Introduction
Testicular cancer is a type of cancer that develops in the testicles, which are part of the male reproductive system. Although it is relatively rare, it is the most common cancer in young men aged 20 to 34. Early detection and treatment are crucial, as testicular cancer is highly treatable, especially when caught early. This article aims to provide patients with a comprehensive understanding of testicular cancer, including its causes, risk factors, subtypes, symptoms, diagnosis, prevention, prognosis, treatment options, and ongoing research.
Causes and Risk Factors
The exact cause of testicular cancer is not known, but several risk factors have been identified that may increase the likelihood of developing the disease. Understanding these risk factors can help individuals be more vigilant about their health.
Age: Testicular cancer is most commonly diagnosed in young and middle-aged men, particularly those between the ages of 20 and 45. However, it can occur at any age, including in teenagers and older men.
Cryptorchidism (Undescended Testicle): Cryptorchidism is a condition where one or both testicles fail to move down into the scrotum before birth. Men with this condition have a higher risk of developing testicular cancer. The risk is higher if the undescended testicle remains in the abdomen rather than descending partially. Surgical correction of this condition, known as orchiopexy, can reduce the risk if performed at a young age.
Family History: Having a close relative, such as a father or brother, with testicular cancer increases the risk of developing the disease. This suggests a genetic component to the risk.
Personal History: Men who have had cancer in one testicle are at an increased risk of developing cancer in the other testicle. Regular follow-up and monitoring are essential for these individuals.
Race and Ethnicity: Testicular cancer is more common in white men compared to men of other races. The reasons for this disparity are not fully understood.
HIV Infection: Men with human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS) have a slightly higher risk of developing testicular cancer, particularly seminoma.
Other Factors: Other potential risk factors include low birth weight, exposure to certain chemicals, and having certain congenital abnormalities such as hypospadias (a birth defect where the urethral opening is not at the tip of the penis).
Subtypes
Testicular cancer is classified into different subtypes based on the type of cells involved. The two main types are germ cell tumors and stromal tumors.
Germ Cell Tumors
- Germ cell tumors are the most common type of testicular cancer, accounting for about 95% of cases. They are further divided into two main subtypes:
Seminomas
- Seminomas tend to grow and spread more slowly than non-seminomas. They are usually diagnosed in men aged 30 to 50. Seminomas can secrete a hormone called human chorionic gonadotropin (HCG), which can be detected through blood tests.
Non-Seminomas
- Non-seminomas are more aggressive and tend to grow and spread more quickly than seminomas. They are usually diagnosed in younger men, typically in their late teens to early 30s. Non-seminomas include several subtypes, such as embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, and teratoma.
Stromal Tumors
- Stromal tumors are rare and account for about 5% of testicular cancer cases. They develop from the supportive tissues around the germ cells in the testicle. The two main types of stromal tumors are:
Leydig Cell Tumors
- Leydig cell tumors develop from cells that produce testosterone. They are usually benign and can be cured with surgery.
Sertoli Cell Tumors
- Sertoli cell tumors develop from cells that support and nourish the developing sperm. These tumors are also usually benign.
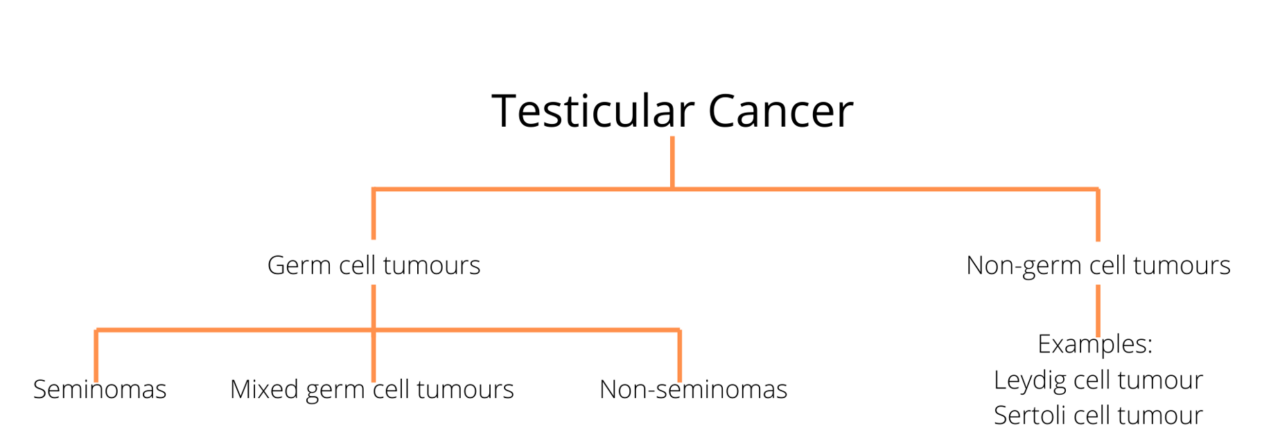
Source of image learnoncology.ca
Symptoms
The symptoms of testicular cancer can vary, but the most common sign is a lump or swelling in the testicle. It is important to be aware of the symptoms and seek medical attention if any changes are noticed.
