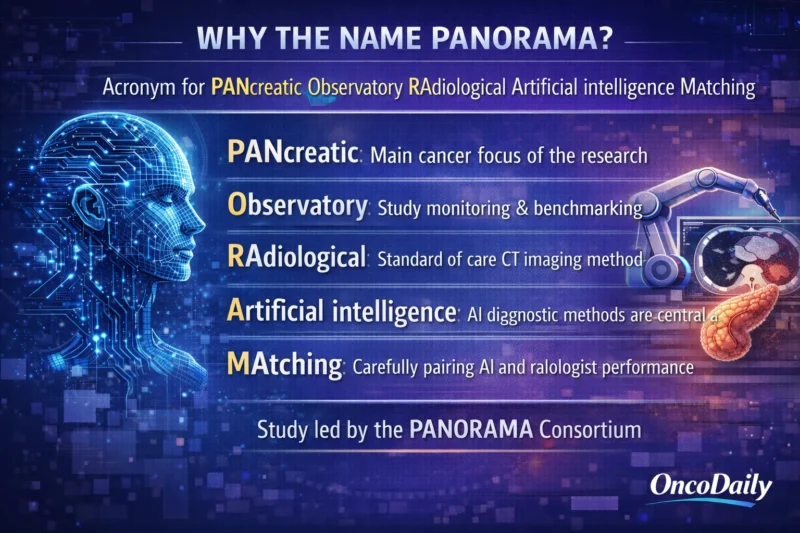
The PANORAMA study, published in The Lancet Oncology in 2026, challenges a long-standing diagnostic limitation. It asks whether artificial intelligence can detect pancreatic cancer on routine contrast-enhanced CT scans more accurately than radiologists (Alves et al., 2026).
The findings are not incremental. They are disruptive.
Why Early Detection of Pancreatic Cancer Remains So Difficult
Pancreatic cancer rarely produces symptoms in early stages. By the time clinical signs appear, the disease is often locally advanced or metastatic. Surgical resection remains the only potentially curative treatment, yet only a minority of patients are diagnosed early enough to qualify. Even among those undergoing resection, median survival reaches approximately 32 months, compared to just months in advanced disease (Conroy et al., 2023; Mackay et al., 2024).
Contrast-enhanced CT in the portal venous phase is the recommended first-line imaging modality for pancreatic cancer detection, endorsed by ESMO and other major radiology societies (Conroy et al., 2023; Al-Hawary et al., 2014). Yet interpretation of CT imaging is complex. Small tumors can blend into pancreatic parenchyma. Indirect signs such as duct dilation or subtle contour abnormalities may be overlooked. Inter-reader variability is well documented (Singh et al., 2020; LeBlanc et al., 2023).
This diagnostic vulnerability is precisely where the PANORAMA study intervenes.
What the PANORAMA Study Was Designed to Prove
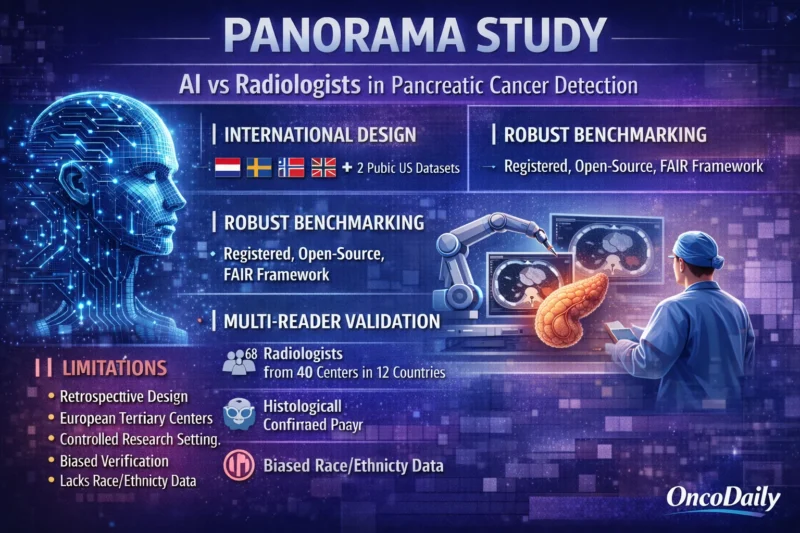
The PANORAMA study, Artificial Intelligence and Radiologists in Pancreatic Cancer Detection Using Standard-of-Care CT Scans, was not a small pilot investigation. It was structured as a large, international, paired, confirmatory diagnostic accuracy study.
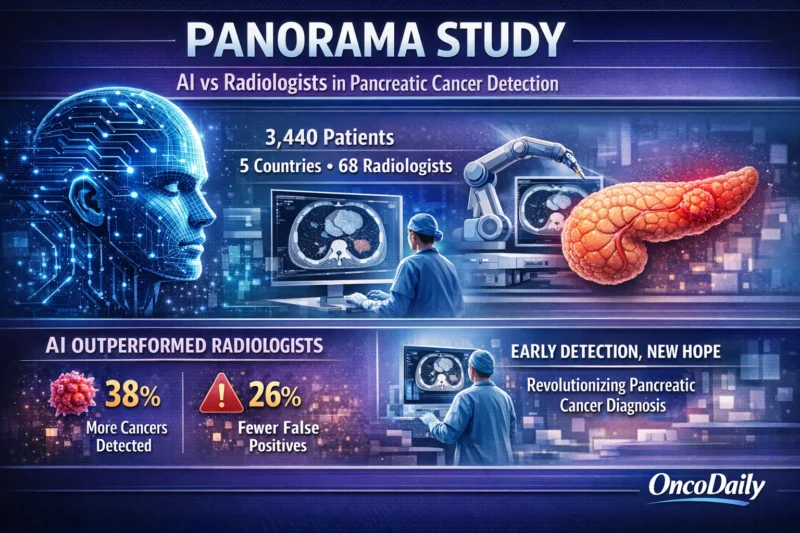
The dataset included 3,440 patients collected between 2004 and 2023 across five European tertiary centers and two US public datasets. Among them, 1,103 cases of pancreatic ductal adenocarcinoma were histologically confirmed.
