What is immunotherapy?
Immunotherapy is a type of cancer treatment that helps your own immune system find and fight cancer cells. Normally, your immune system works to protect you from infections and diseases, but cancer cells can sometimes hide from it or weaken its response. Immunotherapy boosts the immune system, making it stronger and better at attacking cancer.
Unlike chemotherapy, which directly kills cancer cells, immunotherapy trains your body to do the work itself. This can lead to a longer-lasting defense against cancer, sometimes even after treatment stops.
How Immunotherapy Works to Fight Cancer
Your immune system is designed to find and destroy harmful invaders like viruses, bacteria, and abnormal cells, including cancer. However, cancer cells can be tricky—they sometimes hide from the immune system or send signals that weaken the body’s natural defenses. Immunotherapy helps the immune system recognize and attack cancer more effectively.
Here’s how it works:
- Boosting the Immune Response – Some immunotherapies strengthen immune cells so they can better detect and destroy cancer cells.
- Removing “Brakes” on the Immune System – Normally, the immune system has built-in brakes to prevent attacking healthy cells. Some cancers take advantage of these brakes to avoid being attacked. Immunotherapy can release these brakes, allowing immune cells to go after cancer.
- Training the Immune System – Certain immunotherapies act like teachers for the immune system, helping it recognize cancer cells more easily and remember them in case they return.
Because immunotherapy helps the body fight cancer itself, it can sometimes provide long-lasting benefits. However, it doesn’t work for everyone, and doctors carefully check whether a patient’s cancer is likely to respond to this type of treatment.
Types of Immunotherapy
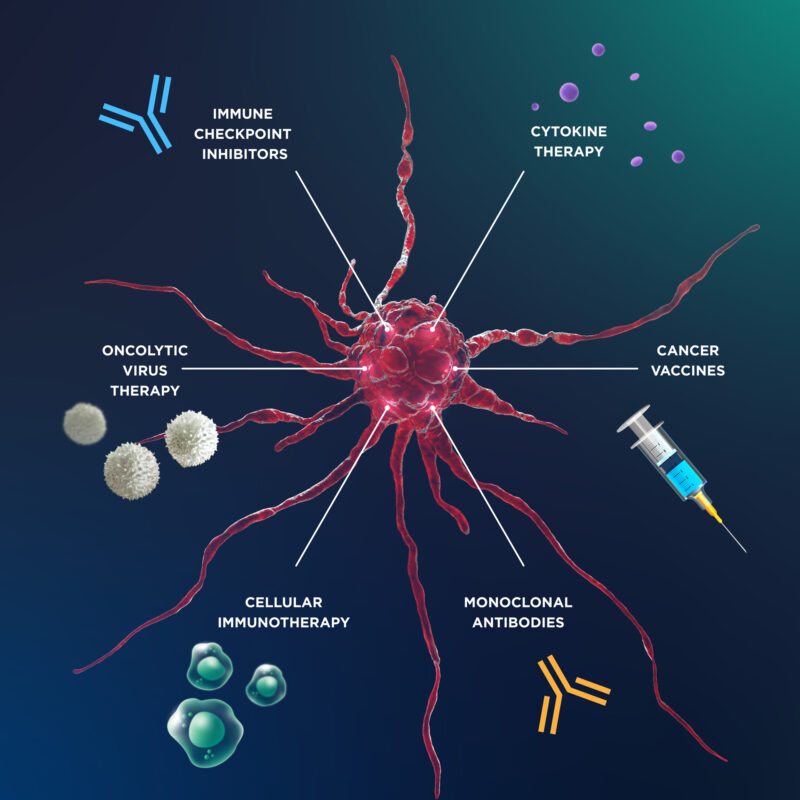
Immunotherapy comes in different forms, each working in a unique way to help your immune system fight cancer. Here are the main types:
- Checkpoint Inhibitors – Some cancers hide from the immune system by using special proteins called “checkpoints.” Checkpoint inhibitors remove these barriers, allowing immune cells to recognize and attack cancer.