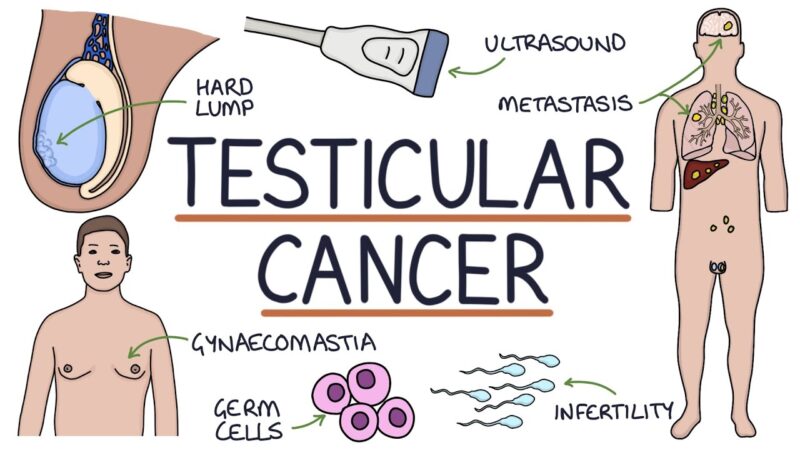
This image is taken from zerotofinals.com
Common Symptoms
- A painless lump or swelling in either testicle
- A feeling of heaviness in the scrotum
- A dull ache in the lower abdomen or groin
- Sudden buildup of fluid in the scrotum
- Pain or discomfort in a testicle or the scrotum
- Change in the way a testicle feels or a feeling of unevenness
- Enlargement or tenderness of the breasts (gynecomastia)
Symptoms of Advanced Testicular Cancer
If testicular cancer has spread to other parts of the body (metastasis), additional symptoms based on location may include:
- Lower back pain
- Shortness of breath, chest pain, or a cough (even coughing up blood)
- Swelling of one or both legs
- Headaches or confusion
Diagnosis
Diagnosing testicular cancer typically involves a combination of physical examinations, imaging tests, and blood tests. Early detection is crucial for effective treatment.
Physical Examination
A physical examination may be performed to check for lumps, swelling, or other abnormalities in the testicles. Abdomen and lymph nodes may be examined to check for signs of cancer spread.
Ultrasound
An ultrasound is often the first imaging test used to evaluate a lump in the testicle. It uses sound waves to create images of the inside of the body and can help determine whether a lump is solid (which may indicate cancer) or fluid-filled (which is usually benign).
Blood Tests
Blood tests can measure levels of certain proteins called tumor markers that are often elevated in men with testicular cancer. These markers include alpha-fetoprotein (AFP), human chorionic gonadotropin (HCG), and lactate dehydrogenase (LDH).
Imaging Tests
Additional imaging tests, such as chest X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) scans, may be performed to determine if the cancer has spread to other parts of the body.
Surgery
If testicular cancer is suspected, the entire testicle may be surgically removed in a procedure called an orchiectomy. The removed testicle is then examined under a microscope to confirm the diagnosis and determine the type and extent of the cancer.
Prevention
While there is no sure way to prevent testicular cancer, certain measures can help reduce the risk and promote early detection.
Regular Self-Examinations
Performing regular self-examinations can help detect testicular cancer early. It is recommended to check the testicles monthly, ideally after a warm bath or shower when the scrotal skin is relaxed. Any lumps, swelling, or changes in size or shape should be reported to a healthcare provider.
Awareness of Risk Factors
Being aware of personal risk factors, such as a family history of testicular cancer or a history of undescended testicles, can help individuals be more vigilant about their health and seek medical advice if needed.
Healthy Lifestyle
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding known risk factors such as smoking, may contribute to overall health and potentially reduce the risk of cancer.
