Testicular cancer is a relatively rare malignancy, but it holds a unique position in oncology due to its high curability and increasing incidence in young men. Unlike many other cancers that predominantly affect older adults, testicular cancer most commonly strikes men between the ages of 15 and 35. Although it accounts for only about 1% of all male cancers, it remains the most frequently diagnosed solid tumor in this age group, according to the American Cancer Society.
What Are the Symptoms of Testicular Cancer
Early detection is critical for successful treatment, as testicular cancer has one of the highest cure rates among solid tumors. Despite its high treatability, many cases are diagnosed late due to a lack of awareness regarding its early symptoms. Understanding the clinical manifestations of testicular cancer can facilitate timely diagnosis and improve outcomes.
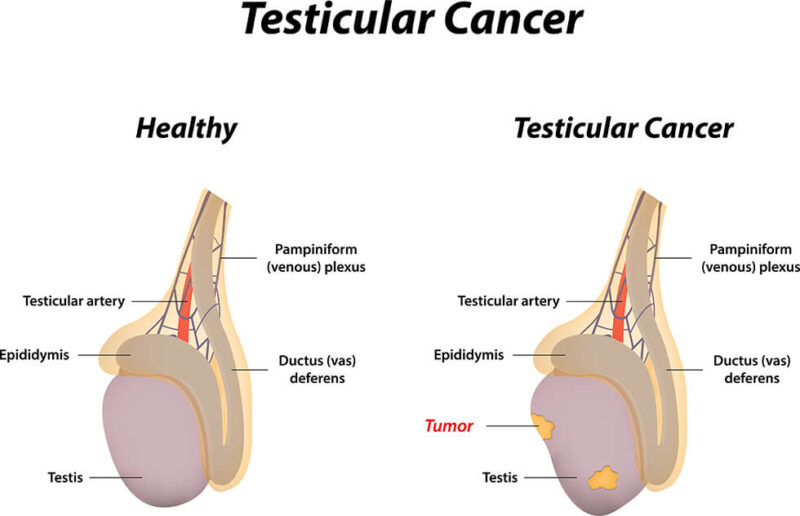
- Testicular lump or mass – Often the first noticeable sign, a firm or hard nodule within the testicle is present in more than 90% of cases. It is usually painless, which may lead to delayed diagnosis (according to the American Cancer Society ).
- Scrotal swelling or enlargement – The affected testicle may increase in size, or there may be a gradual buildup of fluid in the scrotum (hydrocele).
- Heaviness in the scrotum – Some patients report a sensation of fullness or dragging in the lower abdomen or scrotum.
- Dull pain or discomfort in the testicle, scrotum, or groin – Though testicular cancer is often painless, some individuals experience mild, persistent aching or discomfort in the affected area.
In some cases, testicular cancer may present with systemic or distant symptoms, especially if the disease has progressed beyond the testicle. These include:
- Sudden onset of scrotal fluid accumulation – A rapid increase in scrotal size due to a hydrocele or hematocele may occur.
- Gynecomastia (breast enlargement or tenderness) – Certain types of testicular tumors, such as Leydig cell tumors, produce excess estrogen or human chorionic gonadotropin (hCG), leading to breast tissue growth.
- Lower back pain – A sign of retroperitoneal lymph node involvement, which may indicate advanced disease.
- Abdominal pain or mass – Testicular cancer can metastasize to abdominal lymph nodes, causing discomfort or a palpable mass.
- Shortness of breath, chest pain, or cough – Pulmonary metastases can cause respiratory symptoms in advanced-stage disease.
- Neurological symptoms (headache, dizziness, or seizures) – Rarely, testicular cancer spreads to the brain, leading to neurological complications.
Some patients may present with symptoms due to hormonal or metabolic effects of the tumor rather than direct tumor growth. These include:
- Hyperthyroidism-like symptoms (weight loss, palpitations, heat intolerance) – Due to high hCG levels, which can mimic thyroid-stimulating hormone (TSH) activity.
