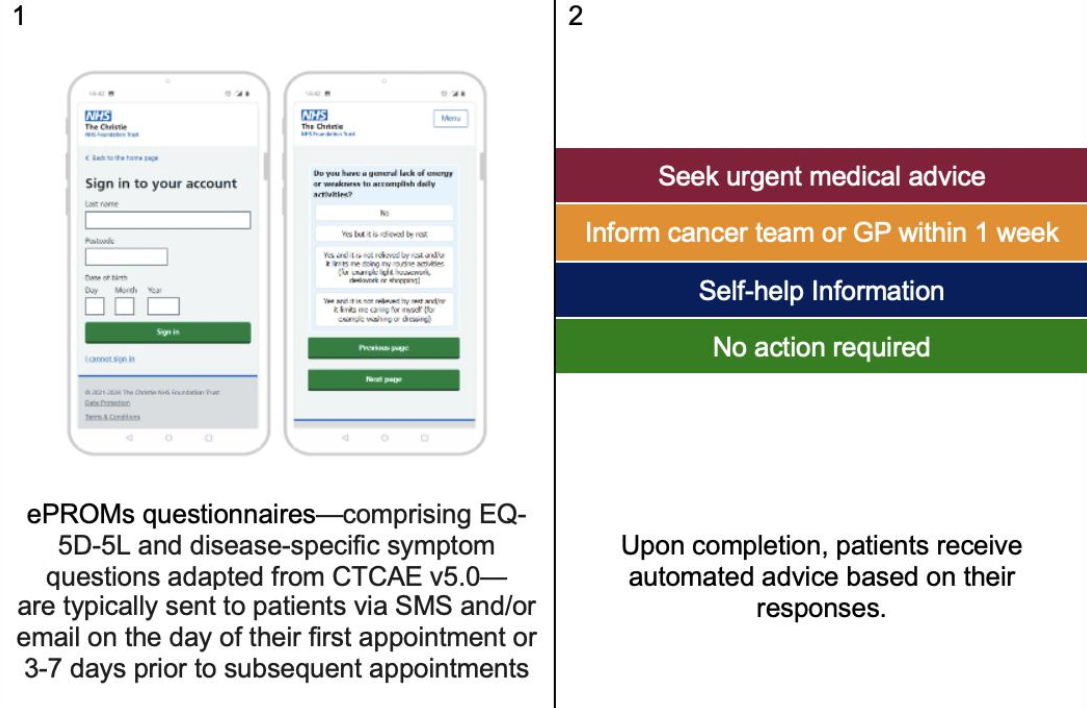
Electronic patient-reported outcome measures (ePROMs) are transforming the way cancer care is delivered by enabling patients to report symptoms, treatment side effects, and quality-of-life concerns remotely and in real time. These digital tools have been associated with earlier detection of clinical deterioration, better symptom management, and improved communication between patients and care teams. In oncology, where treatment regimens can be complex and toxicities highly variable, ePROMs offer an opportunity to center the patient’s voice in decision-making and personalize care.
Despite growing adoption, especially in high-income healthcare systems, there is still limited large-scale real-world data on how patients experience ePROMs in routine clinical practice. Understanding patient perspectives is essential to guide effective implementation, ensure usability, and maximize engagement.
To address this need, researchers from The Christie NHS Foundation Trust (United Kingdom) and partner institutions in Hong Kong conducted a comprehensive evaluation of patient-reported experiences with MyChristie-MyHealth, a digital ePROMs platform embedded in routine cancer services. The findings, presented at the MASCC 2025 Annual Meeting, provide new insights into the acceptability and perceived value of ePROMs across six major cancer types, offering one of the largest real-world assessments of ePROMs from the patient’s perspective to date.
