Skin cancer is the most common and fastest growing cancer type globally, with melanoma causing the majority of skin cancer deaths. Each year, millions are diagnosed, and the frequency continues to rise, presenting a major public health burden. According to the American Cancer Society, in 2025 more than 100000 new melanoma cases will be diagnosed in the United States alone, and about 8000 diagnosed patients are expected to die, majority of them being men. Alarmingly, every hour, nearly two people die of melanoma in the U.S. These statistics highlight the critical need for improved surveillance and early detection strategies (American Cancer Society, Key Statistics for Melanoma Skin Cancer, 2025).
Total Body Photography and Automated Lesion Mapping are emerging as powerful tools to enhance early detection and continuous monitoring of skin cancer, improving patient outcomes.
Photo:Depositphotos
How to Improve Survival Outcomes in Melanoma?
As with many cancers, early detection is the cornerstone of effective melanoma management. When caught in its earliest stages, melanoma has a five-year survival rate of up to 99%. (American Cancer Society, Key Statistics for Melanoma Skin Cancer, 2025). There are two main approaches used for early detection: population-based screening and targeted screening. Population-based screening includes everyone regardless of individual risk. While comprehensive, this method can impose a substantial financial burden on healthcare systems due to the large number of low-risk individuals screened. In contrast, targeted screening focuses on individuals at increased risk of developing melanoma, such as those with a family history, numerous or atypical moles, or fair skin—resulting in a higher prevalence of diagnosed cases.
This technique is widely used and prioritized, as it can improve early melanoma detection rates, enhance patient outcomes, and optimize the use of healthcare resources (Hornung A, et al. Int J Environ Res Public Health. 2021).
What is Skin Surveillance and Why is it Important?
Skin surveillance facilitates the timely identification and monitoring of suspicious or changing lesions. This is especially critical in melanoma, where early diagnosis can be lifesaving. The 5-year relative survival rate for melanoma skin cancer is approximately 95% overall, reaching nearly 100% when detected at a localized stage before spreading. However, survival drops significantly with regional or distant spread, underscoring the vital role of early detection through systematic surveillance (SEER Cancer Stat Facts: National Cancer Institute, 2025).
Certain populations—including individuals with lighter skin tones, those with intense or repeated sun exposure or sunburns, persons with personal or family history of skin cancer, certain racial and ethnic groups, and immunosuppressed patients—are at higher risk for aggressive skin malignancies, making surveillance critical for these vulnerable groups (Erdmann et al.,Int J Environ Res Public Health, 2021).
Moreover, evidence shows that melanoma detected during routine skin checks by healthcare professionals reduces mortality risk by 32% compared to self-detection, highlighting the life-saving impact of proactive skin monitoring (Melanoma Institute Australia, 2021). As skin cancer rates continue to rise, with over 212,000 new cases of melanoma expected in the U.S. in 2025 alone, skin surveillance remains an essential public health measure for early intervention and improved outcomes.
What’s Missing in Traditional Skin Exams?
Traditional visual examination and dermoscopy are key components of detecting skin cancer and have been used as a primary diagnosing tool for many years. Despite the availability of various detection methods, routine skin surveillance still depends on visual assessments, but these methods have their limitations.
Visual exams are often the first step, but they can vary a lot depending on the doctor’s experience and judgment. Dermatologists assess lesions based on features such as shape, color, and size changes, but the subtle resemblance between benign and malignant lesions often makes it challenging to differentiate between the two. This leads to variability in diagnostic accuracy, potential missed diagnoses of early or atypical cancers, and unnecessary biopsies of benign lesions, increasing patient burden and healthcare costs.

Photo:Depositphotos
Dermoscopy is a newer method, which enhances the clinical exam by magnifying lesion details and revealing sub-surface structures, improving diagnostic precision. However, this diagnostic method requires a trained specialist with significant experience in pattern recognition. Deramoscopy may not picture deeper structures as it allows visualization of a given skin lesion only to the level of the papillary dermis. Furthermore, dermoscopy is time-consuming and may be less practical for patients with numerous lesions and limited mobility (Arige S. et al., Biomed Pharmacol J. 2025; Jennifer Y. Chen et al, JAMA Dermatology, 2025).
This is why the field is rapidly advancing in new diagnostic technologies like total body photography and automated lesion mapping, which promise to transform skin cancer screening and follow-up by increasing accuracy, reproducibility, and efficiency.
