Pancreatic ductal adenocarcinoma (PDAC) remains one of the most lethal malignancies worldwide, with a persistently poor prognosis in the metastatic setting. Despite advances in systemic chemotherapy, five-year survival for metastatic disease remains below 5%. Liver metastases account for the vast majority of dissemination patterns, while lung-only metastases represent a less common but increasingly recognized subgroup.
Several retrospective series have suggested that patients with isolated pulmonary metastases may experience more favorable outcomes compared with those harboring liver, peritoneal, or multi-organ disease. However, the clinical and biological determinants underlying this apparent prognostic advantage remain incompletely understood. In particular, the molecular characteristics of lung-only metastatic PDAC and the contribution of circulating tumor DNA (ctDNA) detection have not been comprehensively explored.
This retrospective single-center study, published in European Journal of Cancer on February, 2026, aimed to compare clinical features, molecular profiles, treatment outcomes, and survival of PDAC patients according to metastatic site, with a specific focus on patients presenting with lung-only metastases.
Title: Lung-only metastatic pancreatic cancer: Differences in patients ‘characteristics, molecular profile and survival
Authors: Alice Boilève, Léa Mercier, Baptiste Bonnet, Anthony Tarabay, Sarah Blanchet-Deverly, Antoine Hollebecque, Cristina Smolenschi, Marine Valéry, Matthieu Delaye, Thomas Pudlarz, Alina Fuerea, Valérie Boige, Jérome Durand-Labrunie, Maximiliano Gelli, Paul Beunon, Rémy Barbe, Aurélien Lambert, Michel Ducreux
Methods
This retrospective analysis included all patients diagnosed with metastatic PDAC between 2010 and 2024 at a single French academic center. Clinical, radiological, biological, and molecular data were collected from medical records and entered into a secure REDCap® database. The study was approved by the local ethics committee (IRB n° 2024–415) and conducted in accordance with the Declaration of Helsinki.
Patients were categorized according to metastatic pattern at the time of metastatic diagnosis:
- Lung-only metastases
- Liver-only metastases
- Peritoneal-only metastases
- Other or multiple metastatic sites
Metastatic sites were validated during multidisciplinary tumor board discussions with expert radiologists.
Molecular Profiling
Molecular analyses were performed in a subset of patients using tumor tissue, circulating cell-free DNA, or both, primarily within the MOSCATO, MATCH-R, and STING clinical trials. Alterations in key genes (including KRAS, TP53, SMAD4, CDKN2A) were recorded, along with microsatellite status and tumor mutational burden (TMB) when available.
Treatments and Outcomes
All patients received standard-of-care systemic chemotherapy for metastatic PDAC. Overall survival (OS) was defined from metastatic diagnosis to death from any cause. Progression-free survival (PFS) was defined from initiation of first-line chemotherapy to radiologic progression or death. Local treatments with curative intent (surgery, radiotherapy, ablation techniques) were analyzed specifically in the lung-only subgroup.
Statistical Analysis
Survival analyses were performed using Kaplan–Meier estimates, with comparisons by log-rank test. Multivariate analyses were conducted using Cox proportional hazards models adjusting for known prognostic factors. Statistical analyses were performed using RStudio 2022.12.0.
Results
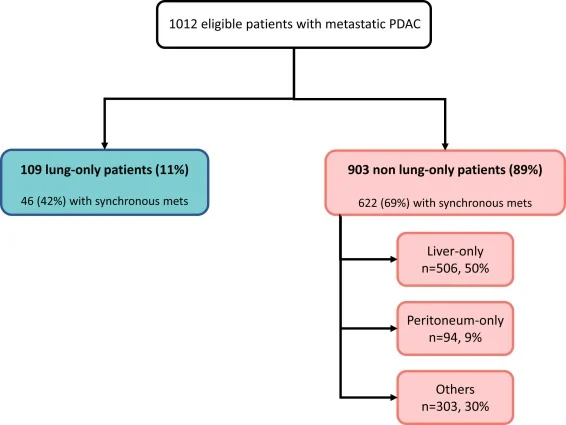
Among 1,012 metastatic PDAC patients, 109 (11%) presented with lung-only metastases, 506 (50%) with liver-only metastases, 94 (9%) with peritoneal-only metastases, and 303 (30%) with other or multiple sites.