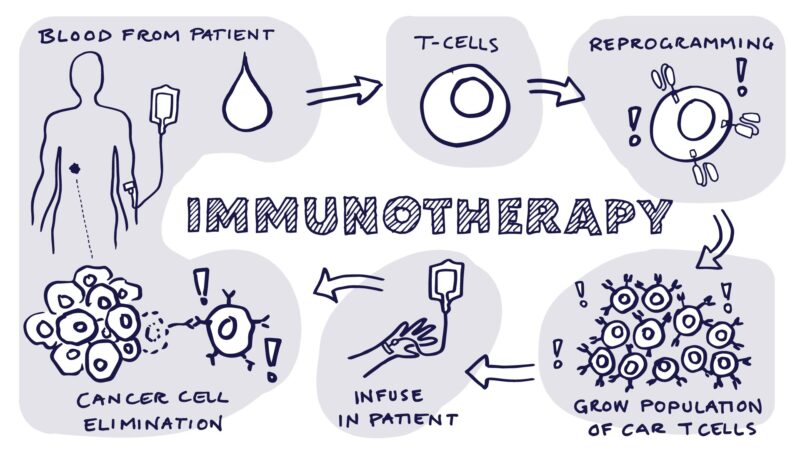
- CAR T-Cell Therapy – This treatment modifies a patient’s own immune cells (T-cells) in a lab to make them better at finding and killing cancer. The modified cells are then put back into the patient’s body to target cancer directly.
- Cancer Vaccines – Unlike regular vaccines that prevent infections, cancer vaccines help train the immune system to recognize and fight cancer cells already in the body.
- Monoclonal Antibodies – These are lab-made immune proteins designed to attach to specific cancer cells, marking them for destruction by the immune system. Some also carry drugs or radiation directly to tumors.
- Oncolytic Virus Therapy – This approach uses modified viruses that infect and kill cancer cells without harming normal cells. It also helps alert the immune system to attack the tumor.
Each type of immunotherapy works differently, and doctors choose the best option based on the type of cancer and how a patient’s immune system responds.
Who Is Eligible for Immunotherapy?
Not everyone with cancer is eligible for immunotherapy. Doctors carefully assess whether a patient’s cancer is likely to respond to this treatment by looking at specific factors, including biomarkers, cancer type, and overall health.
One of the most important factors is biomarker testing. Some cancers have proteins like PD-L1 or genetic changes such as high microsatellite instability (MSI-H) or tumor mutation burden (TMB-H) that make them more likely to respond to immunotherapy, especially checkpoint inhibitors like Keytruda (pembrolizumab) or Opdivo (nivolumab). The type and stage of cancer also matter. Immunotherapy is commonly used for advanced or metastatic cancers, including lung cancer, melanoma, bladder cancer, and some forms of cervical and breast cancer. However, it is still being studied for many other types.
Doctors also evaluate a patient’s overall health. Since immunotherapy works by activating the immune system, patients with autoimmune diseases (such as lupus or rheumatoid arthritis) or organ transplants may not be good candidates, as the treatment could cause the immune system to attack healthy tissues. For some patients who don’t meet standard criteria, clinical trials offer another option, providing access to experimental immunotherapy treatments. As research progresses, scientists are working to expand immunotherapy’s benefits to more types of cancer and patients.
Signs immunotherapy is working
When starting immunotherapy, many patients wonder how they’ll know if the treatment is working. Unlike chemotherapy, which often shows quick tumor shrinkage, immunotherapy works differently—it helps the immune system attack cancer over time, so results can take longer to appear.
One of the first signs that immunotherapy is working is stable disease or tumor shrinkage on imaging scans, such as CT or MRI. While some tumors begin to shrink within a few months, others may stay the same size for a while before shrinking. In some cases, tumors may even appear larger at first due to inflammation caused by immune cells attacking cancer—this is called pseudoprogression and does not mean the treatment is failing.
Patients may also notice improved energy levels and reduced symptoms, such as less pain, better breathing (for lung cancer patients), or fewer cancer-related complications. Blood tests may show changes in tumor markers or an increase in immune activity, suggesting that the body is mounting a stronger response against the disease. Doctors track progress through regular imaging scans and blood tests. If a patient’s cancer is shrinking or staying under control, treatment usually continues. If there is significant tumor growth or worsening symptoms, doctors may consider adjusting the approach.