What is Total Body Photography (TBP)?
Total Body Photography, also known as Whole-Body imaging or mole mapping, is an advanced, non-invasive diagnostic tool used to detect skin cancer. This technique creates a comprehensive visual record of a patient’s skin, from head to toe, by taking high-resolution images of the entire skin surface. These records are often stored, allowing clinicians to compare subsequent images to the baseline to identify changes.
TBP is done by trained nurses, who guide patients to standing in standardized poses while the machine takes the pictures. This step takes typically 15-30 minutes and provides high-resolution images that are stored to create a digital map of skin, where every mole and discoloration is sized and stored. Review of this map is done by dermatologists and AI technologies (Melanoma Institute Australia, 2022; The Woods Medical Centre, 2025).

Photo of TBP procedure -(Machine by Canfield Scientific)
Total Body Photography (TBP) can be performed for nearly anyone, but it is particularly recommended for people with a high number of moles (generally over 100), moles that are unusually large, irregular in shape or color, or located in areas that are hard to monitor, such as the back. TBP offers a visual and objective approach to tracking skin changes.
How have TBP Machines Progressed?
The origins of Total Body Photography (TBP) date back to the 1990s, when imaging involved a patient standing against a plain wall while a specialist manually captured photographs using a flash camera. These images were stored in patients’ medical records for longitudinal review by dermatologists (DermEngine, 2019). Over time, TBP evolved from this 2D clinical photography approach, which required manual posing that was time-consuming, challenging for patients with limited mobility, and labor-intensive (A. Ferreirinha et al., Actas Dermosifiliogr, 2025).
Future advancements led to 3D TBP systems that rapidly and automatically capture high-resolution, standardized whole-body images within seconds, overcoming many limitations of traditional 2D photography. For example, the VECTRA WB360 system uses 92 cameras arranged around the patient to produce a detailed 3D skin surface model within a few seconds, while 2D systems could take up to an hour. (Clare A Primiero et al., Frontiers in Medicine, 2024). These modern 3D systems capture both color images and depth data simultaneously, enabling accurate representation of natural skin contours and folds, which improve lesion visualization and monitoring, particularly in difficult-to-photograph areas.
More recently, automated total body mapping integrated with artificial intelligence (AI) has emerged to enhance lesion detection accuracy and reduce diagnostic variability (A. Ferreirinha et al., Actas Dermosifiliogr, 2025).
Can AI Detect Skin Cancer?
Artificial intelligence (AI), particularly through convolutional neural networks (CNNs), has become an effective tool across medical specialties—including radiology, cardiology, ophthalmology, and dermatology (Bohr et al., Artificial Intelligence in Healthcare, 2020). Sometimes, AI use in dermatology has even outperformed individual specialists in identifying melanoma, as a study from 2017 suggest:
“A single deep convolutional neural network, trained end-to-end on a large dataset of clinical images, can classify skin lesions—including keratinocyte carcinomas and melanoma—with accuracy comparable to that of 21 board-certified dermatologists.” – Andre Esteva et al., Nature, 2017.
Recent research has also increasingly supported the use of Artificial Intelligence (AI) and its algorithms in enhancing skin cancer detection, particularly when combined with Total Body Photography (TBP). A notable 2024 study conducted across two clinical centers gathered comprehensive clinical data, including thousands of TBP images alongside detailed patient-level metadata such as individual risk factors and phenotypic characteristics. This rich dataset was annotated to facilitate the development and validation of AI-based tools capable of providing a holistic assessment — not only of individual skin lesions but also of overall patient risk profiles (Clare A Primiero et al., Frontiers in Medicine, 2024).
The study outcomes showed that AI assistance significantly improved diagnostic accuracy in skin cancer detection across healthcare practitioners of all levels, increasing both sensitivity and specificity. Practitioners using AI guidance diagnosed skin cancers with about 81.1% sensitivity and 86.1% specificity, compared to 75% sensitivity and 81.5% specificity without AI. The greatest benefit was observed in non-specialists such as primary care doctors and nurse practitioners, who improved diagnostic accuracy by approximately 11-13 percentage points with AI support. These results demonstrate AI’s potential to enhance skin cancer detection accuracy, reduce diagnostic errors, and support clinicians in early melanoma identification and monitoring when integrated with advanced TBP imaging (Krista Conger, Stanford Medicine, 2024).
