PEACE-1+ STAMPEDE IPD Meta-analysis at ESMO 2025 — Prostate RT Extends PFS; OS Signal Confined to Low-Volume Disease. Presented by Peter J. Godolphin during the Mini Oral session on GU tumours (prostate, penile and testis).
Background
Guidelines shaped by PEACE-1 and STAMPEDE favor, for low-volume, synchronous mHSPC, a combination of prostate radiotherapy (RT) plus an androgen receptor pathway inhibitor (ARPI) and androgen-deprivation therapy (ADT); docetaxel, with or without an ARPI, is generally not recommended. To clarify the direct effect of prostate RT, investigators assembled updated individual patient data (IPD) from eligible randomized trials.
Methods
Prospero registration CRD420251038299. Primary outcomes were overall survival (OS), progression-free survival (PFS; clinical/radiologic progression or death), and symptomatic local events (SLE: TURP, catheterization, ureteric stent, or nephrostomy). A two-stage, common-effect meta-analysis estimated RT effects.
- Main effects were based on OS.
- Interactions were assessed on PFS (for power) and then on OS if signals emerged.
- Absolute effects derived from flexible parametric models.
All analyses adjusted for a core covariate set.
Results
- IPD from PEACE-1 and STAMPEDE were included to date, representing 88% of eligible men.
- Overall effect: Prostate RT did not improve OS (HR 0.93, 95% CI 0.85–1.02; p=0.11) but prolonged PFS (HR 0.88, 95% CI 0.81–0.96; p=0.003).
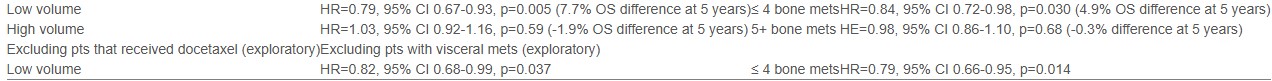
- Effect modification: RT effects varied by disease volume on PFS and OS (Interaction p=0.002 and p=0.009, respectively) and by number of bone metastases on PFS (Interaction p=0.009), less so on OS (p=0.14).
- Who benefited: Benefits were confined to low-volume disease, irrespective of docetaxel use, and to men with ≤4 bone metastases, especially when visceral metastases were absent.
- RT effects did not clearly vary by other patient characteristics.
- Investigators will present updated results—including HORRAD IPD and the SLE endpoint—to refine recommendations.
Conclusions
Across all synchronous mHSPC, no overall OS benefit was seen with prostate RT, although PFS improved. In low-volume disease, there was an approximately 21% relative reduction in risk of death, supporting prostate RT as a component of multimodality treatment for this subgroup and reinforcing current practice patterns emphasizing volume-directed selection. Further updates with HORRAD and SLE outcomes will help calibrate absolute benefits and guide routine care.
You can read the full abstract here.