At MASCC 2025, Dr. Fumiko Chino—radiation oncologist, health policy expert, and former cancer widow—delivered a powerful plenary session on the global impact of financial toxicity and the evidence-based solutions being implemented across systems.
What Is Financial Toxicity and Why Does It Matter?
Financial toxicity refers to the problems patients face related to the cost of medical care. Dr. Chino emphasized that even insured patients can face devastating economic hardship, citing a 2018 ASCO National Cancer Opinion Survey that revealed widespread financial burden among cancer survivors. According to the National Cancer Institute, cancer patients are significantly more vulnerable to financial toxicity than the general population.
In the U.S., the annual patient economic burden of cancer—including out-of-pocket (OOP) and time costs—is approximately $21.1 billion (Yabroff, JNCI 2021).
Financial toxicity leads to:
- Decreased quality of life, with patients reporting more anxiety, fatigue, and poorer physical and social functioning (Zafar, Fenn, Ver Hoeve).
- Decreased satisfaction and trust in care, with many patients doubting their physician’s diagnosis or competence (Chino, Oncologist 2014).
- Decreased quality of care, including 27% nonadherence to medications due to cost.
- The Personal and Societal Toll
Dr. Chino presented alarming statistics:
Three out of four patients experience major financial hardship within one year of diagnosis, even with insurance (Shankaran, JNCI 2021).
Cancer survivors report long-term harms, including:
- 44% decrease in credit score
- 39% contacted by debt collectors
- 45% incurred credit card debt or deferred major purchases
The consequences of this financial strain are dire:
- A 2.65x higher risk of bankruptcy following a cancer diagnosis (Ramsey, Health Affairs 2013)
- A 79% increased mortality risk associated with post-diagnosis bankruptcy (Ramsey, JCO 2016)
Global Perspectives: Financial Toxicity Beyond the U.S.
Financial hardship is not limited to the U.S. In countries with universal healthcare, out-of-pocket costs and lost income still generate distress:
- Out-of-pocket costs: $17–506/month
- Travel costs: up to $393/month