FDA-Approved AI Devices For Skin Cancer Detection
The first AI-enabled medical device authorized by the FDA for skin cancer detection in primary care is DermaSensor. This device assists non-specialists in assessing suspicious skin lesions for melanoma, basal cell carcinoma, and squamous cell carcinoma in patients aged 40 and older. It has a sensitivity of about 95.5%, higher than primary care physicians alone, but comparatively lower specificity (~20.7%), which may result in more false positives (Laura K Ferris et al., J Prim Care Community Health. 2025; Kaushik P. Venkatesh et al, npj Digital Medicine, 2024).
Other FDA-approved AI dermatology devices include MelaFind and NeviSense, which are specialized tools primarily used by dermatologists. MelaFind, approved via the Premarket Approval (PMA) pathway, was discontinued due to low specificity causing unnecessary biopsies. NeviSense remains on the market with high sensitivity but also relatively low specificity (Nahm WJ et al., Int J Dermatol., 2025; Useini V et al., Sci Rep., 2024).
What Are the Challenges with AI in Dermatology?
While artificial intelligence offers valuable opportunities for dermatology, several important challenges remain. One major issue is bias in the training datasets, many of which underrepresent people with darker skin tones and can lead to reduced diagnostic accuracy and widen existing disparities in care. Another concern is the lack of transparency in how most AI systems actually work. Deep learning models often function like “black boxes,” making it hard for clinicians to understand or explain why a particular recommendation was made.
This can make it harder to build trust and slows down clinical adoption. Generalizability is also a real challenge. AI tools that perform well in one setting might not work as accurately in another—especially if the population, skin types, or imaging methods differ. Even beyond the technology itself, there are practical barriers to using AI in everyday practice.
These include the need for large, well-annotated datasets, patient privacy concerns, high development costs, and the difficulty of integrating new tools into existing clinical workflows. Moving forward, it will be important to focus on building AI systems that are not only accurate, but also ethical, transparent, and easy to use. That means training models on diverse populations, making them interpretable for clinicians, and ensuring they can be smoothly integrated into real-world care (Farheen Tafti et al., IP Indian Journal of Clinical and Experimental Dermatology, 2025; Andrzej Grzybowski et al., Clinics in Dermatology, 2024).
What is Automated Lesion Mapping?
Automated lesion mapping (ALM) refers to the use of software tools to identify, label, and track skin lesions—such as moles—across the entire body. It is often implemented through total body photography or other imaging techniques. These systems generate a visual “map” of skin lesions, either on a digital body model or 2D schematic, enabling clinicians to monitor the number, size, shape, and location of lesions over time. This visual documentation supports early detection of suspicious changes and enhances long-term follow-up care (Bell Raj Eapen et al., JMIR Dermatol 2020; Zhouxiao Li et al., J Clin Med. 2022).

Images from the Vectra 3D Skin Imaging System, source The University of Queensland , Australia.
To better understand the value of ALM in total body imaging, it is helpful to consider how skin cancer is typically diagnosed without such technology. Dermatologists rely on a wide range of descriptive terms to classify skin lesions, assessing characteristics such as color, shape, size, location, and distribution. In the case of melanoma, diagnosis often follows the widely adopted ABCDE rule: A for asymmetry, B for border irregularity, C for color variation, D for diameter (typically >6mm) and E for Evolving (American Cancer Society, 2025).
While this method is effective, it is time-consuming—especially considering that the average person has up to 40 moles (National Cancer Institute, 2022). For a single patient, manually documenting and evaluating each lesion across the body can take hours, even for experienced dermatologists.
