At the ESMO Congress 2025 in Berlin, Dr. Jean-Baptiste Bachet (Paris, France) presented the final results of the phase II OPTIPRIME trial (Abstract 727MO), a multicentre French study evaluating a novel “stop-and-go” strategy combining FOLFOX and panitumumab (Pmab) in patients with RAS/BRAF wild-type metastatic colorectal cancer (mCRC).
At OncoDaily GI, we spotlight the innovations reshaping colorectal cancer care — from adaptive treatment sequencing to intelligent use of targeted therapies to mitigate resistance and cumulative toxicity.
Background
Epidermal growth factor receptor (EGFR) blockade has long been a cornerstone of therapy in RAS/BRAF wild-type mCRC, delivering significant response rates and survival benefits. Yet, the cumulative toxicities associated with prolonged anti-EGFR exposure — particularly dermatologic and nail toxicities — often limit treatment duration. Furthermore, continuous EGFR inhibition can foster resistant subclones, potentially diminishing long-term efficacy.
The OPTIPRIME trial was designed to test whether an intermittent (“stop-and-go”) use of panitumumab, alongside oxaliplatin-based chemotherapy, could maintain efficacy while improving tolerability and extending the duration of disease control (DDC) — a metric capturing both the initial and subsequent treatment phases under EGFR-targeted therapy.
Study Design and Methods
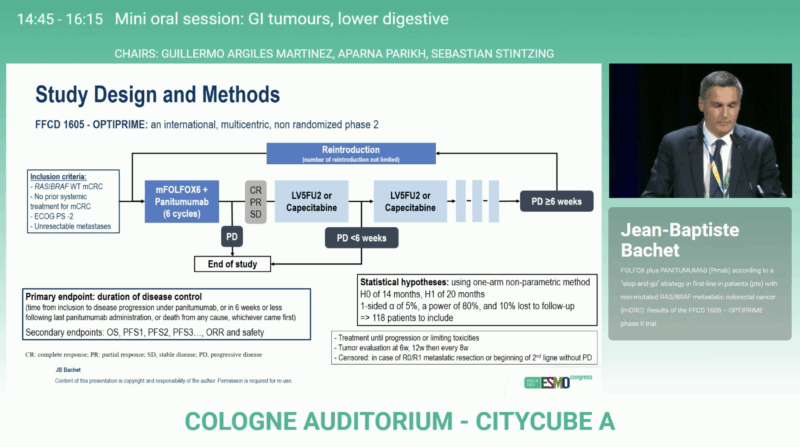
Conducted across 36 French centers between April 2018 and May 2023, OPTIPRIME enrolled 118 patients (mITT: 115 after excluding 3 with RAS or BRAF mutations). Eligible patients had previously untreated, measurable, RAS/BRAF wild-type mCRC with ECOG performance status 0–1.
Treatment consisted of
- Induction phase: 6 cycles of FOLFOX plus panitumumab
- Maintenance phase: Fluoropyrimidine monotherapy (LV5FU2 or capecitabine) for patients achieving disease control
- Reintroduction phase: Upon progression, reintroduction of panitumumab ± oxaliplatin for 6 cycles, repeated as needed (“stop-and-go”)
The primary endpoint, DDC, was defined as the time from inclusion to radiological progression under EGFR therapy with chemotherapy or death. Patients undergoing R0/R1 metastasectomy were censored at surgery, and those switching therapy without progression were censored at the time of switch.
The study was powered to detect an improvement from a median DDC of 14 months (H0) to 20 months (H1), with a 1-sided α of 5% and 80% power. The predefined threshold for success (upper critical value) was 17.84 months.