- Financial stress reported by 41–48% of patients (Longo, 2020)
In LMICs, the burden is catastrophic. In Nigeria, where the average income is $2,640/year, cancer diagnosis and treatment costs $2,049, leading to catastrophic health expenditures for over 90% of patients (Knapp, PAMJ 2022). Families are often forced to withdraw children from school.
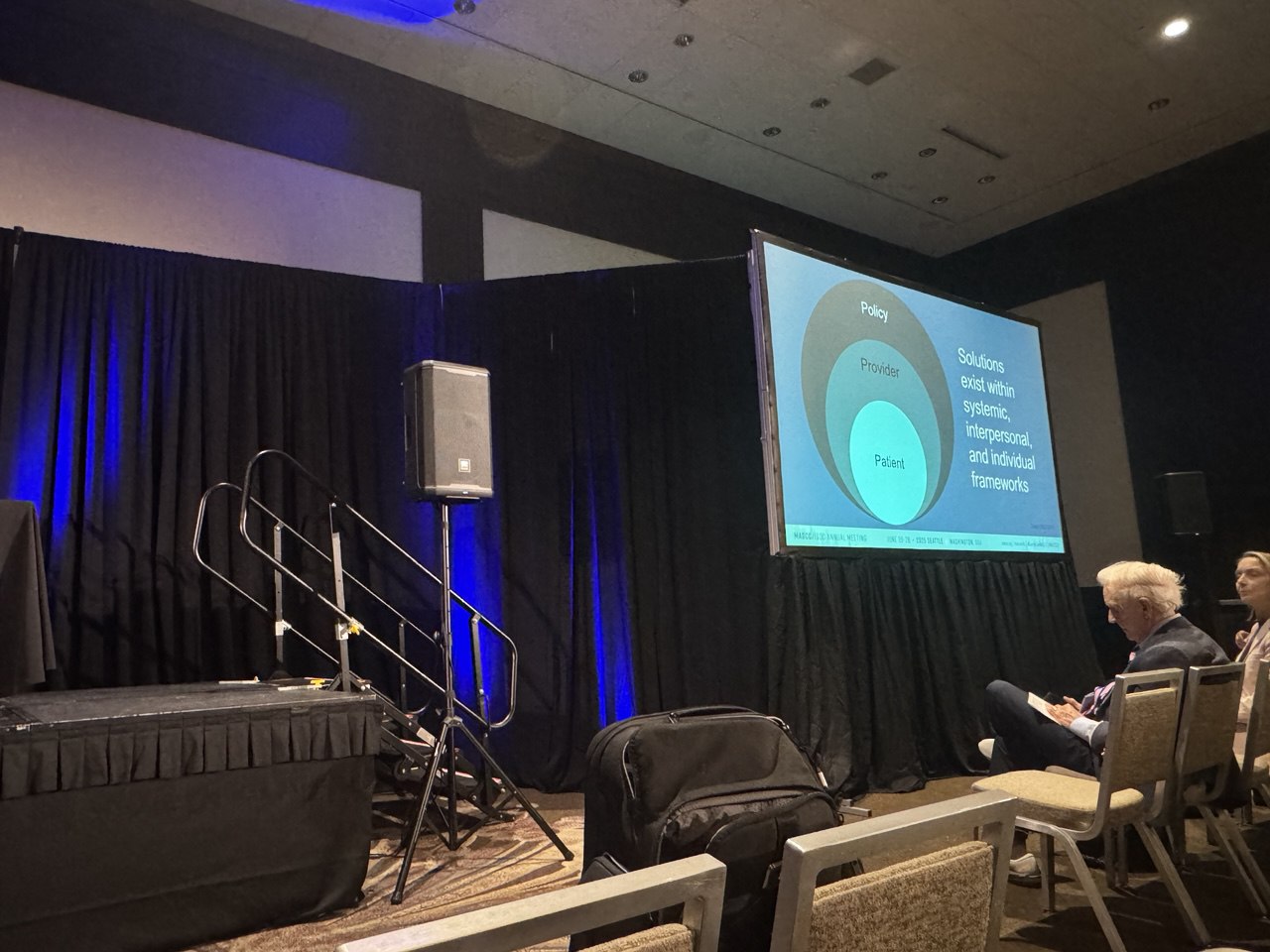
Solutions: From System to Clinic
Dr. Chino outlined actionable interventions at the systemic, interpersonal, and individual levels:
National Initiatives:
- Health insurance expansion (Jemal, JCO 2017)
- Choosing Wisely campaigns (ASCO, ASTRO, SSO)
- Price transparency (Chino, JAMA Onc 2021) — where drug prices ranged from $297 to $33,411 at NCI-designated centersClinical Interventions:
- Upfront financial counseling improved understanding of OOP costs in 88% of patients (Kircher, JOP 2018)
- App-based navigation tools significantly increased financial assistance applications and receipt (Tarnasky, JOP 2021)
- The PRO-TECT trial showed that nurse navigators, pharmacists, and social workers improved outcomes through coordinated financial screening and intervention
Telemedicine and logistical support:
- 66% of patients found telemedicine more affordable than in-person visits (Shaverdian, JNCCN 2021)
- Practical supports like free parking, transportation, and shorter wait times could dramatically reduce financial stress
Training and Cultural Change Needed
A critical barrier remains: providers are not trained to discuss costs. According to Chino and Aviki’s 2022 study, most oncologists acknowledge affordability contributes to care quality, but fewer feel equipped to address it. In fact, 96.3% of recent medical graduates reported insufficient training in affordability and healthcare costs (Bell, JACR 2023).
Conclusion
Dr. Fumiko Chino’s presentation at MASCC 2025 called for urgent action—from national policy to individual clinical practice—to mitigate financial toxicity in cancer care. With evidence-based tools, better education, and system-level alignment, the oncology community has the power to turn data into meaningful change for patients facing not only cancer—but the cost of surviving it.