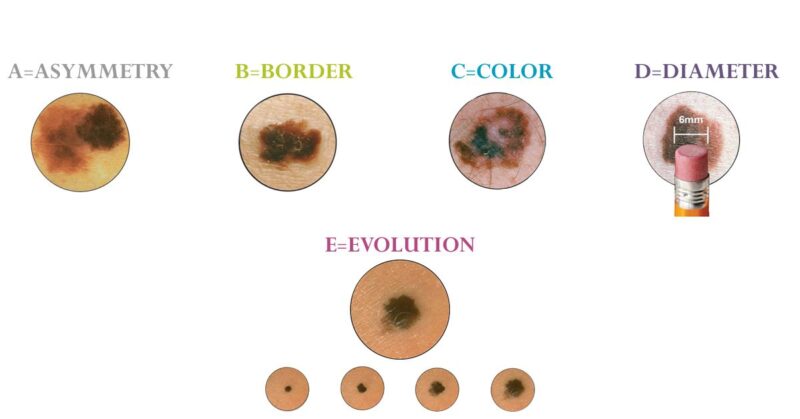
Photo: Iamatmelanoma.org
This is where artificial intelligence (AI) plays a transformative role. A recent literature review by Zhouxiao Li and colleagues (2022) systematically analyzed studies across multiple databases focusing on AI-assisted image analysis in dermatology. Authors note that AI systems can analyze skin lesion features more efficiently and objectively than human observers. Morphological terms commonly used by dermatologists can be annotated and fed into specialized databases allowing AI tools to recognize and retrieve information about previously documented lesions within seconds (Zhouxiao Li et al., J Clin Med. 2022).
What are the Benefits of TBP over Traditional Skin Exams?
The integration of Total Body Photography (TBP) with Automated Lesion Mapping (ALM) offers many clinical benefits, making it a highly valuable tool for skin cancer detection and monitoring in dermatology practices.
- Early detection: This is the key factor determining survival rate of melanoma patients. By analyzing the whole body, TBP facilitates the early detection of quiet killers in a non-invasive stage. Multiple studies show that detection of melanoma rates have increased with the use of Total body photography (Annkathrin Hornung et al., Int J Environ Res Public Health. 2021).
- Improved Monitoring: By capturing and storing images after each procedure, Total Body Photography (TBP) helps to notice the changes in suspicious lesions and supports ongoing monitoring (Annkathrin Hornung et al., Int J Environ Res Public Health. 2021).
- Minimization of unneeded procedures: TBP helps avoid unnecessary procedures by reducing the number of biopsies and removals of benign (non-cancerous) lesions, saving costs and minimizing patient stress. (Melanoma Institute Australia, 2022)
- Comfortable Examinations: TBP is a quick and non-invasive procedure that mainly causes no disruption to patients physical and mental well-being. (On point skin cancer clinic)
- High Accuracy: Automated total body mapping systems detect over 90% of clinically relevant melanocytic lesions identified by expert dermatologists, including all new or changed lesions during follow-up (Julia K Winkler et al., Elsevier, 2024).
- Efficiency and time-saving: These systems can complete a full baseline examination in about 14 minutes, significantly faster than traditional manual methods, reducing clinician workload while maintaining thorough skin coverage (Julia K Winkler et al., Elsevier, 2024).
What Role Can Total Body Photography Play in Rural Areas?
3D Total Body Photography (TBP) has the potential to significantly improve access to dermatology services in remote and rural regions, where melanoma rates are high but access to care is limited. This is particularly relevant in countries like Australia, where many high-risk individuals live in underserved communities with minimal access to dermatologic care (Li et al., Frontiers in Medicine, 2018).
By enabling trained local healthcare providers like nurses or general practitioners to capture standardized skin images, these photographs can be transmitted securely to remote dermatologists for evaluation via teledermatology. This model helps lighten the shortage of dermatology specialists in rural settings, offering patients expert review without the need for long-distance travel (Coustasse et al., Telemedicine and e-Health, 2019). In this way, TBP effectively bridges the access gap created by geographic isolation.
While challenges such as equipment costs, digital infrastructure, and data privacy concerns remain, successful integration of TBP into rural healthcare systems could greatly enhance early skin cancer detection and monitoring, making specialist-level care more equitable and accessible (The University of Queensland, 2024).
What are the Limitations of TBP?
Total Body Photography (TBP) with AI integration brings important benefits, but it also comes with several limitations that can make widespread use challenging. Cost is one of the main concerns—especially for cancer centers with limited budgets. High-end TBP systems, particularly those with 3D imaging, are expensive, take up a lot of space, and require strong IT infrastructure to store and manage the large image files they produce (Li et al., Frontiers in Medicine, 2018). There are also privacy and data security concerns, since TBP involves taking full-body images, often while patients are wearing minimal clothing. This raises questions about patient consent, secure storage, and the sensitivity of medical image data (Primiero et al., Frontiers in Medicine, 2024).