Prognosis
The prognosis for testicular cancer is generally very good, especially when the cancer is detected early. The survival rate for testicular cancer is high, with more than 95% of men surviving at least five years after diagnosis.
Factors Affecting Prognosis
Several factors can influence the prognosis of testicular cancer, including:
- The stage of the cancer at diagnosis
- The type and subtype of the cancer
- The levels of tumor markers in the blood
- The patient’s overall health and response to treatment
Treatment and Side Effects
The treatment of testicular cancer depends on the type and stage of the cancer. Common treatment options include surgery, radiation therapy, and chemotherapy. Each treatment has potential side effects that patients should be aware of.
Surgery
Surgery to remove the affected testicle (orchiectomy) is the primary treatment for most cases of testicular cancer. In some cases, lymph nodes in the abdomen may also be removed (retroperitoneal lymph node dissection).
Side Effects of Surgery
- Pain and discomfort in the surgical area
- Swelling and bruising
- Risk of infection
- Changes in body image and self-esteem
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It is often used to treat seminomas, which are more sensitive to radiation.
Side Effects of Radiation Therapy
- Fatigue
- Skin irritation in the treated area
- Nausea and vomiting
- Diarrhea
- Risk of infertility
Chemotherapy
Chemotherapy uses drugs to kill cancer cells and is often used to treat non-seminomas or advanced testicular cancer. It may be given before or after surgery.
Side Effects of Chemotherapy
- Nausea and vomiting
- Hair loss
- Fatigue
- Increased risk of infections
- Risk of infertility
- Nerve damage (neuropathy)
Newest Options and Ongoing Trials
Research is ongoing to develop new and more effective treatments for testicular cancer. Clinical trials are an important part of this research and may offer patients access to cutting-edge therapies.
Targeted Therapy
- Targeted therapy involves drugs that specifically target cancer cells while sparing normal cells. This approach may reduce side effects compared to traditional chemotherapy.
Immunotherapy
- Immunotherapy uses the body’s immune system to fight cancer. It is being studied as a potential treatment for testicular cancer, particularly for cases that do not respond to standard treatments.
Clinical Trials
- Patients with testicular cancer may consider participating in clinical trials to access new treatments and contribute to the advancement of medical knowledge. Clinical trials are carefully controlled research studies that evaluate the safety and effectiveness of new treatments.
More information about ongoing clinical trials can be found on clinicaltrials.gov
Patient Survivorship
Survivorship refers to the phase of care that follows the completion of cancer treatment. It involves monitoring for recurrence, managing long-term side effects, and addressing the emotional and psychological impact of cancer.
Follow-Up Care
Regular follow-up appointments are essential for monitoring for any signs of recurrence and managing any long-term side effects of treatment. Follow-up care may include physical examinations, blood tests, and imaging tests.
Fertility and Sexual Health
Testicular cancer and its treatment can affect fertility and sexual health. Patients may consider sperm banking before treatment to preserve fertility. It is important to discuss any concerns about sexual health with a healthcare provider.
Emotional and Psychological Support
A diagnosis of testicular cancer can be emotionally challenging. Support from family, friends, and healthcare professionals is important. Counseling and support groups can also provide valuable emotional support.
Healthy Lifestyle
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding known risk factors such as smoking, can contribute to overall health and well-being.
This fascinating video is taken from The Princess Margaret Cancer Foundation
Conclusion
Testicular cancer is a highly treatable disease, especially when detected early. Understanding the risk factors, symptoms, and treatment options can empower patients to take an active role in their health. Regular self-examinations and awareness of personal risk factors are important for early detection. Advances in research and treatment continue to improve outcomes for patients with testicular cancer. Survivorship care is essential for monitoring for recurrence, managing long-term side effects, and addressing the emotional and psychological impact of cancer.
Resources
- Testicular Cancer: Symptoms and Signs – cancer.net
- Testicular Cancer Treatment – cancer.gov
- Testicular Cancer, Information, Resources, Support – cancercare.org
- Testicular Cancer Patient Education and Resources – rogelcancercenter.org
- Testicular cancer resources and support organisations – cancerresearchuk.org
- Testicular Cancer – StatPearls – PubMed
- Testicular Cancer: Pathogenesis, Diagnosis and Management – PubMed
- Advances in Diagnosis and Treatment of Testicular Cancer – PubMed
- Diagnosis and Treatment of Early Stage Testicular Cancer – AUA
- Testicular Cancer: Biology to Bedside – AACR Journals


