At the SIO 2025 Annual Meeting, Dr. Joke Bradt presented new data positioning music therapy as an effective and scalable treatment for anxiety in cancer survivorship. Rather than functioning only as a supportive wellness activity, music therapy demonstrated therapeutic outcomes comparable to those seen with structured psychological care.
The work presented suggests that music therapy can stand alongside cognitive behavioral therapy not as an alternative or complementary practice, but as a peer treatment option – one that may be particularly relevant for patients who do not connect with traditional talk-based therapies, or who benefit from expressive and sensory forms of emotional processing.
Background
Music therapy in oncology spans a continuum – from informal patient-driven music listening to structured, therapist-guided interventions involving active engagement such as guided relaxation, vocalization, and collaborative songwriting. Over the past decade, clinical trials and meta-analyses have shown that music therapy can reduce anxiety, depression, pain, and improve quality of life.
However, many music therapy studies are rated as “low methodological quality” due to the inability to blind patients to treatment, a standard derived from drug trial design. This often leads to weaker recommendation levels and limited reimbursement, despite meaningful clinical benefits. Dr. Bradt described this as the “methodological quality trap”, calling for evaluation frameworks that are appropriate for non-pharmacological therapies.
A crucial next step is comparing music therapy directly with gold-standard psychological care, rather than placebo or waitlist controls – leading to the MELODY Trial.
The MELODY Trial
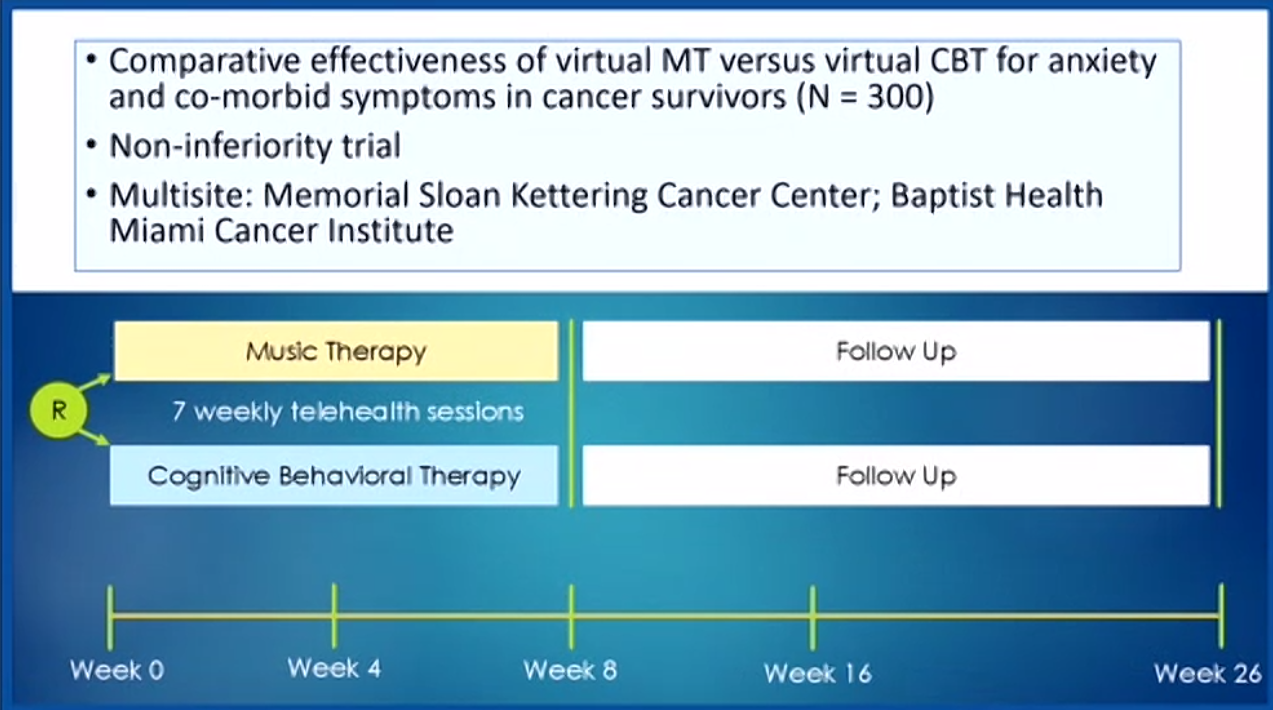
The MELODY Trial was a multi-site, telehealth-based randomized non-inferiority study comparing music therapy to cognitive behavioral therapy (CBT) for anxiety in cancer survivors. The study enrolled 300 participants across Memorial Sloan Kettering Cancer Center and Baptist Health Miami Cancer Institute, each receiving seven weekly virtual sessions of either music therapy or CBT, with follow-up through week 26.
The music therapy protocol began with guided music listening and relaxation to establish trust, followed by collaborative songwriting, in which patients worked with the therapist to shape lyrics and melodies that reflected their personal experiences. This creative process aimed to support emotional expression and long-term anxiety reduction.