Background
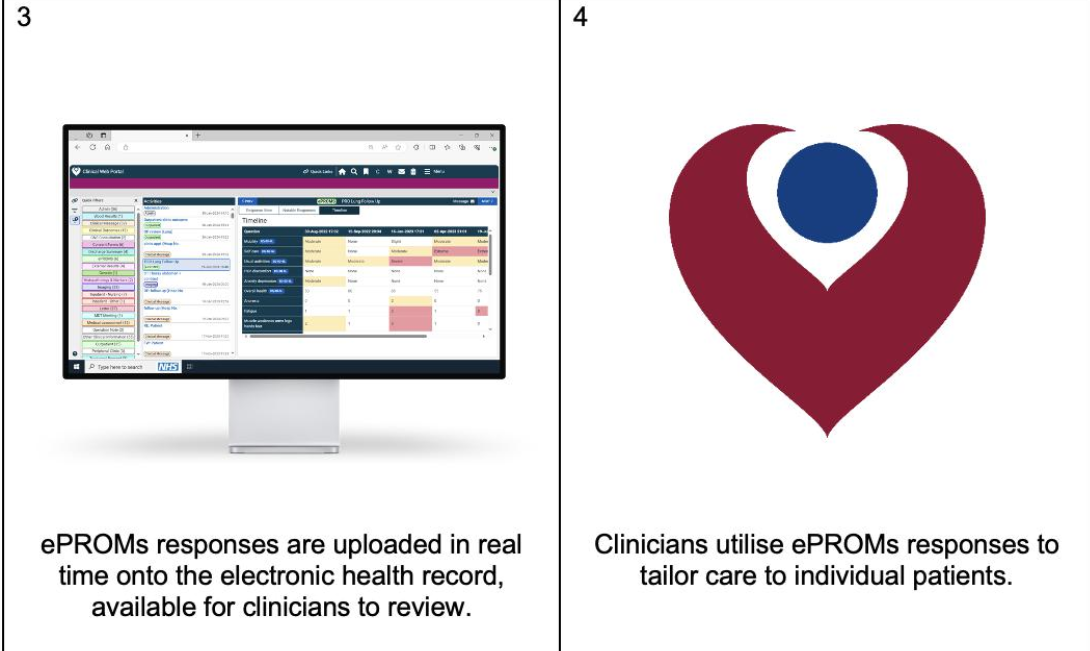
The integration of electronic patient-reported outcome measures (ePROMs) into routine cancer care has gained significant traction in recent years. These tools enable patients to report symptoms, treatment side effects, and overall wellbeing remotely—helping clinicians monitor patient health more accurately between visits. Prior research has shown that ePROMs can improve symptom control, enhance patient-provider communication, and in some cases, even extend survival. However, there remains a critical need to evaluate how patients themselves experience and perceive ePROMs in real-world oncology settings.
To address this gap, researchers from the United Kingdom and Hong Kong evaluated patient satisfaction with MyChristie-MyHealth, a digital ePROMs platform implemented at The Christie NHS Foundation Trust. Since its launch in 2019, the platform has been embedded in over 30 cancer services, with more than 70,000 forms completed by December 2024. This large-scale evaluation, presented at MASCC 2025, provides valuable patient-centered data on the acceptability and usability of ePROMs across multiple tumor types.
Study Design and Methods
The research team conducted a cross-sectional analysis of patient-reported experience using ePROMs. Eligible participants were cancer patients who had submitted at least one ePROM through the MyChristie-MyHealth platform within the past six months. Six key services were selected based on user volume and diversity of treatment pathways:
- Lung cancer
- Head and neck cancer
- Prostate cancer (hormonal therapy)
- Breast cancer (abemaciclib)
- Colorectal cancer (surgery)
- Renal cancer (immunotherapy or tyrosine kinase inhibitors)
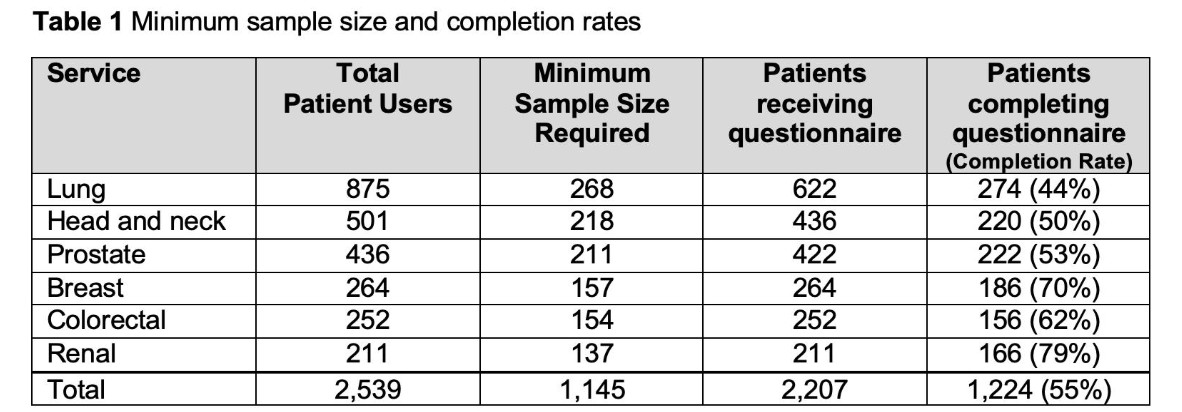
To ensure statistically meaningful results, the minimum sample size per service was calculated using the formula described by WW Daniel (1999), based on a 95% confidence level and 5% margin of error. Assuming a 50% response rate, questionnaires were sent to double the required sample size for each cancer service. Invitations to complete a digital patient experience survey were sent via SMS to a randomly selected cohort of users.