Since immunotherapy works by strengthening the immune system, some side effects, like mild inflammation or flu-like symptoms, can actually be a sign that the immune system is responding. However, severe side effects should always be reported to a doctor. Because every patient responds differently, monitoring and patience are key. Even if changes are not immediate, long-term benefits are possible, and many patients experience lasting responses after successful treatment.
Side effects of Immunotherapy
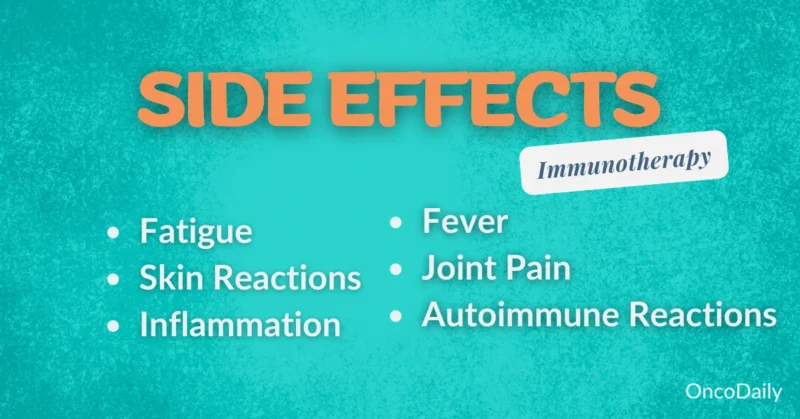
Immunotherapy can result in a range of side effects that vary in severity. While some side effects are common and generally manageable, others can be serious and require close monitoring.
Common and Serious Side Effects
Most patients experience mild to moderate side effects, which are usually manageable. The most common ones include:
- Fatigue – Feeling unusually tired is one of the most reported side effects, as the immune system becomes more active.
- Skin Rash and Itching – Some patients develop skin irritation or a rash, which can be mild or, in rare cases, severe.
- Diarrhea or Nausea – Some forms of immunotherapy can cause digestive issues, though these are usually mild.
- Flu-like Symptoms – Fever, chills, body aches, or headaches may occur as the immune system responds to treatment.
Serious Side Effects (Immune-Related Reactions)
Since immunotherapy boosts the immune system, in some cases, it may become too active and attack healthy organs. These are called immune-related adverse events (irAEs) and can affect different parts of the body:
- Lungs (Pneumonitis) – Inflammation of the lungs can cause cough, shortness of breath, or chest pain. If untreated, it can become serious.
- Colon (Colitis) – Severe diarrhea, abdominal pain, or blood in the stool can be a sign of inflammation in the digestive tract.
- Liver (Hepatitis) – Some patients develop liver inflammation, which may not have symptoms but can be detected through blood tests.
- Endocrine System (Thyroid or Adrenal Issues) – The immune system can attack glands that regulate hormones, leading to fatigue, weight changes, or dizziness.
- Nervous System – In rare cases, patients may experience muscle weakness, vision problems, or nerve pain.
What to Expect During Treatment
tarting immunotherapy can feel overwhelming, but understanding the treatment process can help patients feel more prepared. Immunotherapy is usually given in a hospital or cancer treatment center, and most patients receive it as an outpatient procedure, meaning they do not need to stay overnight.
- Before Treatment Begins: Before starting immunotherapy, patients undergo blood tests, imaging scans, and sometimes biomarker testing to ensure the treatment is appropriate for their cancer type. Doctors also discuss possible side effects and how to manage them.
- During the Infusion: Most immunotherapy drugs are given through an intravenous (IV) infusion, which delivers the medication directly into the bloodstream. Each session usually lasts 30 minutes to a few hours, depending on the specific drug. Patients sit in a comfortable chair while being monitored by nurses for any immediate reactions. Some people bring books, listen to music, or nap during their treatment.
- How Often Will Treatment Be Given: The frequency of immunotherapy depends on the drug and treatment plan. Some patients receive infusions every 2 to 6 weeks, while others may follow a different schedule. The length of treatment varies—some continue for several months or even years if the therapy remains effective and well-tolerated.
- Monitoring Progress: Doctors track progress using imaging scans (CT, MRI, or PET scans) and blood tests every few months. Unlike chemotherapy, which often shows quick tumor shrinkage, immunotherapy can take longer to work because it activates the immune system over time.