- Deep vein thrombosis (DVT) or pulmonary embolism (PE) – Testicular cancer has a strong association with venous thromboembolism (VTE), sometimes preceding the cancer diagnosis.
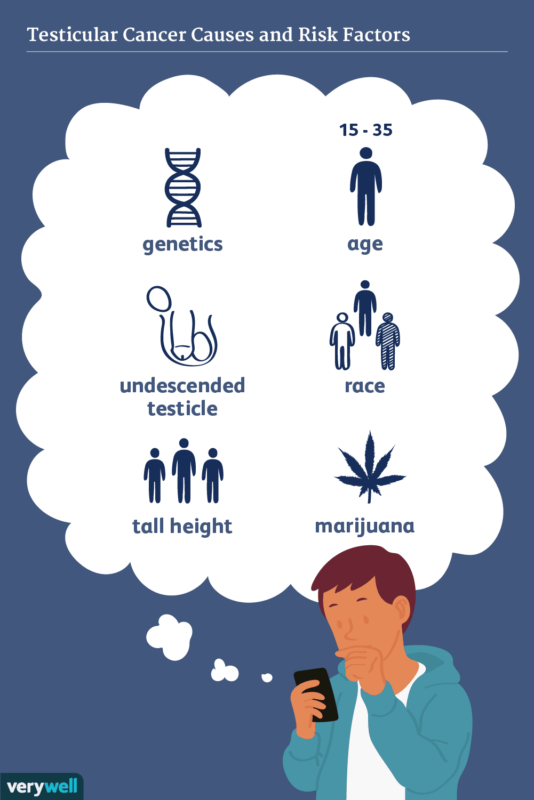
What Causes Testicular Cancer
The exact cause of testicular cancer remains unclear, but researchers have identified several key risk factors that may contribute to its development.
- Klinefelter Syndrome: Klinefelter syndrome (47,XXY) is a genetic condition where males have an extra X chromosome. This condition leads to hormonal imbalances and can increase the risk of testicular cancer. Men with Klinefelter syndrome tend to have smaller testes, lower testosterone levels, and an increased risk of developing germ cell tumors, which are the most common type of testicular cancer.
- Cryptorchidism (Undescended Testes): Men with a history of cryptorchidism, where one or both testes fail to descend into the scrotum during fetal development, are at an increased risk of testicular cancer. Even if the condition is corrected surgically, the risk remains elevated, though the exact cause of the association is still being studied. This is considered a risk factor, especially for seminoma (a type of testicular cancer).
- Family History and Hereditary Risk: A family history of testicular cancer significantly increases an individual’s risk. Men with a father or brother who has had testicular cancer are more likely to develop the disease themselves. Certain genetic mutations may be passed down through families that predispose them to developing testicular cancer, though the exact genetic causes are not fully understood.
Recent research has identified key genetic mutations associated with testicular cancer risk. Genome-wide association studies (GWAS) have highlighted DNA variations in regions linked to cancer susceptibility, including mutations in the DAZL gene, which plays a role in sperm development. Additionally, inherited mutations in genes like WT1—important for cell differentiation—suggest that genetic predisposition plays a larger role than previously thought. Somatic mutations, such as alterations in the KIT gene (common in seminomas) and BRAF mutations, have also been identified. These findings provide insight into tumor development and potential targeted therapies for improved treatment (according to the Testicular Cancer Consortium (TECAC).
Genetic testing is increasingly used to identify individuals at higher risk, particularly those with a family history of testicular cancer. BRCA1 and BRCA2 mutations, known for their link to breast and ovarian cancer, have also been associated with increased risk in men.Prenatal factors, such as cryptorchidism (undescended testicles), are now better understood, allowing for earlier intervention. Emerging liquid biopsy techniques, analyzing blood or urine for cancer markers, are being developed for early detection, potentially improving outcomes by diagnosing cancer at its earliest stages.