Key Results
A total of 2,207 patients were contacted across the six cancer services. From this group, 1,224 patients returned completed questionnaires, surpassing the required sample size for each service. The final response rate reflected high engagement from a diverse patient population.
- Lung, head and neck, and breast cancer services achieved some of the highest participation rates.
- The feedback covered a range of domains including ease of use, symptom communication, engagement, and perceived value of the ePROMs platform.
- All services met or exceeded the target number of completed surveys to ensure statistically valid comparisons.
Key Findings
The study revealed high satisfaction levels across all tumor types and treatment groups:
- Patients reported that ePROMs helped them feel more in control of their care and enabled earlier communication of symptoms.
- Many users found the interface user-friendly and accessible, even those unfamiliar with digital tools.
- Patients valued the opportunity to reflect on their symptoms before clinical visits, leading to more productive discussions with healthcare providers.
- There was a consistent perception that the system contributed to personalized and timely care, particularly among patients on complex or long-term treatment regimens.
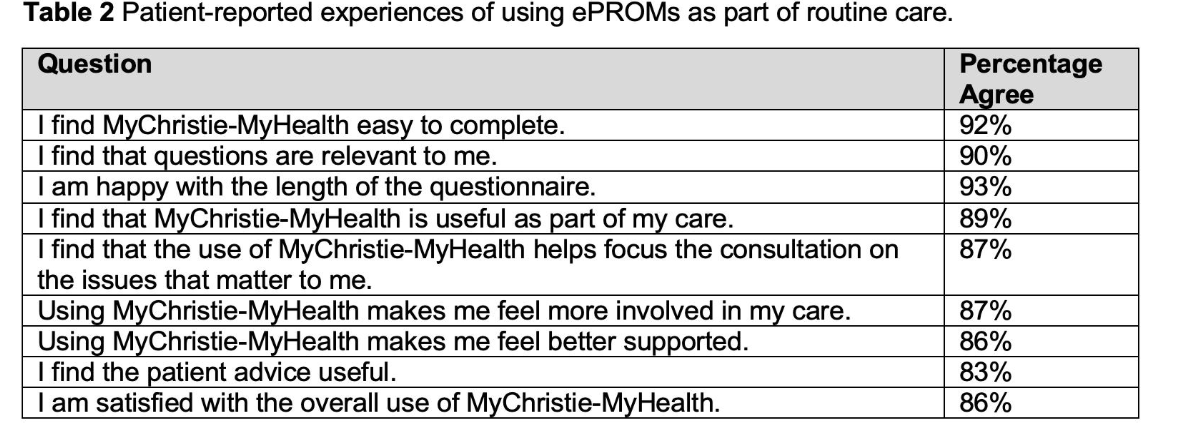 These results affirm the feasibility and patient acceptability of implementing ePROMs across diverse real-world oncology settings. The authors emphasized that the strong patient-reported experience supports ongoing and expanded integration of ePROMs in cancer care pathways.
These results affirm the feasibility and patient acceptability of implementing ePROMs across diverse real-world oncology settings. The authors emphasized that the strong patient-reported experience supports ongoing and expanded integration of ePROMs in cancer care pathways.
Future work will involve qualitative interviews to gain deeper insights into user experience and clinician feedback to explore how ePROMs impact workflow, triage, and treatment decisions.
Conclusions
This large, multicenter evaluation adds to growing global evidence that ePROMs are not only feasible to implement but are also highly valued by cancer patients. The findings presented at MASCC 2025 suggest that digital health solutions like MyChristie-MyHealth can enhance communication, empower patients, and support high-quality, individualized care—marking a critical step toward more person-centered oncology.