- Managing Side Effects: Mild side effects like fatigue, rash, or flu-like symptoms are common and usually manageable. However, serious side effects, such as immune-related inflammation in organs (lungs, liver, intestines, or endocrine glands), require close monitoring. Patients should report any new or worsening symptoms to their doctor immediately.
- What Happens If Treatment Stops Working: If scans show that cancer is still growing or if side effects become too severe, doctors may adjust the treatment plan. This could mean switching to a different immunotherapy drug, combining it with other treatments like chemotherapy, or exploring clinical trials for new options.
Cost, Insurance, and Financial Assistance
Immunotherapy can be expensive, with costs depending on the specific drug, treatment duration, and location. For example, pembrolizumab (Keytruda) costs around $11,000–$15,000 per dose, while CAR T-cell therapy can exceed $400,000 for a full course of treatment. These prices can be overwhelming, but insurance and financial assistance programs can help.Most private insurance plans, as well as Medicare and Medicaid, cover FDA-approved immunotherapies, but co-pays and out-of-pocket costs can still be high. Some patients may need to go through pre-authorization or appeal coverage denials.
For those struggling with costs, financial assistance programs are available. Pharmaceutical companies like Merck (Keytruda) and Bristol-Myers Squibb (Opdivo) offer co-pay assistance or free medication for eligible patients. Nonprofit organizations like the Cancer Financial Assistance Coalition and Patient Advocate Foundation also provide grants to help cover treatment expenses.Patients should discuss costs with their doctors and insurance providers early in the treatment process to explore coverage options and financial aid programs. Many hospitals also have oncology financial counselors who can help navigate available resources.
Lifestyle and Immune System Support During Treatment
Maintaining a healthy lifestyle during immunotherapy can help strengthen the immune system and manage side effects. Eating a balanced diet with plenty of fruits, vegetables, and lean proteins provides essential nutrients, while staying hydrated supports overall health. Gentle exercise like walking or yoga can reduce fatigue and stress, but it’s important to listen to your body and rest when needed.
Managing stress through meditation, deep breathing, or support groups can also improve emotional well-being.Getting enough sleep (7-9 hours per night) helps the body heal, and practicing good hygiene—such as frequent handwashing and avoiding sick individuals—can lower infection risks. These small but effective habits can boost immunity, improve energy, and enhance overall treatment success.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What is immunotherapy for cancer?
Immunotherapy is a treatment that helps the immune system recognize and attack cancer cells. It works by boosting the body’s natural defenses to fight cancer.
How does immunotherapy differ from chemotherapy?
Unlike chemotherapy, which directly kills cancer cells, immunotherapy trains the immune system to target and destroy cancer cells, often providing long-lasting effects.
What are the different types of immunotherapy?
The main types include checkpoint inhibitors, CAR T-cell therapy, monoclonal antibodies, cancer vaccines, and oncolytic virus therapy.
Who is eligible for immunotherapy?
Eligibility depends on cancer type, biomarkers like PD-L1, tumor mutation burden, and overall health. Some patients may qualify for clinical trials if standard options don’t apply.
How do doctors know if immunotherapy is working?
Doctors monitor tumor shrinkage or stability using imaging scans and blood tests. Some side effects, like inflammation, may also indicate an immune response.
What are the common side effects of immunotherapy?
Common side effects include fatigue, skin rashes, flu-like symptoms, nausea, and diarrhea. More serious side effects may involve the lungs, liver, or endocrine system.
How long does immunotherapy treatment last?
Treatment duration varies. Some patients receive immunotherapy for months or years, depending on their response and tolerance to the therapy.
Is immunotherapy expensive, and is it covered by insurance?
Immunotherapy can be costly, with some treatments exceeding $10,000 per dose. Many insurance plans cover FDA-approved immunotherapies, and financial assistance programs are available.
What should patients expect during immunotherapy treatment?
Most immunotherapy is given through IV infusions at a hospital or clinic. Sessions can last from 30 minutes to a few hours, with ongoing monitoring for side effects.
Can lifestyle changes help improve immunotherapy results?
Yes, a healthy diet, staying hydrated, regular exercise, stress management, and good sleep can support the immune system and improve overall treatment outcomes.