Another limitation is that some areas of the body—like the scalp, genital regions, palms, soles, skin folds, and other hard-to-photograph spots—are difficult to capture accurately. As a result, melanomas in those locations may be missed (Melanoma Institute Australia, 2022). TBP can also struggle with detecting hypopigmented melanomas, which account for around 2–8% of cases. These lighter or non-pigmented lesions may not be picked up as easily by the imaging systems as darker ones (Li et al., Frontiers in Medicine, 2018). In younger patients, another issue is the higher rate of unnecessary biopsies, since normal mole growth might be mistaken for a malignancy (Melanoma Institute Australia, 2022).
Finally, TBP usually requires regular follow-up—annually or biannually for most people, and every 3 to 6 months for those at high risk. These ongoing appointments demand time and resources, both from patients and clinics, and are often missed due to busy schedules or practical barriers (The Woods Medical Center, 2025).
What’s Next in AI and Skin Surveillance?
Future developments in skin surveillance are likely to focus on making artificial intelligence more transparent and easier to understand. By combining genetic data and medical history researchers hope to build smarter, more personalized tools for skin monitoring. New technologies, such as smartphone-compatible total body photography (TBP) and teledermatology platforms, could also play crucial roles for people in remote or underserved areas to access care. At the same time, methods like federated learning, which allow algorithms to learn from data without moving it from secure locations, may help protect patient privacy while still improving the accuracy of these systems.
Photo: Depositphotos
Smartphone-Compatible Total Body Photography (TBP)
A growing number of mobile applications are now being developed to aid in the early detection of skin cancer. One such example is SkinVision, a CE-marked medical device in Europe that utilizes machine learning to assess images of skin lesions and categorize risk levels (low, low with tracking, or high). The app allows users to monitor changes over time and currently supports more than 2 million users globally. Recent studies report that SkinVision detects approximately 95% of skin cancer cases (SkinVision – Skin cancer detection app., 2025).
Similarly, tools such as SkinScreener, MoleMapper, and SkinIO offer comparable features. SkinIO, for example, employs total body photography to capture comprehensive skin imagery, which is then reviewed remotely by board-certified dermatologists who notify users if follow-up is recommended.
While these applications can empower users and support early detection, it is essential to note that neither of them are FDA-approved yet and should not be considered a replacement for clinical dermatological evaluation.
The Future Vision of Skin Cancer Monitoring
Ultimately, the future of skin cancer monitoring will need to be centered around patients’ needs and experiences. This means designing technologies that incorporate user feedback, provide clear instructions, and are accessible across different socioeconomic and geographic backgrounds. Tools that combine skin imaging with individual medical history—such as family history of melanoma or known genetic mutations—could help doctors offer more personalized risk assessments and follow-up plans (Nahm et al., Int J Dermatol, 2025).
For these technologies to be safely integrated into medical care, they must go through rigorous evaluation, not only in controlled trials but also in real-world settings. Regulatory agencies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) are starting to adopt structured frameworks that support the safe rollout and long-term monitoring of AI-powered tools in healthcare. For instance, models such as the AI-Medical Device Risk Stratification Framework have been proposed to categorize the risk level of different digital tools and guide regulatory oversight (FDA, EMA regulatory guidelines, 2024-2025).
Yet, fairness remains a major concern. Many current skin image datasets include mostly lighter skin tones, which can lead to reduced diagnostic accuracy for people with darker skin. This imbalance could widen existing health disparities if not addressed (Courtney M. Heldreth et al., ACM Journal on Responsible Computing, 2024). Global efforts—like the Skin Image Database for Equity (SIDE) and the Global Skin Image Dataset Project—are now working to build more diverse and representative datasets to ensure that new technologies serve all populations effectively (Ghorbani et al., MICCAI, 2024).
Importantly, these tools are not meant to replace medical professionals. Instead, they are designed to support clinicians by handling routine tasks like identifying changes in moles or organizing follow-up recommendations. This way, dermatologists can focus their time and attention on complex cases, decision-making, and connecting with their patients. If designed and implemented thoughtfully, these technologies could improve both the efficiency of skin cancer screening and the quality of care delivered to patients (Nahm et al., Int J Dermatol, 2025).