Environmental and Lifestyle Risk Factors
Testicular cancer risk is influenced by a combination of genetic, environmental, and lifestyle factors. Exposure to harmful chemicals such as pesticides, herbicides, polychlorinated biphenyls (PCBs), and heavy metals like lead, cadmium, and mercury has been associated with an increased likelihood of developing testicular cancer. These substances, often found in agricultural and industrial settings, may disrupt hormone levels and interfere with normal testicular development. While PCBs have been banned, their persistence in the environment continues to raise concerns.
Additionally, smoking is a well-established risk factor, particularly for non-seminomatous germ cell tumors. Carcinogens in tobacco smoke can damage DNA in testicular cells, and even exposure to secondhand smoke may contribute to an elevated risk, especially in younger individuals who are more susceptible to environmental toxins. Dietary habits and body weight also play a significant role in testicular cancer risk. Diets high in saturated fats, especially from animal sources, can influence hormone levels and may contribute to cancer development, while a low intake of fruits and vegetables deprives the body of antioxidants that protect against oxidative stress and inflammation.
Obesity, particularly during adolescence, is another emerging risk factor, as excess body fat can disrupt hormonal balance and create an environment that promotes tumor growth. While ongoing research continues to refine our understanding of these risk factors, maintaining a healthy diet, avoiding exposure to harmful chemicals, and eliminating tobacco use may help reduce the risk of developing testicular cancer.
What Are Types of Testicular Cancer
Testicular cancer is classified based on the type of cells it originates from, primarily affecting germ cells, which are responsible for producing sperm. The two main categories are.
Seminomas
Slow-growing and highly responsive to treatment. They account for approximately 50% of testicular cancer cases ( according to the American Cancer Society ). Seminomas generally grow more slowly and tend to be confined to the testicle initially. They are more sensitive to radiation and chemotherapy, leading to a favorable response to treatment.
Treatment typically involves orchiectomy (surgical removal of the affected testicle), followed by radiation therapy if localized, or chemotherapy if the cancer has spread. The prognosis for seminomas is excellent, with survival rates exceeding 95% when diagnosed at an early stage, according to the American Cancer Society. Even in advanced stages, the survival rate remains high due to effective treatment options.
Non-Seminomas
Non-seminomas represent about 40% of testicular cancer cases and include subtypes like embryonal carcinoma, yolk sac tumors, choriocarcinoma, and teratomas. Non-seminomas tend to grow more rapidly and are more likely to spread to lymph nodes and other organs compared to seminomas. They are less responsive to radiation but are treatable with chemotherapy. Like seminomas, treatment starts with orchiectomy. However, non-seminomas often require chemotherapy due to their more aggressive nature.
Retroperitoneal lymph node dissection (RPLND) may also be needed in some cases. The prognosis for non-seminomas is generally favorable, especially in early stages. Survival rates are 90% or higher for localized cases, but survival rates for advanced cases can vary depending on the extent of spread and response to chemotherapy, according to the American Cancer Society ).
Seminoma vs Non-Seminoma: Key Differences and Similarities
Each with distinct growth patterns, treatment responses, and prognoses. Understanding these differences is crucial for selecting the most effective treatment approach.
- Age Group – Seminomas are more common in men aged 30-40, whereas non-seminomas typically affect younger men, usually between teens and early 30s.
- Growth Rate and Spread – Seminomas tend to grow slowly and remain localized longer, whereas non-seminomas are faster-growing and more likely to spread to other organs.
- Tumor Markers – While seminomas may elevate hCG levels, they never produce AFP. Non-seminomas, on the other hand, can elevate both AFP and hCG
- Response to Treatment – Seminomas respond well to radiation and chemotherapy, while non-seminomas are primarily treated with surgery and chemotherapy since radiation is less effective.
- Subtypes – Seminomas exist as a single type, while non-seminomas include embryonal carcinoma, yolk sac tumor, choriocarcinoma, teratoma, or mixed forms.