The study was divided into two major components. First, an international AI grand challenge invited global developers to train and benchmark algorithms. Second, a multi-reader study involved 68 radiologists from 40 centers across 12 countries. The goal was not theoretical model performance, it was direct comparison.
The primary endpoint was the area under the receiver operating characteristic curve (AUROC), a standard measure of diagnostic discrimination.
Importantly, the study followed STARD-AI, STROBE, and BIAS reporting frameworks, and was pre-registered for transparency (Maier-Hein et al., 2020; Sounderajah et al., 2020; von Elm et al., 2008). In a field often criticized for benchmarking inconsistencies (Mahmood, 2025), the methodological rigor of the PANORAMA study stands out.
How the AI Was Trained and Validated
The AI component of the PANORAMA study used a carefully structured training and testing design. A total of 2,224 patients were used for model training and 86 for tuning. The final performance was evaluated in a completely sequestered external test set of 1,130 patients.
Crucially, pancreatic cancer cases were confirmed histologically, and negative controls required either histopathologic confirmation or at least three years of follow-up to exclude missed malignancy.
The final AI model was an ensemble of the top three performing algorithms from the international challenge.
On the independent test cohort, the AI achieved an AUROC of 0.92 (95% CI 0.90–0.93), with a sensitivity of 85.7% and specificity of 83.5%.
These results alone suggest high diagnostic performance. But the true test was comparison with human readers.
AI Versus Radiologists: Direct Comparison
In the reader study, 68 radiologists evaluated 391 CT scans, including 144 confirmed pancreatic cancer cases. The pooled radiologist performance yielded an AUROC of 0.88 (95% CI 0.85–0.91).
When evaluated on the same dataset, the AI achieved an AUROC of 0.92 (95% CI 0.89–0.94). The PANORAMA study demonstrated not only statistical non-inferiority (p<0.0001), but statistical superiority (p=0.001).
At matched specificity, AI detected 38% more cancers than radiologists. At matched sensitivity, AI reduced false positives by 26%. These are not marginal gains. In a disease where early detection can mean the difference between resection and palliation, such improvements are clinically meaningful.
Why the PANORAMA Study Is Different From Previous AI Reports
Many prior AI publications in pancreatic imaging have been limited by small datasets, single-center design, or lack of external validation. Some included fewer than 1,000 patients. Others lacked formal reader comparisons.
The PANORAMA study addressed these weaknesses directly. It used a large multicenter dataset, international benchmarking, and transparent statistical planning. It also established a FAIR (Findable, Accessible, Interoperable, Reusable) framework, enabling reproducibility.
This matters. AI research has faced criticism for lack of generalizability and inconsistent reporting standards. The PANORAMA study sets a methodological benchmark that future diagnostic AI systems must now meet.
Could This Enable Opportunistic Screening?
Contrast-enhanced CT scans are performed widely for numerous abdominal indications. Estimates suggest that 40–52% of CT imaging globally uses portal venous phase protocols (Berrington de Gonzalez & Kleinerman, 2015; Dekker et al., 2022).
This creates a provocative possibility: AI could evaluate existing scans for early pancreatic cancer detection without additional radiation exposure or dedicated screening programs.
The authors of the PANORAMA study cautiously raise this prospect. However, they also acknowledge the risks of overdiagnosis and downstream economic burden (Alshybani, 2024). Prospective implementation studies will be required before integration into clinical workflow.
Important Limitations
The PANORAMA study is retrospective, and most data originated from European tertiary centers. Reader evaluations occurred in controlled settings without full clinical context such as laboratory data, prior imaging, or multidisciplinary discussion.
Therefore, performance reflects stand-alone interpretation rather than complete real-world diagnostic pathways. Additionally, race and ethnicity data were not available, limiting subgroup analysis of algorithm equity. Despite these limitations, the scale and rigor of the study provide strong evidence.
Does This Replace Radiologists?
No.
The PANORAMA study evaluated AI as a stand-alone system to establish benchmark performance. Real-world integration will likely involve AI-assisted interpretation rather than replacement.
Evidence from other domains, such as prostate MRI (Saha et al., 2024) and mammography (Lång et al., 2023), shows that AI can safely reduce workload while maintaining diagnostic accuracy. In pancreatic cancer detection, AI may serve as a second reader, a triage tool, or a safety net for subtle lesions.
The future is augmentation, not substitution.
Why the PANORAMA Study Matters
Pancreatic cancer has long been described as a medical emergency (Lancet Gastroenterology & Hepatology, 2021). Therapeutic advances alone have not meaningfully shifted survival curves. The PANORAMA study introduces a new variable into that equation: earlier detection through artificial intelligence.
By demonstrating superiority over pooled radiologist performance in a rigorous, confirmatory design, the PANORAMA study does more than publish impressive metrics. It changes the conversation. If validated prospectively, AI-supported CT interpretation could move pancreatic cancer detection earlier on the timeline, where surgery is possible, and survival is measurable in years rather than months.
The question is no longer whether AI can match radiologists in pancreatic cancer detection. The PANORAMA study suggests it can exceed them. The next question is whether healthcare systems are ready to use it.
Written by Armen Gevorgyan, MD