The CBT sessions, by contrast, focused on psychoeducation, cognitive restructuring, relaxation strategies, and managing worry patterns, following a conventional anxiety treatment framework. Both interventions included at-home practice between sessions.
Results
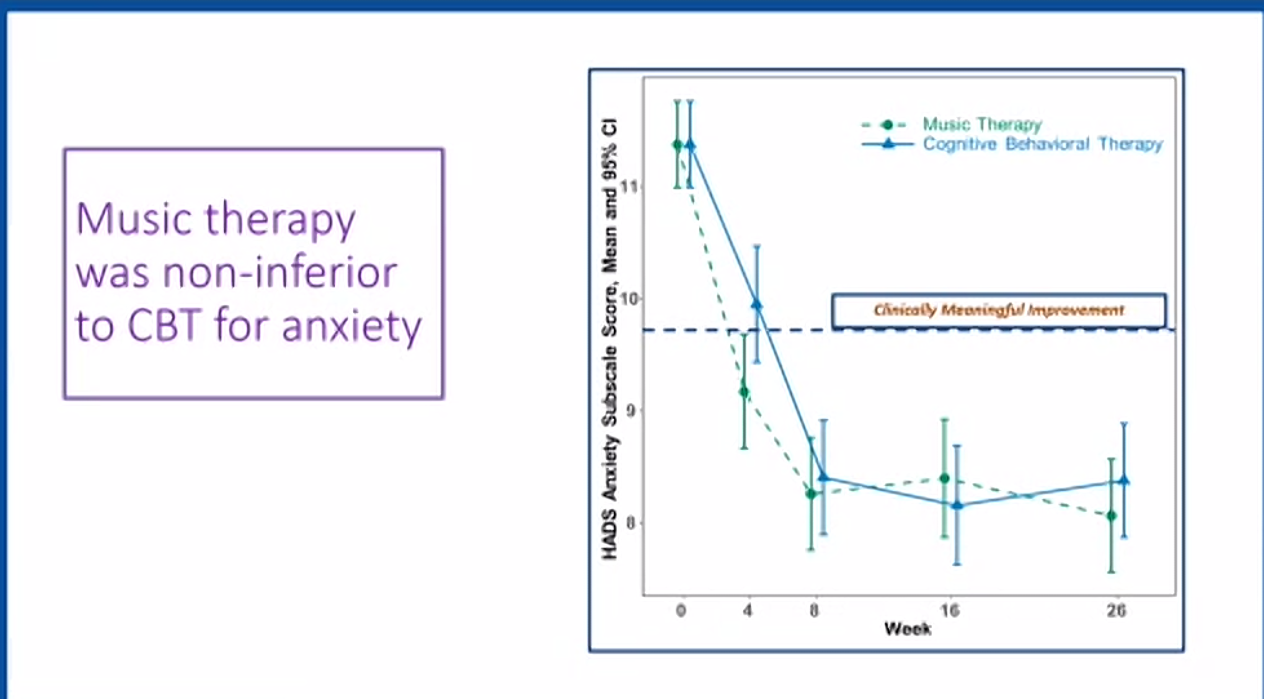
The trial demonstrated that music therapy was non-inferior to CBT for reducing anxiety, meaning both treatments resulted in clinically meaningful, sustained improvements. Anxiety symptoms decreased significantly in both groups, with benefits maintained up to four months post-treatment.
Secondary outcomes – including fatigue, depressive symptoms, insomnia, pain, cognitive complaints, and both mental and physical quality of life – showed similar improvements in both arms.
Qualitative analysis of patient-written songs highlighted emotional processing, meaning-making, and self-reconnection as central themes. Many participants described the final song as a tangible representation of their psychological progress.
Conclusion
The MELODY Trial provides strong evidence that music therapy is an effective treatment option for anxiety in cancer survivorship, with outcomes comparable to those achieved through cognitive behavioral therapy. The fact that this benefit was observed in a rigorously designed, multi-site comparative trial adds weight to the role of music therapy as a clinically grounded intervention rather than a supplemental or ancillary service.
Importantly, the entire intervention was delivered remotely using standardized protocols, demonstrating that music therapy can be offered at scale without requiring in-person clinical infrastructure. This makes the model particularly well-suited for patients who face barriers to traditional care, including those with limited mobility, those living far from cancer centers, and survivors navigating return to daily life following treatment.
These findings support the integration of music therapy as a core component of survivorship care, not an optional add-on. As evidence continues to expand, the data also point to the need for reimbursement frameworks that recognize music therapy as a clinically effective treatment, ensuring patients have sustainable access to services that improve psychological well-being and quality of life. The trial’s results represent a meaningful shift in how supportive care in oncology can be delivered – more flexible, more expressive, and more patient-centered, without compromising clinical rigor.
For more information clik here.