Both arise from germ cells in the testicles. Symptoms are similar, often presenting as a painless lump or swelling in the testicle. Diagnosis involves ultrasound, blood tests (AFP, hCG, LDH), and orchiectomy (testicle removal). Both have excellent cure rates, with early-stage cases exceeding 95% survival (according to American Cancer Society).
What are the Stages of Testicular Cancer?
Testicular cancer is categorized into different stages based on tumor size, lymph node involvement, and metastasis. Staging helps determine the extent of the disease and guides treatment decisions. The American Joint Committee on Cancer (AJCC) Tumor-Node-Metastasis (TNM) system is commonly used, classifying testicular cancer into the following stages:
- Stage 0 (Carcinoma in situ) – Abnormal cells in the testicle but no invasive growth.
- Stage I – Cancer is confined to the testicle.
- Stage II – Cancer has spread to regional lymph nodes.
- Stage III – Cancer has metastasized to distant organs (lungs, liver, brain).
How is Testicular Cancer Diagnosed
If testicular cancer is suspected, doctors use a combination of imaging, blood tests, and pathology examinations to confirm the diagnosis. Blood tests check for tumor markers, substances produced by cancer cells
- Alpha-fetoprotein (AFP) – Elevated in non-seminomas, but not in pure seminomas.
- Human chorionic gonadotropin (HCG) – Elevated in both seminomas and non-seminomas.
- Lactate dehydrogenase (LDH) – Less specific but useful for monitoring disease burden.
Ultrasound-Primary imaging tool to differentiate solid tumors (likely cancerous) from cystic or fluid-filled masses (usually benign). Accuracy: 90-95% in distinguishing between cancerous and benign testicular masses( according to American Cancer Society ). CT, PET-CT and MRI Scans-Used to determine if cancer has spread to the lymph nodes, lungs, or other organs.
What Are the Treatment Options for Testicular Cancer
Testicular cancer is highly treatable, and treatment plans typically involve a combination of surgery, radiation therapy, and chemotherapy. The choice of treatment depends on the type and stage of the cancer.
Surgical treatment
The first line of treatment for testicular cancer is usually orchiectomy, the removal of the affected testicle. It is typically performed under general anesthesia, and it is a critical step in diagnosing and staging the cancer. If cancer is confined to the testicle, further treatments like radiation or chemotherapy may not be necessary.
- Side Effects:Short-term swelling and discomfort and hormonal imbalances (in cases where both testicles are affected, leading to testosterone deficiencies).
- Recovery Time:Most patients can return to normal activities within 1-2 weeks post-surgery, depending on individual recovery.
Radiation Therapy
Radiation therapy is primarily used for seminomas, either after surgery to destroy any remaining cancer cells or to treat cancer that has spread to nearby lymph nodes.
Technological Advancements:Newer techniques like Intensity-Modulated Radiation Therapy (IMRT) have greatly reduced side effects. IMRT allows for more precise targeting of cancer cells, minimizing damage to surrounding healthy tissue. This helps reduce side effects like fatigue, skin irritation, and gastrointestinal distress.
- Side Effects:Skin irritation and redness in the treated area and fatigue and potential long-term risk of secondary cancers, though this is rare with modern techniques.
- Recovery Time:Radiation therapy typically requires daily treatment sessions over 2-3 weeks. Most side effects are manageable and improve after treatment ends.
Chemotherapy
Chemotherapy is commonly used for non-seminomas or when cancer has spread beyond the testicle. Common chemotherapy drugs for testicular cancer include bleomycin, etoposide, and cisplatin. These drugs are often given in combination, such as the BEP regimen (bleomycin, etoposide, and cisplatin). Typical chemotherapy regimen is BEP (Bleomycin, Etoposide, Cisplatin): Usually administered over a 3-week cycle, and this may be repeated for 3-4 cycles, depending on the stage of cancer and the patient’s response.