Results
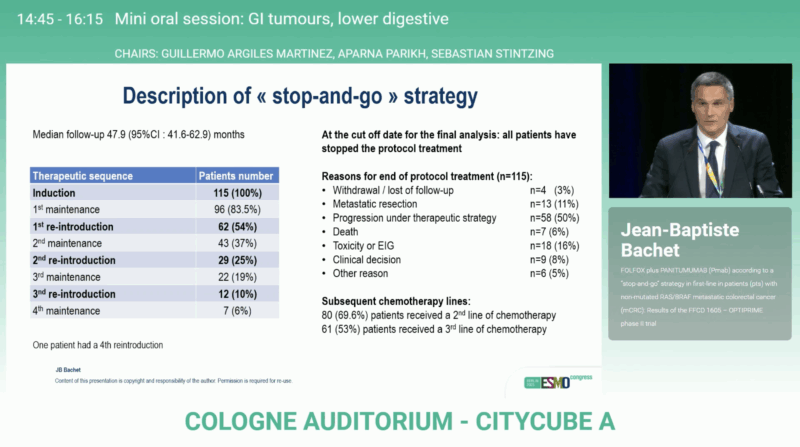
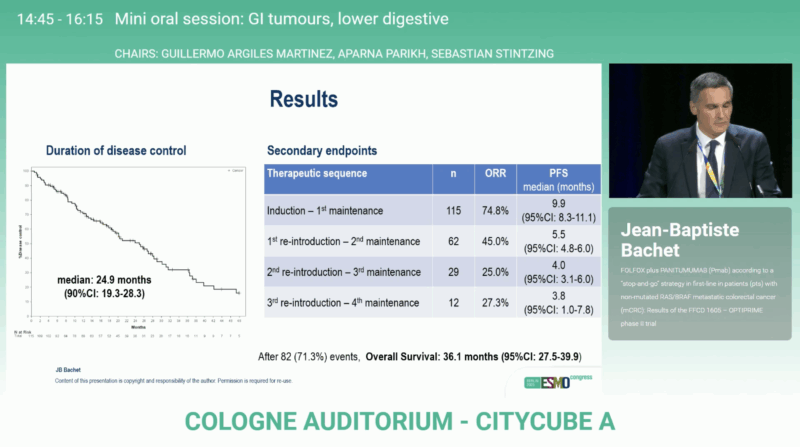
After a median follow-up of 47.9 months, OPTIPRIME achieved its primary endpoint with a median DDC of 24.9 months (90 % CI 19.3–28.3), surpassing the predefined efficacy boundary. The overall response rate reached 74.8 %, reflecting substantial activity of the FOLFOX + panitumumab regimen.
Most patients (83.5 %) entered at least one maintenance phase, and many underwent repeated reintroductions of panitumumab, illustrating the practical feasibility of this cyclic regimen. A subset (11 %) proceeded to metastasectomy with curative intent. At data cut-off, 69.6 % of patients had received subsequent second-line therapy.
The median overall survival was 36.1 months (95 % CI 27.5–39.9), among the best reported for first-line mCRC in this molecular subgroup. Median progression-free survival (PFS) during the induction and first maintenance phase was 9.9 months (95% CI 8.3–11.1), confirming durable early disease control. These findings confirm that intermittent EGFR inhibition can sustain long-term disease control while preserving patient quality of life and delaying resistance.
Interpretation
The OPTIPRIME trial successfully met its primary endpoint, validating a biologically rational and clinically practical strategy for optimizing EGFR-targeted therapy in mCRC. The median DDC of nearly 25 months underscores the durability achievable through treatment holidays, allowing patients to recover from toxicity while preserving future sensitivity to anti-EGFR agents.
This “stop-and-go” model represents an important step forward in adaptive treatment design, addressing one of the key dilemmas in metastatic colorectal cancer: how to balance intensity, tolerance, and long-term benefit. It aligns with growing evidence from molecular studies showing that resistant EGFR clones can decay during drug-free intervals, restoring sensitivity upon rechallenge.
Clinical Implications
The OPTIPRIME findings strengthen the case for flexible, individualized sequencing of anti-EGFR therapy in mCRC. By alternating active and maintenance phases, clinicians can maintain high disease control rates while minimizing cumulative toxicity and optimizing quality of life.
With median survival exceeding three years, the study underscores how thoughtful integration of targeted agents within an adaptive framework can meaningfully extend outcomes in metastatic colorectal cancer.
You can read the full abstract here.
Conclusion
The OPTIPRIME phase II trial (NCT03584711) validates the clinical value of a “stop-and-go” panitumumab strategy in RAS/BRAF wild-type mCRC. By integrating periods of EGFR inhibition and maintenance fluoropyrimidine therapy, investigators achieved both prolonged disease control and strong overall survival, with improved tolerability.
These results may inform future treatment paradigms emphasizing adaptive, toxicity-conscious sequencing of targeted agents — a principle likely to gain further traction as precision oncology continues to evolve.

You can read about PERISCOPE II Trial: Randomized study finds no OS advantage for gastrectomy plus CRS/HIPEC versus systemic therapy on OncoDaily.