You Can Also Read Melanoma (Skin Cancer): Symptoms, Causes, Stages, Diagnosis and Treatment by OncoDaily
You Can Also Listen 50¢ Soap, Skin Cancer, and TIME’s Kid of the Year – Myths & Facts: OncoDaily DeepDive
Renaissance Portraits as Early Dermatological Records
Renaissance portraits serve as some of the earliest accidental lesion maps, capturing visual records of skin conditions centuries before modern dermatological tools like dermoscopy and total body photography existed. Artists of that era painted detailed human subjects, inadvertently documenting various skin lesions and conditions that today’s dermatologists can interpret through a clinical lens (Amit Om et al., J Clin Aesthet Dermatol. 2018).
For example, Renaissance art often depicted infectious skin diseases such as erysipelas (“St. Anthony’s fire”) and smallpox, with visible plaques or lesions shown on subjects’ skin. Artists also unintentionally captured neoplastic (tumor) conditions like benign nevi (moles), malignant growths, and pigmentary changes. Here are few examples:
Charles IV of Spain and His Family” by Francisco Goya
In this royal group portrait, Goya depicts the King’s sister, Infanta María Josefa (fourth from the left), with a dark pigmented mark on her forehead that appears suspicious. While many artists of the era might have concealed such an imperfection, Goya’s commitment to realism meant capturing every detail. In doing so, he inadvertently created one of the most lifelike examples of an accidental “lesion map” in art. Though it’s impossible to confirm whether the mark was melanoma or another skin condition, historical records note that she died in 1801, only six months after the painting was completed.
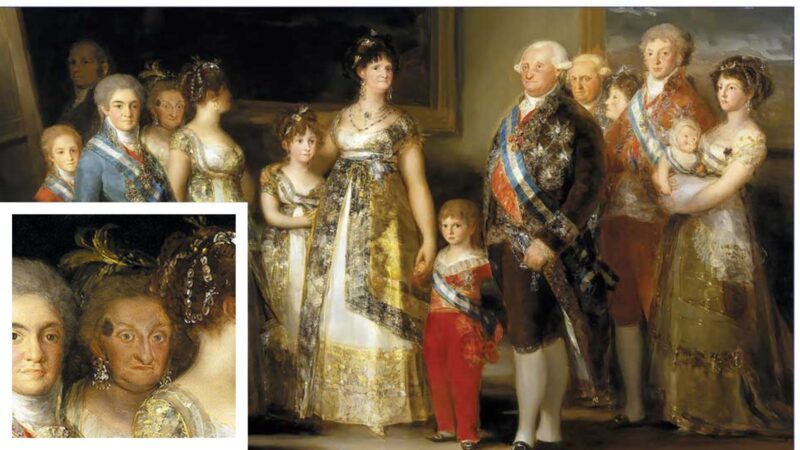
Picture from FranciscoGoya.com
The Temptation of St. Anthony” by Matthias Grünewald
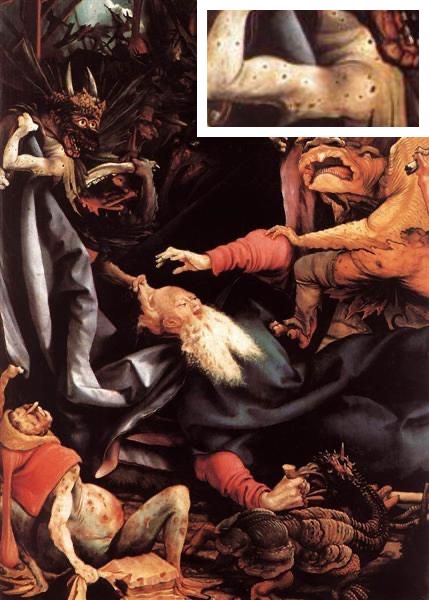
This painting is a part of the Isenheim Altarpiece (1512–1516), is recognized for its accurate and complete depiction of a halo naevus (also known as a halo nevus or Sutton nevus). This lesion consists of a pigmented mole surrounded by an area of depigmentation, creating a “halo” effect around the nevus. Grünewald’s representation is considered one of the earliest and most precise visual records of this dermatological phenomenon in art history.
(Happle, R. Grünewald-Nävus. Hautarzt 45, 882–883, 1994)
Duke and Duchess of Urbino” by Francesca P.
In the portrait, the Duke is captured with benign intradermal nevi (moles).