Common side effects are nausea and vomiting (commonly managed with anti-nausea medications), neuropathy (numbness or tingling in hands/feet),fatigue (can last for weeks or months after treatment),hair loss (temporary), increased risk of infections (due to lowered white blood cell count). Strategies for managing side effects are anti-nausea medications (e.g., ondansetron) taken before and after chemotherapy sessions can help manage nausea, regular exercise, physical therapy, and medications like gabapentin can help alleviate neuropathy symptoms, prioritizing rest, and following a balanced diet. Energy levels may improve several weeks after the completion of chemotherapy. Chemotherapy typically requires 3-4 cycles, each lasting 3 weeks. Recovery time varies, but most patients experience a gradual return to normal energy levels within a few months post-treatment.
Testicular cancer has high curability, especially when caught early. Surgery, radiation therapy, and chemotherapy are the primary treatments used to fight the disease, each with its own set of benefits and side effects. Advances in radiation technology like IMRT and modern chemotherapy regimens have greatly improved treatment effectiveness while reducing side effects.
Newest Options and Ongoing Trials
Recent advancements in immunotherapy and targeted therapies offer new hope for patients with testicular cancer, particularly for those with advanced or recurrent disease.
- Immunotherapy: Researchers are investigating the efficacy of immune checkpoint inhibitors,such as pembrolizumab and nivolumab, in treating advanced or refractory testicular cancer. These agents aim to enhance the body’s immune response against cancer cells
- Targeted Treatments: Research is focusing on therapies that target specific genetic mutations involved in the cancer’s growth.
- High-Dose Chemotherapy with Stem Cell Transplantation: For patients with relapsed or refractory testicular cancer, high-dose chemotherapy followed by autologous stem cell transplantation has shown promise. A study from Indiana University reported a 60% cure rate using this approach.
- Bispecific Antibodies: Researchers are investigating bispecific antibodies that target CLDN6 and CD3 to enhance T-cell activation against cancer cells. Agents like XmAb541 and SAIL66 are among those in development.
- Antibody-Drug Conjugates (ADCs): ADCs such as TORL-1-23 and DS-9606a are designed to deliver cytotoxic drugs directly to CLDN6-expressing tumors .
- mRNA-Encoded Bispecific Antibodies: Another approach involves mRNA-based therapeutics, such as BNT142, which encodes an anti-CD3/anti-CLDN6 bispecific antibody to stimulate immune responses against cancer.
- CAR-T Therapy: CLDN6-targeted CAR-T cells are also being explored as a novel immunotherapy approach, potentially improving treatment outcomes for solid tumors expressing this protein.
What is the Prognosis of Testicular Cancer
Testicular cancer is highly treatable and has a strong prognosis, especially with early detection. The survival rate varies based on the stage of cancer and whether it’s a seminoma or non-seminoma.
Several factors affect the prognosis of testicular cancer beyond just the stage, including tumor markers such as alpha-fetoprotein (AFP), lactate dehydrogenase(LDH) and human chorionic gonadotropin (hCG), which are often elevated in testicular cancer and are critical for determining prognosis. If AFP levels are elevated, it often indicates a non-seminoma of cancer, which may require more aggressive treatment. hCG levels: Elevated hCG is often found in both seminomas and non-seminomas and can help guide treatment decisions. Recurrence of testicular cancer is possible, but regular follow-up care and monitoring of tumor markers help detect recurrences early. For example:I ncreased AFP or hCG levels after treatment may signal a recurrence, prompting further investigation and intervention.
Survival Rates for Testicular Cancer
Testicular cancer is one of the most treatable cancers, with a high survival rate even in advanced stages. The prognosis depends on several factors, including the type of cancer (seminoma or non-seminoma), stage at diagnosis, and response to treatment. Early-stage testicular cancer has a particularly high cure rate, while more advanced stages may require aggressive treatments such as chemotherapy and surgery. Below is an overview of survival rates by stage, based on data from the American Cancer Society (ACS) and other cancer research organizations
- Stage 0 (In Situ)-Seminomas diagnosed at stage 0 (in situ) have near 100% survival rates. Treatment generally involves surveillance or localized radiation therapy, leading to excellent outcomes.Non-Seminomas: Stage 0 non-seminomas are rare, but when detected early, survival rates are similar to seminomas, often near 100%( according to American Cancer Society ).