Compared with other metastatic patterns, lung-only patients were:
- More frequently female (63% vs 46%)
- Older at metastatic diagnosis (median 66.2 vs 63.0 years)
- Less likely to present with synchronous metastases (42% vs 69%)
- More often non-smokers
- More likely to have a primary tumor located in the pancreatic head
CA19-9 levels at diagnosis were significantly lower in lung-only patients, while CEA levels were comparable between groups.
A contributive molecular profile was available for 457 patients (45%). KRAS and TP53 mutations were less frequently detected in lung-only patients when assessed by liquid biopsy. However, when analyses were restricted to tumor tissue, no significant differences were observed between lung-only and other metastatic groups, suggesting lower ctDNA shedding rather than true molecular divergence.
Median tumor mutational burden was lower in lung-only patients, and SMAD4 alterations were significantly less frequent in this subgroup.
You can also read about Top 10 Pancreatic Cancer Updates – January 2026 on OncoDaily.
First-Line Treatment and Response
First-line chemotherapy regimens did not differ significantly between groups. Overall response rates were similar, but disease control rate was higher in lung-only patients (84% vs 72%). Lung-only patients experienced fewer hospitalizations during first-line therapy.
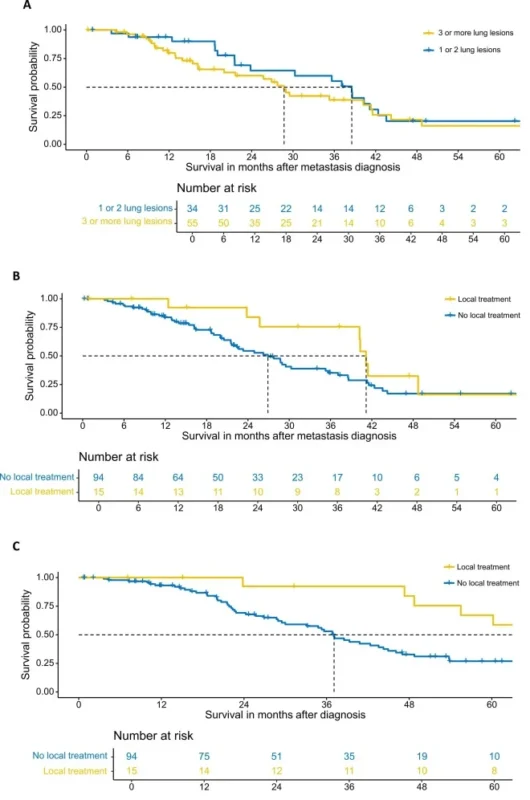
Median OS from metastatic diagnosis was significantly longer in the lung-only group:
- 28.7 months for lung-only metastases
- 13.5 months for liver-only metastases
- 11.5 months for peritoneal-only metastases
- 11.3 months for other or multiple sites
Median PFS was also prolonged in lung-only patients (10.6 vs 6.1 months). In multivariate analysis, lung-only metastatic status remained an independent favorable prognostic factor (HR = 0.40).
Locoregional Treatments
Fourteen percent of lung-only patients underwent at least one curative-intent local treatment. Median OS from metastatic diagnosis was numerically longer in patients receiving locoregional therapy, and OS from initial diagnosis was significantly prolonged.
Conclusion
This large single-center retrospective study demonstrates that PDAC patients with lung-only metastases represent a distinct subgroup with markedly improved survival compared with other metastatic patterns. These patients display specific clinical characteristics, lower ctDNA detectability, and prolonged OS and PFS, independent of other prognostic factors.
Liquid biopsy appears less contributive in lung-only metastatic PDAC, underscoring the importance of tumor tissue analysis when feasible. While locoregional treatments may further improve outcomes in selected patients, the favorable prognosis of this subgroup is not solely explained by local interventions.
Overall, these findings support the concept that lung-only metastatic PDAC constitutes a biologically and clinically distinct entity that should be considered separately in both clinical practice and future research.
The full article is available in the European Journal of Cancer.