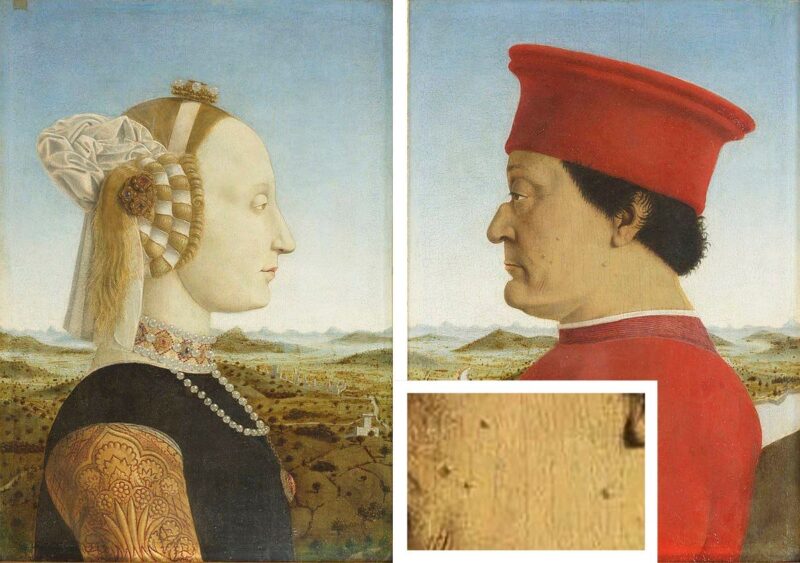
All examples from (Amit Om et al., J Clin Aesthet Dermatol. 2018).
Written by Ina Khachatryan
FAQ
What is Total Body Photography and how does it work?
TBP is a non-invasive method that captures high-resolution images of the entire skin surface to monitor moles and lesions over time for early skin cancer detection.
Who should get Total Body Photography?
TBP is recommended for people at high risk of melanoma, such as those with many moles, atypical lesions, or a family history of skin cancer.
How often should Total Body Photography be done?
TBP is typically repeated every 6 to 12 months, with higher-risk patients sometimes needing follow-up every 3 to 6 months.
How does Total Body Photography help in early detection of skin cancer?
By providing a visual baseline, TBP enables clinicians to detect new or changing lesions early, improving melanoma survival rates.
What is the difference between Total Body Photography and dermoscopy?
TBP captures full-body images for broad monitoring, while dermoscopy magnifies individual lesions for detailed examination.
What is Automated Lesion Mapping and how is it used?
Automated Lesion Mapping uses AI software to identify and track skin lesions on TBP images, supporting efficient lesion monitoring over time.
How accurate is Automated Lesion Mapping compared to manual mapping?
Automated Lesion Mapping is highly accurate, detecting over 90% of relevant lesions with less variability than manual methods.
What technologies or algorithms power Automated Lesion Mapping?
ALM relies on deep learning algorithms, especially convolutional neural networks, trained to analyze lesion features in skin images.
Can Automated Lesion Mapping detect all types of skin lesions?
While effective for many pigmented lesions, ALM may have limitations in detecting hypopigmented or hard-to-image lesions.
How is Automated Lesion Mapping integrated with other imaging methods like Total Body Photography?
ALM analyzes the comprehensive images captured by TBP to create detailed lesion maps for improved skin surveillance.
How accurate is artificial intelligence in diagnosing skin cancer compared to doctors?
AI can diagnose skin cancer with accuracy comparable to or sometimes better than dermatologists, improving sensitivity and specificity.
Can AI improve early detection and diagnosis of melanoma and other skin cancers?
Yes, AI enhances early detection by analyzing skin images efficiently and supporting clinicians in identifying suspicious lesions sooner.
What challenges does AI face in becoming a reliable tool for skin cancer diagnosis?
AI still faces challenges like biased training data that may miss diverse skin tones, limited transparency in how decisions are made, inconsistent accuracy across different populations, and practical difficulties integrating into everyday clinical workflows.
Is self-diagnosing skin cancer realistic or reliable?
While smartphone apps and online resources can raise awareness, self-diagnosing skin cancer is not reliable and should never replace professional evaluation, as even trained dermatologists use advanced tools like dermoscopy, TBP, and AI to detect subtle or dangerous lesions.