- Stage I (Localized)– When seminomas are confined to the testicle (Stage I), the survival rate is 98-99% with surgery (orchiectomy) and often radiation therapy for localized cases. The survival rate for Stage I non-seminomas is similarly high, around 95-98%, with surgery (orchiectomy) and, in some cases, follow-up chemotherapy( according to American Cancer Society ).
- Stage II (Regional Spread to Lymph Nodes)– In Stage II seminomas, the survival rate is 95-98%, with chemotherapy (if necessary) and/or radiation treatment. The prognosis remains excellent due to the responsiveness to these therapies. Stage II non-seminomas have a slightly lower survival rate compared to seminomas, around 90-95%. They may require chemotherapy, and if lymph nodes are involved, surgery (RPLND) may be needed( according to American Cancer Society ).
- Stage III (Distant Metastasis)– The survival rate for Stage III seminomas, where cancer has spread to distant organs, is around 85-90%. With aggressive chemotherapy regimens, including high-dose treatments and stem cell transplants when necessary, outcomes remain favorable.Non-Seminomas: Stage III non-seminomas, which tend to spread more rapidly, have a survival rate of around 80-85%. Despite being more aggressive, these cancers are often treatable with advanced chemotherapy, and survival rates improve significantly with early intervention( according to American Cancer Society ).
Seminomas are typically less aggressive and more responsive to radiation, leading to better outcomes, particularly in early stages. Their survival rates remain high even in later stages, largely due to the effectiveness of treatments like chemotherapy and radiation therapy.Non-Seminomas are more aggressive and less sensitive to radiation. Their treatment often involves a combination of chemotherapy and surgery (RPLND) to address metastasis. Although the survival rates for non-seminomas are slightly lower than seminomas, early detection and advanced chemotherapy have significantly improved outcomes.
| Stage | Five-Year Survival Rate |
| Stage I | 99% |
| Stage II | 96% |
| Stage III | 73% |
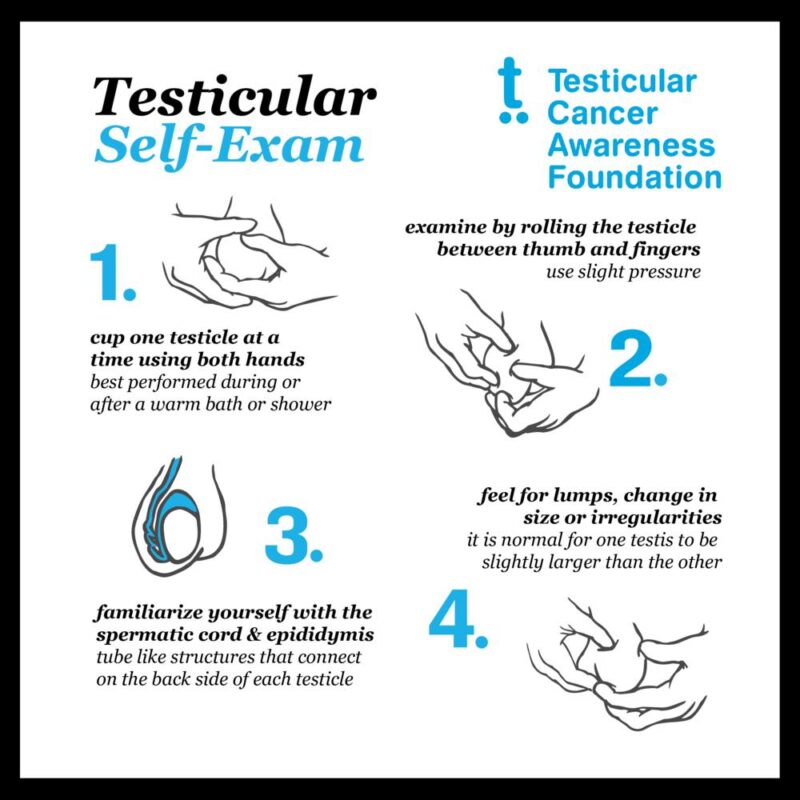
How to Perform a Testicular Self-Exam
Testicular self-exams are a simple and effective way to detect early signs of testicular cancer or other health issues. Here’s how you can perform one safely and efficiently:
- Best time – Perform the exam after a warm shower when the scrotum is relaxed.
- Use both hands – Gently roll each testicle between the thumb and fingers, checking for any lumps or abnormalities.
- Look for changes – Pay attention to any size discrepancies, firm areas, or unusual swelling.
- Check the epididymis – The soft, coiled structure at the back of the testicle is normal, but any hard lumps are not.
- Consult a doctor – If you notice any abnormalities, seek medical advice immediately.
Lifestyle Changes
One of the most significant steps individuals can take to reduce their risk of testicular cancer and other cancers is to quit smoking. Avoiding tobacco and secondhand smoke can protect the body from harmful carcinogens and lower the risk of testicular and other cancers. Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce the risk of many cancers, including testicular cancer.
Limiting saturated fats and processed foods can also promote better health and reduce cancer risk. If you work in an environment where you’re exposed to agricultural chemicals, heavy metals, or other toxins, taking protective measures such as wearing proper gear or minimizing exposure can help reduce your risk. For example, using organic products or avoiding excessive pesticide exposure may reduce environmental risks.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD
FAQ
Is Testicular Cancer Curable?
Testicular cancer is one of the most treatable and curable malignancies, even in advanced stages. Advances in surgery, chemotherapy, and radiation therapy have significantly improved outcomes, making testicular cancer a highly manageable condition.
How Often Should You Perform a Testicular Self-Exam?
It’s recommended to perform a testicular self-exam (TSE) once a month. Regular self-exams help detect any changes early, which is crucial for identifying testicular cancer or other conditions at a treatable stage.
What Does Testicular Cancer Feel Like?
Early Signs of testicular cancer are painless lump or swelling in the testicle, feeling of heaviness in the scrotum, dull ache in the lower abdomen or groin, sudden fluid buildup in the scrotum,change in testicle size or firmness (one may become significantly larger or harder than the other).
How to Lower Your Risk of Testicular Cancer?
Regular self-exams help identify any unusual changes early, improving treatment outcomes. Men with risk factors like a family history or undescended testicles should discuss screening options with a doctor. Maintaining a healthy lifestyle—avoiding smoking, limiting chemical exposure, and eating a balanced diet—supports overall well-being.
Can Testicular Cancer Affect Fertility?
Yes, both the cancer itself and treatments like chemotherapy and radiation can impact fertility. Patients are often advised to bank sperm before starting treatment.
What Are the Chances of Survival for Testicular Cancer?
Testicular cancer has one of the highest survival rates, with a 5-year survival rate over 95% when detected early. Even in advanced cases, aggressive treatment often leads to successful outcomes.
Can Testicular Cancer Come Back After Treatment?
Recurrence is possible but uncommon. Regular follow-ups with blood tests and imaging help monitor for any signs of relapse. If it does return, additional treatment options, including chemotherapy and surgery, are available.
Can Testicular Cancer Spread to Other Parts of the Body?
Yes, in advanced stages, it can spread to lymph nodes, lungs, liver, or even the brain. This is why early detection and treatment are crucial for the best prognosis.
What Can Be Done to Prevent Testicular Cancer?
There is no definitive way to prevent testicular cancer, but regular self-examinations can help detect it early. Maintaining a healthy lifestyle and addressing risk factors like undescended testicles (cryptorchidism) may also be beneficial.